Today’s Dietitian
Vol. 18, No. 12, P. 18
Can dietitians make a case for supplements?
Research has long established the important part magnesium plays in building bones through its relationship with calcium and vitamin D. Relatively new to the research scene is magnesium’s role in everything from healthy blood pressure and decreased risk of stroke and heart disease to preventing migraine headaches and reducing type 2 diabetes risk. But because dietary intake is declining among people eating westernized diets, the need for magnesium supplementation may be increasing.
Magnesium is considered a major mineral. About 50% to 60% of the magnesium in the body is locked inside bones; the rest resides in soft tissue like muscle. The human skeleton acts as a magnesium reservoir, buffering magnesium concentration in the blood. As we age, the magnesium reservoir in bones is reduced to nearly one-half over the course of a lifetime.1
Impact on Cardiovascular Health
Theories about magnesium’s role in heart disease and stroke prevention have been circulating for years, but a dearth of well-designed studies to specifically address this question existed until recently. Researchers were pointed in the right direction in 2013 when a meta-analysis published in The American Journal of Clinical Nutrition found that circulating and dietary magnesium are inversely associated with cardiovascular disease (CVD) risk. The analysis included 16 studies involving more than 313,000 individuals and found that higher circulating magnesium levels were associated with a 30% lower risk of CVD.2
In 2015, the International Journal of Cardiology published results from a cohort of the EPIC study that looked at dietary magnesium intake and its relationship to stroke and blood pressure. Men (but not women) with the lowest intakes of magnesium had the highest risk of stroke and had significantly higher blood pressure and total cholesterol measures.3 While this reveals a clear association between dietary magnesium and blood pressure and stroke, it doesn’t prove a cause and effect relationship.
In 2016, The American Journal of Clinical Nutrition published a double-blind, placebo-controlled clinical trial measuring the effect of magnesium supplements on arterial stiffness, a marker for heart disease. Researchers used what’s considered the gold-standard method for quantifying arterial stiffness, carotid-to-femoral pulse wave velocity, a noninvasive measurement of a wave pulse traveling along the aorta. Participants in the intervention arm of the trial were given 350 mg magnesium citrate per day in three divided doses and experienced a significant reduction in arterial stiffness.4
And earlier this year the journal Hypertension published a meta-analysis that looked exclusively at good quality randomized, double-blind, placebo-controlled trials on the effect of magnesium supplements on blood pressure. Researchers concluded that 300 mg per day of supplemental magnesium for one month was sufficient to significantly reduce blood pressure.5
Role in Migraine Headaches
The relationship between magnesium and migraine headaches has been a topic of interest for years, but new research gives strong support for including magnesium supplements as a potential component of routine care for migraine sufferers. A 2015 study compared the efficacy of IV treatment in 70 acute migraine sufferers with either magnesium sulfate or standard drug therapy (dexamethasone/metoclopramide). Pain measurements decreased in both groups, but the patients receiving magnesium recorded significantly improved pain scores at intervals of 20 minutes, one hour, and two hours compared with those receiving standard drug treatment. Since the magnesium sulfate was administered through an IV solution, it’s difficult to extrapolate these results to oral magnesium supplements.6 However, a 2016 meta-analysis tackled the question by looking at both IV and oral magnesium as treatment for migraine headache pain. The meta-analysis examined a total of 10 studies looking at oral magnesium supplementation and found a significant decrease in frequency and severity of migraine headaches in people taking supplemental magnesium (doses varied between 100 and 800 mg/day, mostly in the form of magnesium citrate). Researchers concluded that oral magnesium supplements significantly decreased the frequency and intensity of migraine headaches and should be adopted as part of a multifactorial approach to treating migraines.7 Experts suggest magnesium deficiency may be present in up to one-half of all migraine sufferers—possibly from increased urinary excretion due to a hormonally influenced stress response—and that 400 mg per day of supplemental magnesium citrate is a reasonable and safe intervention for most people who experience migraine headaches.8
