Today’s Dietitian
Vol. 18 No. 8 P. 34
Fiber often triggers symptoms in IBS patients, but it’s also a commonly recommended treatment. Here’s how patients can eat a fiber-rich diet without worsening GI distress.
Between 25 and 45 million people in the United States suffer with irritable bowel syndrome (IBS).1 “IBS is a symptom-based condition defined by the presence of abdominal pain and altered bowel habits,” says William Chey, MD, a professor of gastroenterology at the University of Michigan. “Patients may have constipation, diarrhea, or both,” Chey says. The cause of this condition, which affects all age groups, is unknown, but symptoms may be a result of a disturbance in the way the gut, brain, and nervous system interact.1
“IBS is impacted by many factors,” says Torey Armul, MS, RDN, CSSD, a national spokesperson for the Academy of Nutrition and Dietetics, “including genetics, the gut microbiome, the immune system, gut-brain interaction, and diet.” Diet doesn’t cause IBS, but eating may aggravate symptoms as the gut overresponds to the stimulus of food.1
There are no diagnostic tests for IBS, and there’s no universal treatment.1 While a variety of medications are available that target specific symptoms like diarrhea or constipation, dietary changes are a common way to approach managing this condition. “Treatment for IBS is very individualized,” says Emily Haller, RDN, who counsels IBS patients at the University of Michigan Health System’s division of gastroenterology. According to the International Foundation for Functional Gastrointestinal Disorders (IFFGD), there’s no generalized dietary advice for treating IBS. Methods such as food diaries and elimination diets typically are used to identify trigger foods, and it’s recommended that patients avoid known gas-producing foods and attempt to address diarrhea and constipation through diet.1 Since constipation is a very common symptom in IBS, increasing fiber intake seems like a reasonable dietary recommendation. The IFFGD reports that adding fiber may help improve bowel function, especially in IBS with constipation (IBS-C).1
What Kind of Fiber Is Best?
“Fiber tolerance in IBS is very variable,” Haller says. “We know fiber is essential for good health, but as with anything, too much of a good thing can be bad.”
While people have different food triggers, Armul says that fibrous foods are one of the most common. “Fiber can certainly be a trigger for some clients,” Armul says, “but it can also be a great help to others. It varies from person to person.” The trick is that not all fibers are created equal. Some fibers are soluble, some insoluble; some fibers are fermentable, some aren’t. Understanding the difference is key to helping IBS patients find a diet that eases their symptoms.
Soluble vs Insoluble
Soluble fibers are dispersible in water; insoluble fibers are not.2 A review of 17 randomized controlled trials of fiber supplements in IBS patients found that supplementation with insoluble fiber, such as corn or wheat bran, didn’t improve IBS symptoms, but supplementation with soluble fiber, such as psyllium, ispaghula, or calcium polycarbophil, significantly improved symptoms.3 “Fiber creates bulk, but not all fibers are the same,” Chey says. “Insoluble fiber works for constipation by increasing biomass in the stool, and it may even create mechanical stimulation in the bowel, triggering motility. This can help ease constipation, but in people with underlying abnormalities in motor function and overly sensitive gut sensations characteristic of IBS, insoluble fiber can make symptoms worse.” But soluble fiber doesn’t have the same effect, Chey says. “Soluble fiber increases biomass, but not in the same purely mechanical way. It increases the water-holding capacity of the stool, softening it and making passage easier.” So, from a purely mechanical standpoint, insoluble fiber may be more likely to trigger IBS symptoms, while soluble fiber may actually bring some relief, particularly in IBS-C.
“[Several] different studies have shown that soluble fiber benefits constipation and overall symptoms in IBS patients,” Chey says.
Much of this research has looked at the fiber supplement psyllium. “This special kind of soluble fiber has a lot of good research around it,” Armul says. A three-month randomized, placebo-controlled trial of 275 patients with IBS found that supplementation with 10 g psyllium per day improved symptoms of abdominal pain or discomfort in the first two months of supplementation and also improved symptom severity after three months’ supplementation.4
However, getting enough soluble fiber without supplementation can be challenging. “Clients don’t typically understand the difference between the two types of fiber,” Armul says, “and most fibrous foods have both soluble and insoluble.” The soluble fibers (β-glucans, gums, mucilages, and some pectins and hemicelluloses) are commonly found in oats, barley, legumes, fruits (particularly berries), and seeds. The insoluble fiber cellulose is found in all plants, since cellulose is a component of plant cell walls.2 So while legumes and seeds, for example, are good sources of soluble fiber, they also top the list for insoluble cellulose (along with root vegetables, brans, and plants in the cabbage family).1,2 Therefore, increasing dietary soluble fiber also may increase intake of insoluble fiber, which, although it helps with constipation, could mechanically trigger IBS symptoms. And there’s another concern with increasing soluble fiber intake: Soluble fibers are more readily fermented than insoluble fibers, and fermentation in the colon has emerged as a key trigger in IBS.
