Today’s Dietitian
Vol. 19, No. 6, P. 38
Emerging research shows that protein quality, not quantity, may help slow CKD progression.
Approximately 14% of the US population has chronic kidney disease (CKD).1 As discussed in part one of this two-part series, research shows that controlling diabetes, high blood pressure, and obesity can help prevent CKD. Dietary changes are key to addressing these risk factors, and current research is focusing on healthful dietary patterns as a means of prevention. New research shows that dietary pattern, specifically with regard to protein balance, also may be the key to preventing progression in those already showing signs of kidney damage. CKD typically is a progressive disease, but advancement to kidney failure isn’t inevitable: Medications, diet, and other lifestyle changes can slow progression.2
In this second half of our update on diet and kidney disease, Today’s Dietitian looks at exciting new research into how increasing intake of certain fruits and vegetables can slow progression and reduce CKD complications.
Body Out of Balance
The kidneys are critical in keeping the body functioning properly. They regulate the composition and volume of blood, remove metabolic wastes, produce erythropoietin needed for red-blood cell synthesis, and activate vitamin D needed for calcium absorption and bone health. They also control acid/base balance.3 When the kidneys aren’t working well, everything goes haywire. People with CKD are prone to anemia due to impaired erythropoiesis (the process of red blood cell production) and low iron stores; mineral imbalance and bone disorders involving vitamin D, calcium, and phosphorus; high levels of serum potassium (hyperkalemia); malnutrition; salt and fluid retention often associated with worsening high blood pressure; metabolic acidosis; and high rates of cardiovascular disease (CVD).3
Kidney damage is a multifactorial process, but kidney disease always is marked by a decrease in the ability of the filtering units of the kidney (the glomeruli) to filter blood. The five stages by which kidney failure is measured are based on estimated glomerular filtration rate (eGFR). In stage 1 (eGFR of 90 or above), the kidneys can still do their job, but urine tests indicate a problem. Complications become more likely and more severe as eGFR declines, until stage 5 (also known as end-stage renal disease or kidney failure, and defined as an eGFR of less than 15), at which point dialysis or kidney transplant becomes necessary.4
Nutritional Interventions
The purpose of diet therapy in CKD is to delay progression and prevent and treat complications.2 Premature death due to CVD and all other causes is so high that adults with CKD are 16 to 40 times more likely to die than to progress to kidney failure.5 With this connection between CKD and CVD, a heart-healthy diet is a must, and for those patients with diabetes, good blood sugar control is important.2 But many of the dietary recommendations for CKD are an attempt to restore balance in the body when blood or urine tests indicate something is amiss. Dietary changes are essential to the management of CKD, and dietary restrictions become more complex as kidney function declines. As the kidneys become less able to maintain balance in the body, dietary intake of sodium, potassium, phosphorus, and calcium may need to be adjusted, and fluid restriction may become necessary in later stages.3
Protein and CKD
Protein restriction has long been a major and controversial issue in CKD management. Current recommendations vary, and the latest guidelines haven’t been updated since 2012, but generally it’s recommended that CKD patients restrict protein intake to the Recommended Dietary Allowance of 0.8 g/kg body weight per day. Some governing bodies suggest attempting lower intake for some patients, and most specifically recommend avoiding excessive intake (see sidebar).
One of the reasons dietary protein may be hard on the kidneys is its effect on renal acid load. “The kidneys remove acid from the blood and put it in the urine,” says Donald E. Wesson, MD, MBA, FASN, an acid/base physiologist who’s president of the Diabetes Health and Wellness Institute at Baylor Scott and White Health, and a professor of medicine at Texas A&M College of Medicine. “Diets in industrialized societies tend to be high in foods that create a high dietary acid load,” Wesson says. This makes the kidneys work harder. “We wondered what effect months or years of high acid load would have on the kidneys over time,” Wesson says. “What we have found is, at least in rats, the more acidic the diet, the worse its effect on kidney function.” Research by Wesson and others on the relationship between dietary protein and acid/base balance in the body could be a key to determining appropriate protein intake recommendations.
Metabolic acidosis (characterized by low serum bicarbonate concentration) is known to contribute to GFR decline and is associated with a further increase in the already high rate of CVD-related mortality in CKD patients.6 Supplementation with oral sodium bicarbonate can correct acidosis.3 Interestingly, in animal models of kidney disease, bicarbonate administration has been found to slow progressive GFR decline even if the animals don’t have acidosis, and emerging evidence indicates that patients with any change from normal toward the acid spectrum of the acid-base balance are at higher risk of all-cause mortality.7,8 These findings suggest that high dietary acid load itself might contribute to kidney disease progression.