Magnesium and Diabetes
A 2011 meta-analysis published in Diabetes Care examined epidemiologic studies with more than 500,000 participants and showed a diabetes risk reduction of 14% with every 100 mg increase in daily dietary magnesium intake.1 Accumulating epidemiologic evidence of this relationship between magnesium and type 2 diabetes prompted a group of researchers from Mexico to look more closely at the issue. Their work was published in 2011 in the journal Magnesium Research, citing lower incidence of type 2 diabetes among people consuming high levels of dietary magnesium compared with people eating a lower-magnesium diet. However, the researchers were quick to point out the lack of good clinical trials to confirm a causal relationship.9
To follow-up, some of these same researchers went on to investigate the question in a more robust setting. In 2015, their double-blind, placebo-controlled study of magnesium supplementation in 116 people with prediabetes who also had low blood levels of magnesium was published in the journal Diabetes and Metabolism. Study subjects in both the intervention and control groups were instructed to incorporate standard diet and exercise to improve insulin sensitivity. However, the intervention arm also received 382 mg magnesium chloride through an oral supplement daily for four months. After four months, fasting and postprandial glucose levels were significantly lower in the intervention group compared with placebo. A standardized measure of insulin resistance also was significantly lower in the intervention group. The study authors concluded that oral magnesium supplementation does indeed improve glycemic status in people with prediabetes who start off with low serum levels of magnesium.10
Magnesium has influence over several enzymes and enzymatic reactions in the human body. Among them is tyrosine kinase, an enzyme that helps activate insulin receptors, and has been postulated to function at less than full throttle in the absence of adequate magnesium.10 In addition, magnesium deficiency is related to an increase in proinflammatory cytokines. Data from the National Health and Nutrition Examination Survey (NHANES) published in 2005 in the Journal of the American College of Nutrition show that adults who consumed less than 50% of the recommended dietary allowance (RDA) for magnesium were more than twice as likely to have elevated C-reactive protein—an inflammation marker—than adults who met their RDA for magnesium.11 Together, these metabolic responses to low circulating magnesium levels may explain the increase in insulin resistance and type 2 diabetes risk, along with risk of stroke and CVD.1,2
Counseling Patients
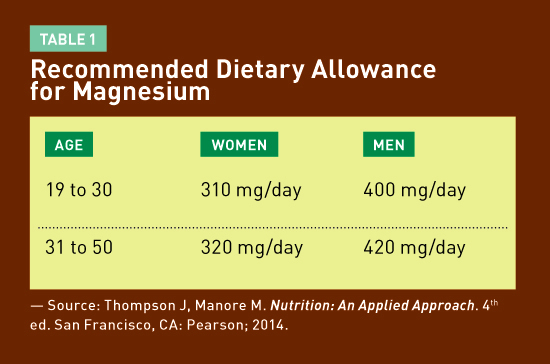
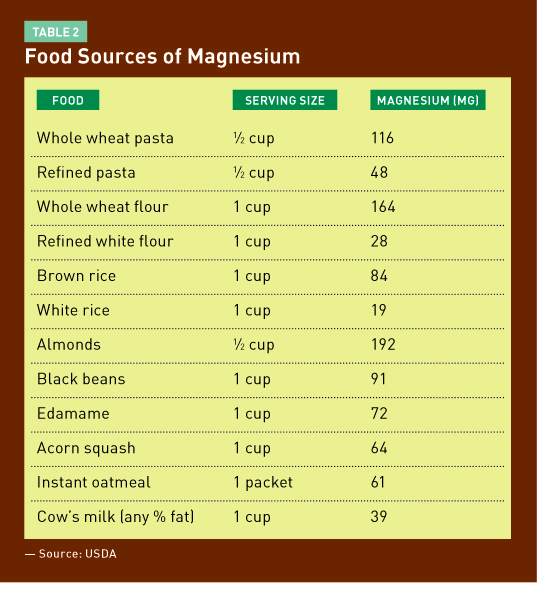
So who’s at risk of not getting adequate dietary magnesium? Many Americans, it turns out (see Table 1 for RDA for magnesium). Evidence shows average magnesium intakes in the United States have significantly declined over the last few generations. NHANES data from 2000 show 68% of US adults consume less than the RDA for magnesium and about 20% consume under 50% of the RDA.11 Refined whole grains may be a major contributor to this trend: Processing wheat to flour or brown rice to white rice reduces the magnesium content significantly (see Table 2).12
Adding to the challenge of obtaining optimal serum magnesium levels is the fact that magnesium balance is controlled by a fine-tuned interplay of intestinal absorption, exchange with bone, and kidney function. On average, only about one-third of ingested dietary or supplemental magnesium is absorbed into the blood.1
Consuming 100% whole grains can ensure higher dietary magnesium intake. Dietitians can recommend patients include brown rice, whole wheat, and oats along with nuts and beans to boost their total daily magnesium consumption (see Table 2).