Fermentable vs Nonfermentable
“Fermentability is a big piece in the IBS puzzle,” Chey says. “When the bacteria in the colon break down fermentable fiber, they produce hydrogen, methane, and carbon dioxide. These gases cause luminal distention, stretching the intestines and colon. This can be uncomfortable for anyone, but particularly so for people with IBS whose bowels can be overly sensitive to a variety of stimuli such as food or stress.” But increased gassiness isn’t the only problem with fermentable fiber in IBS sufferers. “When the bacteria break down the fermentable fiber, they don’t just produce gas; they also create short-chain fatty acids. These acids lower the pH of the colonic environment,” Chey says. “The gut microbiome is highly influenced by pH, so that could play a role, but bile acids are also highly dependent on pH. Emerging research is showing that bile acids may play an important role in IBS. People with IBS with diarrhea have higher levels of primary bile acids in their colon, and people with IBS with constipation have lower levels. The presence of bile acids seems to affect how quickly or slowly things move through the colon.” Soluble fibers like pectins, β-glucans, and guar gum (found in oats, barley, and many fruits and vegetables) are readily fermented; insoluble cellulose, and the insoluble lignins from woody plants and seeds, are not.2
The fact that fermentation by gut microbiota is related to IBS symptoms has lead to the emergence of a diet low in fermentable foods as an IBS treatment. “The traditional approach to treating IBS was to recommend more frequent smaller meals, and less insoluble fiber, fat, caffeine, and gas-producing foods,” Armul says. “A newer approach is a diet low in FODMAPs.” FODMAP is an acronym for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, all of which are short-chain carbohydrates fermented by gut bacteria. Numerous observational and randomized-controlled studies support the efficacy of the low-FODMAP diet in patients with IBS.5
Fiber on a Low-FODMAP Diet
Many fiber-rich foods must be omitted on a low-FODMAP diet, since fiber often is fermentable. “Getting enough fiber on a low-FODMAP diet can be hard because good fiber sources like whole-grain breads and most legumes are excluded,” Haller says. “If other low-FODMAP, high-fiber foods are not incorporated, we can see fiber intake plummet on this diet, which is not good.”
One key to incorporating fiber into a low-FODMAP diet is to control portion sizes. Smaller amounts of trigger foods may not elicit symptoms. “We use a bucket analogy,” Haller says. “The bucket represents a person’s unique capacity to tolerate FODMAPs. Since FODMAPs can have a gradual and cumulative effect, a person’s bucket can ‘fill up’ with high-FODMAP foods. If a person with FODMAP sensitivities exceeds their limit and ‘fills their bucket,’ they will experience symptoms. Sometimes just one type of FODMAP contributes to filling the bucket (just lactose, or just fructose, for example). Sometimes it’s a cumulative effect: too many short-chain fermentable carbohydrates from a variety of sources, and your bucket overflows.”
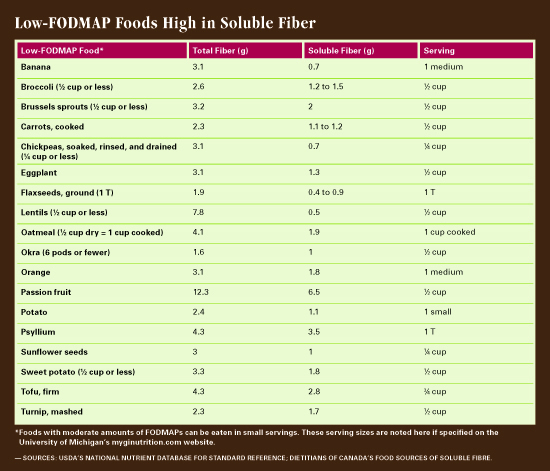
Fortunately, there are high-fiber foods that aren’t high in FODMAPs. “Quinoa is a high-fiber, low-FODMAP source,” Haller says. “So are oats. One-half cup of oatmeal or two tablespoons of oat bran per sitting are considered low FODMAP.” While beans and legumes are generally high FODMAP, Haller says that one-half cup of lentils and one-quarter cup of chickpeas may be tolerated. The galacto-oligosaccharides in these pulses are water soluble, so soaking and discarding the liquid before using is essential.6 Haller recommends sticking to canned chickpeas and lentils and rinsing and draining well. “It’s thought that the FODMAPs leach into the canning liquid over time, so rinsing canned chickpeas or lentils will wash away a lot of the FODMAPs,” she says. Nuts and seeds are great low-FODMAP sources of fiber. “All nuts except cashews and pistachios are low FODMAP,” Haller says, “but we recommend small handfuls. For example, 20 almonds are on the high-FODMAP list, but you won’t get too many FODMAPs if you only eat 10 to 15. And all seeds, including sunflower, chia, and flax, are fine in appropriate quantities as well.” Haller recommends adding ground flax or chia seeds to food. “This is another great way to add soluble fiber without changing the taste or volume of the food,” she says. “If you’re working with someone who’s a picky eater or doesn’t want to make changes, tricks like that can up the fiber in their diet.” Haller recommends a website developed by the University of Michigan division of gastroenterology and hepatology (myginutrition.com) and The Monash University Low FODMAP Diet app for information on low-FODMAP foods and portion sizes.