Animal-based proteins yield acids when metabolized, so restricting dietary protein may improve acid/base balance.3,9 “Protein restriction has been a complicated topic over the years,” says Michael Conrad, MD, senior member of the Center for Kidney Care in New Jersey. “In the past, severe restriction (less than 0.6 g/kg) was believed to slow progression, but the diet was very restrictive, and there were complications associated with it, including malnutrition.” Then, in 1994, the Modification of Diet in Renal Disease study was published in The New England Journal of Medicine. Two large clinical trials found that reducing total protein intake made very little difference in kidney disease progression, and a very low-protein diet didn’t slow further progression.10
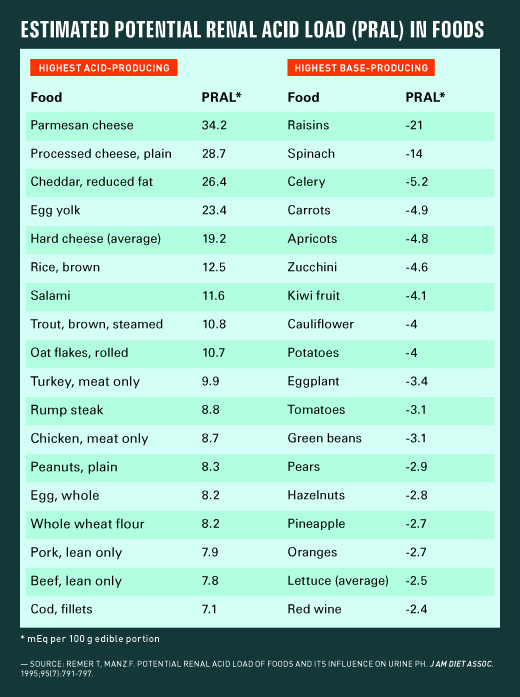
Research by Wesson and others suggests that the issue may be not the quantity of protein but the quality.11 While animal proteins increase acid load, the metabolism of plant-sourced protein, for the most part, yields base (alkali). “Rather than total protein restriction, adding base-producing plant-sourced protein to the diet seems to make the difference,” Wesson says. In a 2013 study, Wesson and colleagues found that increasing alkali-producing fruit and vegetable intake improved metabolic acidosis and reduced kidney injury in stage 4 CKD. Baseline total protein intake of study participants was 1.2 g/kg, nearly all from animal sources. The researchers provided fruits and vegetables known to have low dietary acid load (see table). Although there was little change in participants’ total protein intake, a greater proportion of total protein was now plant based, and, after one year, the eGFR of participants receiving fruits and vegetables hadn’t worsened, metabolic acidosis had improved, and urine indices of kidney injury were lower.12 A comparison group that received sodium bicarbonate had similar outcomes, but sodium bicarbonate supplements can raise blood pressure, which may further damage the kidneys.3
It should be noted that plant foods typically are high in potassium, so adding fruits and vegetables to the diet of people with CKD could contribute to hyperkalemia. High-potassium foods typically are restricted in CKD diets when serum potassium levels begin to rise.3 “We carefully selected patients at low risk of developing hyperkalemia in our study,” Wesson says. “Until we have larger-scale studies, we don’t recommend trying this approach in patients with a history of hyperkalemia, or in patients with less than 30% normal kidney function.” In other words, increasing fruits and vegetables in CKD stages 1 to 3 may help slow disease progression by lessening renal acid load, but this approach isn’t recommended for patients in stages 4 or 5 at this time.
“As acid/base physiologists, our focus is just on the alkali-producing aspects of fruits and vegetables, which seem to be kidney protective. Of course, there are a lot of other good things in plant foods that may help protect kidney function,” Wesson says. “Data also suggest a plant-based diet reduces CVD risk in kidney disease.”
A 2017 meta-analysis in the Clinical Journal of the American Society of Nephrology concluded that dietary patterns higher in fruits and vegetables, fish, legumes, cereals, whole grains, and fiber, and lower in red meat, salt, and refined sugars were associated with lower all-cause mortality in patients with CKD.13 “I’m really excited about finding ways to get patients with CKD to increase their plant intake,” Wesson says, “because a diet that balances out animal-based proteins with plenty of plant foods can extend the whole life, not just the kidney life.”
Putting It Into Practice
While this research is promising, it hasn’t yet been translated into recommendations. “Moderate protein restriction is still recommended,” Conrad says, “and the more advanced the stage of kidney disease, the more emphasis is placed on protein restriction.” The Chronic Renal Insufficiency Cohort Study, funded by the National Institute of Diabetes and Digestive and Kidney Diseases, is examining risk factors for progression of CKD, which may result in revisions to treatment guidelines for risk factor reduction, and the Academy of Nutrition and Dietetics in partnership with the National Kidney Foundation Kidney Disease Outcomes Quality Initiative is aiming to release updated guidelines in 2018.4,14 Existing protein intake recommendations are summarized in the sidebar.
To add potentially protective base-producing foods to the diet, Wesson recommends plenty of dark leafy vegetables like collard, turnip, and mustard greens, and kale and spinach. Raisins have the lowest potential renal acid load of any food or beverage presented in Remer and Manz’s original study that introduced the concept of potential renal acid load in 1995.9 Citrus fruits also are protective. Although they’re acidic before consumption, they create an impressive amount of base when metabolized (except for grapefruit). Cheeses and egg yolk have the greatest impact on increasing kidney-damaging renal acid load, with meats, poultry, and some fish ranking high on the list as well. Some surprises on the acid-producing list include some foods normally considered healthful choices, like peanuts, rolled oats, and whole wheat products.9
Studies are being done to confirm the findings of Wesson and his colleagues, so keep an eye out for information on using fruits and vegetables to reduce renal acid load and slow kidney disease progression. In the meantime, increasing intake of plant foods is unequivocally linked to better overall health, so moving clients with or without early-stage CKD toward this goal is a recommendation everyone can get behind.
