Today’s Dietitian
Vol. 18 No. 4 P. 12
Thickened liquids are commonly prescribed for patients with dysphagia. However, dissatisfaction with and inaccessibility to thickened liquids frequently results in poor patient compliance. Reduced compliance can lead to dehydration, weight loss, weakness, respiratory illness, and increased risk of falls. In fact, evidence has shown that noncompliance by patients prescribed thickened liquid diets correlated to significantly higher mortality rates compared with those who were compliant. Nutrition professionals, caregivers, and patients must be diligent in pursuing options that meet both accessibility and palatability preferences to overcome compliance barriers for patients with swallowing disorders to improve health outcomes and quality of life.
The prevalence of dysphagia in the healthy older adult population ranges between 13.8% and 37.6%.1-5 Cabre and colleagues found that 55% of 134 community dwelling elderly adults >70 years of age diagnosed with pneumonia demonstrated clinical signs of dysphagia.6 Reduced muscle mass, strength,7 range of motion,8 and sensory awareness that occurs due to normal aging can lead to increased oral transit time, delayed swallowing onset, and poor airway protection during swallowing. These symptoms increase the risk of laryngeal penetration and laryngeal aspiration. In addition to normal aging, various neurogenic diagnoses also can result in dysphagia, including the following (percentages represent prevalence rate of dysphagia in people with these diseases): stroke (38% to 51%),9 dementia (45%),10 and four out of five individuals with Parkinson’s disease.11
Key factors in reducing the incidence of aspiration pneumonia and other negative health outcomes include early identification, effective and efficient intervention, and patient compliance.
Identification and Effective Intervention
A timely assessment by a certified speech-language pathologist experienced in differential diagnosis and implementation of an effective individualized intervention plan can address the first two factors of identification and effective intervention. Changing the rheological properties of the thickened liquid increases the cohesion of the bolus, reduces the flow rate of the bolus through the pharynx,12 and potentially improves clearance of the bolus. Although the direct effect thickened liquids have on health outcomes remains under investigation, it endures as a common management technique to minimize the risk of aspiration in individuals with dysphagia.13,14 In a survey study investigating the practice patterns of speech-language pathologists, the majority of respondents reported thickened liquids to be an effective method to reduce the risk of aspiration in individuals with dysphagia. Nectarlike liquids were more commonly prescribed than honeylike liquids and were most commonly recommended for characteristics including delayed swallow onset, poor oral control of thin liquids, and laryngeal penetration/aspiration.13
Patient Compliance
Psychosocial Factors
The third key factor to successful dysphagia management is patient compliance. Many individuals report the difficulty of following a modified diet of thickened liquids due to affordability, accessibility, and palatability. In a survey done by Garcia, Chambers, and Molander, nearly one-half of the individuals surveyed reported a strong dislike of thickened liquids.13 Another study reported 45% of survey respondents on a modified diet said that eating was no longer an enjoyable experience.15 Leiter and Windsor evaluated a group of geriatric individuals’ compliance to thickened liquids after a five-day period. Patient compliance was expected to be relatively high after such a short period; however, only 35.6% adhered to the dietary modifications.16 Noncompliance may be due to poor palatability and reduced accessibility and/or increased cost of the thickened liquids. Another consideration is the reported decreased quality of life in individuals with dysphagia. Psychosocial effects such as depression, isolation, and anxiety17 also could result in poor compliance.
Health Outcomes
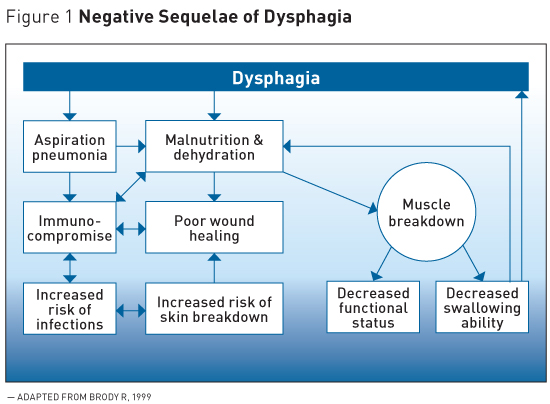
Noncompliance can lead to a cascade of negative health sequelae including malnutrition, dehydration, weight loss, muscle atrophy, increased risk of falls, and respiratory illness (see Figure 1 online).18
A compelling study by Low and colleagues revealed the serious health consequences of noncompliance. The authors reported that 86% of individuals who made a conscious decision not to comply with speech-language pathologists’ thickened liquid recommendations died. This is a significant contrast to the 39.5% who died despite following dietary recommendations.19 In addition, the degree to which recommendations were followed was correlated with the incidence of chest infections, aspiration pneumonia, and hospital readmissions. Those who were noncompliant were considerably younger, living at home, and had significantly more hospital admissions and chest infections or aspiration pneumonia than those who complied.