Many fruits and vegetables are low in FODMAPs as well, and some of these also are high in soluble fiber. “Oranges and bananas are low-FODMAP foods that are high in soluble fiber, as are passion fruit and guava if those fruits are familiar to your patient population. Berries like blueberries and strawberries, melons like honeydew and cantaloupe, and grapes are also low FODMAP, and, although they aren’t considered high in soluble fiber, they do have some, and it all adds up,” Haller says. “One-eighth of an avocado at a sitting also is a moderate-FODMAP food that delivers great fiber as well as healthful fats.” As far as vegetables are concerned, Brussels sprouts, carrots, eggplant, okra, sweet and white potatoes, and turnips are all low-FODMAP foods with great soluble fiber content.7,8 Sticking to appropriate portion sizes is essential on a low-FODMAP diet. A tablespoon of ground flaxseeds or one-quarter cup butternut squash are considered low FODMAP, for example, but any more than that at one sitting delivers too much fermentable fiber.8
Putting It Into Practice
The IFFGD suggests IBS patients strive for the same 20 g to 35 g of fiber recommended for the general population. Increasing fiber can help improve bowel function and decrease symptom severity, even though certain high-fiber foods like bran may increase gas and bloating.1 Emphasizing soluble fiber may be particularly helpful. According to the Linus Pauling Institute, the results of randomized controlled trials suggest that increasing soluble fiber intake gradually to 12 g to 30 g per day may be beneficial for patients with IBS-C, although fiber supplements could exacerbate symptoms in people whose main symptom is diarrhea.2 It’s essential to increase fiber intake gradually, as adding too much fiber too quickly can make things worse.1,2 If targets can’t be reached with dietary intake, fiber supplements (especially psyllium supplements) may be helpful.1,2
However, incorporating fiber into the diet of people with IBS should be done in concert with other treatment advice, such as keeping meals small. Since fiber isn’t the only IBS symptom trigger, and because the effect of fiber varies from person to person, elimination diets and food diaries may be useful for identifying particular trigger foods. Besides FODMAPs, caffeine, alcohol, high-fat meals, and sugary foods are known to be common triggers.1 “Recording types of food, size of meals, meal frequency, and how you felt throughout the rest of the day helps find links between food and symptoms,” Armul says. “Use that information to inform an elimination diet.”
“Registered dietitian nutritionists are best suited to assess the overall diet and determine what changes need to be made,” Haller says. “I work to gradually increase patients’ fiber intake, choosing low-FODMAP grains, starches, fruits, and vegetables.” While she agrees that the balance of soluble and insoluble fiber is important, Haller doesn’t recommend pointing that out to a patient. “They have enough to worry about, especially during the FODMAP elimination phase,” Haller says. “We as nutrition professionals should be familiar with low-FODMAP, high–soluble fiber foods and work that information into our plans and suggestions for patients. Sample menus, lists, and ideas are really helpful. We’ve created meal and snack suggestions that provide a balance of nutrients, including fiber.”
Fiber can trigger IBS symptoms by setting off an overreaction to mechanical stimuli or by providing fodder for bacterial fermentation. But fiber, and especially soluble fiber, has been shown to ease overall symptoms and constipation in IBS sufferers. By slowly increasing fiber intake with appropriate portions of high-fiber (and particularly high soluble fiber) foods that also are low in fermentable carbohydrates (ie, FODMAPs), patients with IBS can find relief—along with a more healthful overall dietary pattern.
— Judith C. Thalheimer, RD, LDN, is a freelance nutrition writer, a community educator, and the principal of JTRD Nutrition Education Services.
References
1. What is IBS? International Foundation for Functional Gastrointestinal Disorders website. http://www.aboutibs.org/what-is-ibs/what-is-ibs.html. Updated June 15, 2016.
2. Fiber. Linus Pauling Institute Micronutrient Information Center website. http://lpi.oregonstate.edu/mic/other-nutrients/fiber
3. Bijkerk CJ, Muris JW, Knottnerus JA, Hoes AW, de Wit NJ. Systematic review: the role of different types of fibre in the treatment of irritable bowel syndrome. Aliment Pharmacol Ther. 2004;19(3):245-251.
4. Bijkerk CJ, de Wit NJ, Muris JW, Whorwell PJ, Knottnerus JA, Hoes AW. Soluble or insoluble fibre in irritable bowel syndrome in primary care? Randomised placebo controlled trial. BMJ. 2009;339:b3154.
5. Shepherd SJ, Lomer MC, Gibson PR. Short-chain carbohydrates and functional gastrointestinal disorders. Am J Gastroenterol. 2013;108(5):707-717.
6. Iacovou M, Tan V, Muir JG, Gibson PR. The low FODMAP diet and its application in East and Southeast Asia. J Neurogastroenterol Motil. 2015;21(4):459-470.
7. Food sources of soluble fibre. Dietitians of Canada website. http://www.dietitians.ca/Downloads/Factsheets/Food-Sources-of-Soluble-Fibre.aspx
8. Low FODMAP foods. My Nutrition Health website. http://myginutrition.com/tools.html