— Judith C. Thalheimer, RD, LDN, is a freelance nutrition writer, speaker, and community educator in Philadelphia, Pennsylvania.
RECOMMENDED DIETARY PROTEIN INTAKE GUIDELINES
Protein intake recommendations vary and haven’t been updated recently. The following is a summarization of some of the available guidelines:
2010 Academy of Nutrition and Dietetics Nutrition in Chronic Kidney Disease (CKD)
• 0.6 to 0.8 g/kg/day for adults with CKD without diabetes, not on dialysis, and with an estimated glomerular filtration rate (eGFR) <50 mL/min/1.73 m2, based on the client’s motivation level, willingness to participate in frequent follow-ups, and risk of protein-energy malnutrition
• 0.9 g/kg for adults with diabetic nephropathy to avoid hypoalbuminemia
* The Academy of Nutrition and Dietetics and the National Kidney Foundation Kidney Disease Outcomes Quality Initiative are aiming to release updated guidelines in 2018.
2012 Kidney Disease Improving Global Outcome Clinical Practice Guideline for the Evaluation and Management of CKD
• 0.8 g/kg/day in adults with or without diabetes and GFR <30 mL/min/1.73 m2
• Avoid protein intake over 1.3 g/kg/day in adults with CKD at risk of progression.
• Dietary protein restriction below 0.8 g/kg/day appears to offer no advantage.
National Institute of Diabetes and Digestive and Kidney Diseases
• 0.8 g/kg/day
• Further lowering to 0.6 g protein/kg/day in patients without diabetes may be beneficial, although many patients will be unable to achieve this level even with intensive nutrition counseling.— Sources: Academy of Nutrition and Dietetics; Kidney International; National Institute of Diabetes and Digestive and Kidney Diseases
References
1. Kidney disease statistics for the United States. National Institute of Diabetes and Digestive Kidney Diseases website. https://www.niddk.nih.gov/health-information/health-statistics/Pages/kidney-disease-statistics-united-states.aspx. Published December 2016.
2. Slow progression and reduce complications. National Institute of Diabetes and Digestive Kidney Diseases website. https://www.niddk.nih.gov/health-information/health-communication-programs/nkdep/identify-manage/manage-patients/slow-progression/Pages/slow-progression.aspx
3. National Kidney Disease Education Program. Making sense of CKD: a concise guide for managing chronic kidney disease in the primary care setting. https://www.niddk.nih.gov/health-information/health-communication-programs/nkdep/a-z/Documents/ckd-primary-care-guide-508.pdf. Published July 2014.
4. CKD stages. The Renal Association website. http://www.renal.org/information-resources/the-uk-eckd-guide/ckd-stages#sthash.yABcBEd9.dpbs. Published 2013.
5. Chronic kidney disease and kidney failure. National Institutes of Health website. https://report.nih.gov/nihfactsheets/ViewFactSheet.aspx?csid=34. Updated March 29, 2013.
6. Wesson DE. Does serum HCO3 predict risk for cardiovascular disease? Am J Nephrol. 2017;45(2):115-117.
7. Wesson DE. Is NaHCO3 an antiaging elixir? Am J Physiol Renal Physiol. 2016;311(1):F182-F183.
8. Mahajan A, Simoni J, Sheather SJ, Broglio KR, Rajab MH, Wesson DE. Daily oral sodium bicarbonate preserves glomerular filtration rate by slowing its decline in early hypertensive nephropathy. Kidney Int. 2010;78(3):303-309.
9. Remer T, Manz F. Potential renal acid load of foods and its influence on urine pH. J Am Diet Assoc. 1995;95(7):791-797.
10. Modification of Diet in Renal Disease (MDRD). National Institute of Diabetes and Digestive and Kidney Diseases Central Repository website. https://www.niddkrepository.org/studies/mdrd/
11. Goraya N, Wesson DE. Dietary protein as kidney protection: quality or quantity? J Am Soc Nephrol. 2016;27(7):1877-1879.
12. Goraya N, Simoni J, Jo CH, Wesson DE. A comparison of treating metabolic acidosis in CKD stage 4 hypertensive kidney disease with fruits and vegetables or sodium bicarbonate. Clin J Am Soc Nephrol. 2013;8(3):371-381.
13. Kelly JT, Palmer SC, Wai SN, et al. Healthy dietary patterns and risk of mortality and ESRD in CKD: a meta-analysis of cohort studies. Clin J Am Soc Nephrol. 2017;12(2):272-279.
14. Current KDOQI projects. National Kidney Foundation website. https://www.kidney.org/professionals/guidelines/current-KDOQI-projects. Published 2016.