Improving Compliance
Community-Dwelling Individuals
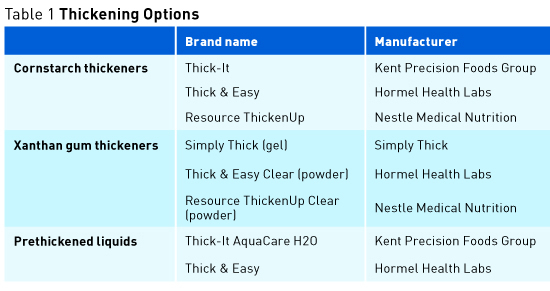
Encouraging patients to follow modified diet recommendations is important but may be insufficient to prompt them to make such a lifestyle change. Education and training in how to use the products is essential. Far too often a patient is sent home with the name of a powdered thickener and told to follow the directions on the back of the container. Patients often are unaware of various thickening options (see Table 1 on page 13), how to mix the product with the desired beverage, how the viscosity can change over time and/or temperature, the influence of a particular beverage on the viscosity, creative recipes using thickening products, and how to plan for a social event or dining out experience. Providing resources for various thickened liquid options, identifying additional palatable and accessible thickened liquids and recipes, and education and training all play important roles in compliance.
Patients in Medical and Long Term Care Facilities
Cornstarch thickeners continue to be the most commonly used in medical facilities, although use of xanthan gum powders and prethickened beverages is on the rise in acute and subacute facilities. Dietitians and other patient care providers must advocate for the importance of compliance to administrators and work together to identify solutions to this problem. Evidence such as patient health status or change in status, volume of oral intake at mealtimes, and amount of food and liquids refused by the patient may provide important information to help drive the mission of patient compliance in medical facilities.
Thickened Liquids
Instant Food Thickeners: Powders and Gels
Historically, instant food thickeners made from refined cornstarch have been used to thicken liquids for individuals requiring a modified diet. Cornstarch thickeners are inexpensive but they’re high in sugar, may contain gluten, can negatively influence taste and smell, add calories, and contribute to constipation. In addition, cornstarch thickeners are unstable, continuing to thicken over time, and don’t thicken different beverages consistently. Recently, thickeners using refined xanthan gum have become commercially available. Xanthan gum thickeners are more stable over time and don’t alter taste or smell but are more expensive, aren’t readily accessible, and can change viscosity over temperature changes. Due to the need for manual mixing, both cornstarch and xanthan gum instant thickeners are subject to human error.
[Click here to enlarge Figure 2]
Prethickened Liquids
To alleviate human error, medical nutrition companies began marketing beverages that come prethickened or ready to pour. These beverages maintain their viscosity over time and are convenient for consumers. The prethickened beverage can be added to a number of products, making it very versatile. However, these products are typically more expensive and less accessible to consumers.
Studies comparing thickening products have revealed substantial variability between and within thickened liquid products. For example, prethickened beverages have significantly higher viscosity ratings than beverages thickened with instant food thickeners and tend to be more viscous than recommended in the National Dysphagia Diet standards.20 Statistically significant differences in viscosity values among brands of instant food thickeners have been reported.21,22 Leonard and colleagues reported significant reduction in aspiration rate and lower scores on the penetration-aspiration scale with xanthan gum thickener. Although the aspiration rate was reduced with cornstarch thickener, the difference didn’t reach significance, suggesting xanthan gum may be more effective in reducing aspiration in individuals with dysphagia.23 Interestingly, boluses thickened with cornstarch were more viscous than those thickened with xanthan gum, but they weren’t more effective in minimizing aspiration.23
Naturally Nectarlike Liquids
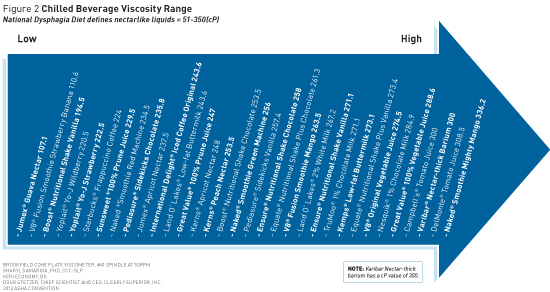
In an attempt to identify more palatable and accessible options for individuals who require thickened liquids, a recent study investigated the viscosity of a variety of commercially made beverages and found 32 products that met the National Dysphagia Diet standards for nectarlike liquids without adding a powder or gel thickener (see Figure 2 online).24 Viscosity was measured using a Brookfield cone plate viscometer with a No. 41 spindle at 50 rpm.24 Of importance, the majority of beverages had a significantly higher viscosity rating when chilled vs room temperature. The beverages listed in Figure 2 aren’t intended to be recommended for all patients who require nectarlike beverages, as some may not be thick enough to be therapeutic. Dietitians should consult a patient’s speech-language pathologist before recommending any of the beverages in Figure 2.