For people who tend to eat a standard American diet low in these foods, a magnesium supplement may be important. Researchers point to magnesium citrate as the best form. Doses used in most studies varied between 300 and 400 mg/day and were found to be safe and well tolerated. Finally, dietitians can suggest people suffering from migraine headaches try magnesium citrate supplements as a standard part of their therapy for pain control and prevention with the expectation that up to 50% of migraine sufferers may have a beneficial response. Note that magnesium at high doses has a known stool-softening effect, so patients should be monitored for changes in bowel function while on magnesium supplements, especially at doses above 400 to 600 mg/day.
— Clare Tone, MS, RD, is a freelance writer, nutrition instructor, and high-altitude gardener.
References
1. Vormann J. Magnesium: nutrition and homeostasis. AIMS Public Health. 2016;3(2):329-340.
2. Del Gobbo LC, Imamura F, Wu JH, de Oliveira Otto MC, Chiuve SE, Mozaffarian D. Circulating and dietary magnesium and risk of cardiovascular disease: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr. 2013;98(1):160-173.
3. Bain LK, Myint PK, Jennings A, et al. The relationship between dietary magnesium intake, stroke and its major risk factors, blood pressure and cholesterol, in the EPIC-Norfolk cohort. Int J Cardiol. 2015;196:108-114.
4. Joris PJ, Plat J, Bakker SJ, Mensink RP. Long-term magnesium supplementation improves arterial stiffness in overweight and obese adults: results of a randomized, double-blind, placebo-controlled intervention trial. Am J Clin Nutr. 2016;103(5):1260-1266.
5. Zhang X, Li Y, Del Gobbo LC, et al. Effects of magnesium supplementation on blood pressure: a meta-analysis of randomized double-blind placebo-controlled trials. Hypertension. 2016;68(2):324-333.
6. Sharami A, Assarzadegan F, Hatamabadi HR, Asgarzadeh M, Sarehbandi B, Asgarzadeh S. Comparison of therapeutic effects of magnesium sulfate vs. dexamethasone on alleviating acute migraine headache. J Emerg Med. 2015;48(1):69-76.
7. Chiu HY, Yeh TH, Huang YC, Chen PY. Effects of intravenous and oral magnesium on reducing migraine: a meta-analysis of randomized controlled trials. Pain Physician. 2016;19(1):E97-E112.
8. Mauskop A, Varughese J. Why all migraine patients should be treated with magnesium. J Neural Transm (Vienna). 2012;119(5):575-579.
9. Rodríguez-Morán M, Simental Mendía LE, Zambrano Galván GZ, Guerrero-Romero F. The role of magnesium in type 2 diabetes: a brief-based clinical review. Magnes Res. 2011;24(4):156-162.
10. Guerrero-Romero F, Simental-Mendía LE, Hernández-Ronquillo G, Rodríguez-Morán M. Oral magnesium supplementation improves glycemic status in subjects with prediabetes and hypomagnesemia: a double blind placebo-controlled randomized trial. Diabetes Metab. 2015;41(3):202-207.
11. King DE, Mainous AG 3rd, Geesey ME, Woolson RF. Dietary magnesium and C-reactive protein levels. J Am Coll Nutr. 2005;24(3):166-171.
12. Nutrient lists: nutrients: magnesium, Mg(mg). United States Department of Agriculture, Agricultural Research Service website. https://ndb.nal.usda.gov/ndb/nutrients/report/nutrientsfrm?max=25&offset=0&totCount=
0&nutrient1=304&nutrient2=&nutrient3=&subset=0&sort=f&measureby=m. Updated May 2016. Accessed October 2, 2016.