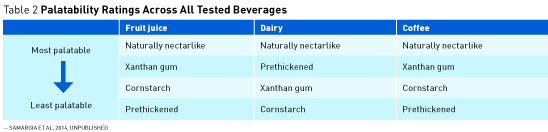
In a follow up study, the palatability of these “naturally” nectarlike beverages was significantly higher than cornstarch thickeners across beverage categories (see Table 2 below).25 Although one might suspect beverages with higher viscosity would be least palatable, there was no correlation between palatability and viscosity values. (See Figure 2 online for the beverages tested and the viscosity ratings.) These findings revealed “naturally thick” beverages can be found on supermarket shelves and are more palatable than those thickened with a powder.
Encouraging Palatability
Patients and families can access various dysphagia diet products such as prethickened liquids and thickening powders, including both cornstarch and xanthan gum types, through www.dysphagia-diet.com. If there’s a beverage found at the supermarket that appears to be thick, be sure to ask the speech-language pathologist to determine whether the thickness is appropriate. Patients are encouraged to try a variety of the thickening options in many different beverages to determine those that are most palatable to them. Some patients and their families create their own recipes in order to increase palatability. Although this is encouraged, the family should continually consult with a speech-language pathologist to ensure the beverage is the appropriate thickness. Recipes for thickened liquids can be found in a book entitled Living with Dysphagia: A Food and Beverage Guide for Individuals With Chewing and Swallowing Difficulties, revised by Debra Zwiefelhofer, RDN, LD, for Med-Diet Laboratories, Inc, available through the website listed above.
Moving Forward
Serious health complications often are associated with dysphagia, particularly for those who don’t comply with modified diet recommendations. Of equal importance is the negative impact on quality of life. Social interaction within our culture often revolves around food. Individuals with dysphagia frequently feel isolated or restricted due to their dietary needs. It’s imperative that dietitians and others in the medical community educate individuals and families about the multitude of options available for thickened liquids. The medical nutrition field has created innovative and unique products to improve palatability and versatility, which will allow patients to find options that work for them and ultimately improve compliance. As health care providers, we must address compliance head on and encourage patients to adhere to recommendations while we push medical facilities to see past supposed costs and do what’s best for our patients.
While timely identification and intervention are imperative in dysphagia management, more emphasis must be placed on improving patient compliance through continued efforts to make thickened liquids more palatable, accessible, and affordable for individuals with dysphagia. In addition, medical facilities need to recognize the overall health and economic impact of patient compliance. Continued contributions to this line of research will offer compelling information to reduce the adverse health effects and reduced quality of life in individuals with dysphagia.
— Sharyl A. Samargia, PhD, CCC-SLP, is an associate professor in the department of communication sciences and disorders at the University of Wisconsin at River Falls. Her research interest involves the study of neuroplasticity as it relates to disorders of voice, motor speech, and swallowing.
References
1. Eslick GD, Talley NJ. Dysphagia: epidemiology, risk factors and impact on quality of life—a population-based study. Aliment Pharmacol Ther. 2008;27(10):971-979.
2. Kawashima K, Motohashi Y, Fujishima I. Prevalence of dysphagia among community-dwelling elderly individuals as estimated using a questionnaire for dysphagia screening. Dysphagia. 2004;19(4):266-271.
3. Kjellén G, Tibbling L. Manometric esophageal function, acid perfusion test and symtomatology in a 55-year old general population. Clin Physiol. 1981;1(4):405-415.
4. Bloem BR, Lagaay AM, van Beek W, Haan J, Roos RA, Wintzen AR. Prevalence of subjective dysphagia in community residents aged over 87. BMJ. 1990;300(6726):721-722.
5. Roy N, Stemple J, Merrill RM, Thomas L. Dysphagia in the elderly: preliminary evidence of prevalence, risk factors, and socioemotional effects. Ann Otol Rhinol Laryngol. 2007;116(11):858-865.
6. Cabre M, Serra-Prat M, Palomera E, Almirall J, Pallares R, Clavé P. Prevalence and prognostic implications of dysphagia in elderly patients with pneumonia. Age Ageing. 2010;39(1):39-45.
7. Fucile S, Wright PM, Chan I, Yee S, Langlais ME, Gisel EG. Functional oral-motor skills: do they change with age? Dysphagia. 1998;13(4):195-201.
8. Sura L, Madhavan A, Carnaby G, Crary MA. Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging. 2012;7:287-298.
9. Parker C, Power M, Hamdy S, Bowen A, Tyrrell P, Thompson DG. Awareness of dysphagia by patients following stroke predicts swallowing performance. Dysphagia. 2004;19(1):28-35.
10. Horner J, Alberts MJ, Dawson DV, Cook GM. Swallowing in Alzheimer’s disease. Alzheimer Dis Assoc Disord. 1994;8(3):177-189.
11. Kalf JG, de Swart BJ, Bloem BR, Munneke M. Prevalence of oropharyngeal dysphagia in Parkinson’s disease: a meta-analysis. Parkinsonism Relat Disord. 2012;18(4):311-315.
12. Zargaraan A, Rastmanesh R, Fadavi G, Zayeri F, Mohammadifar MA. Rheological aspects of dysphagia-oriented food products: a mini review. Food Sci Hum Wellness. 2013;2(3-4):173-178.
13. Garcia JM, Chambers E, Molander M. Thickened liquids: practice patterns of speech-language pathologists. Am J Speech Lang Pathol. 2005;14(1):4-13.
14. Steele C, Van Lieshout PH, Goff HD. The rheology of liquids: a comparison of clinicians’ subjective impressions and objective measurements. Dysphagia. 2003;18(3):182-195.
15. Ekberg O, Hamdy S, Woisard V, Wuttge-Hannig A, Ortega P. Social and psychological burden of dysphagia: its impact on diagnosis and treatment. Dysphagia. 2002;17(2):139-146.
16. Leiter AE, Windsor J. Compliance of geriatric dysphagic patients with safe-swallowing instructions. J Med Speech Lang Pathol. 1996;4(4):289-300.
17. Chen PH, Golub JS, Hapner ER, Johns MM 3rd. Prevalence of perceived dysphagia and quality of life impairment in geriatric population. Dysphagia. 2009;24(1):1-6.
18. Brody R. Nutrition issues in dysphagia: identification, management and the role of the dietician. Nutr Clin Pract. 1999;14(5):547-551.
19. Low J, Wyles C, Wilkinson T, Sainsbury R. The effect of compliance on clinical outcomes for patients with dysphagia on videofluoroscopy. Dysphagia. 2001;16(2):123-127.
20. Adeleye B, Rachal C. Comparison of the rheological properties of ready-to-serve and powdered instant food-thickened beverages at different temperatures for dysphagic patients. J Am Diet Assoc. 2007;107(7):1176-1182.
21. Biggs LR, Cooper LC, Garcia JM, Chambers E. Viscosity comparison of thickened juices at two and ten minute intervals. Undergraduate Research Journal for the Human Sciences. 2003;2:1-7.
22. Pelletier CA. A comparison of consistency and taste of five commercial thickeners. Dysphagia. 1997;12(2):74-78.
23. Leonard RJ, White C, McKenzie S, Belafsky PC. Effects of bolus rheology on aspiration in patients with dysphagia. J Acad Nutr Diet. 2014;114(4):590-594.
24. Samargia SA, Economy K. Alternatives to traditional thickened liquids to improve compliance in patients with dysphagia. Paper presented at: American Speech-Language-Hearing Association Convention; November 14, 2013; Chicago, IL.
25. Samargia SA, Fraser K. Patient compliance in dysphagia management: which thickening agent is most palatable? Paper presented at: The Minnesota Speech-Language-Hearing Association Convention; April 10, 2015; Minnetonka, MN.


