Today’s Dietitian
Vol. 19, No. 2, P. 32
Nutrition support therapy has the power to reduce disease severity, complications, and length of ICU stays, but appropriate and safe administration is essential to achieving the best patient outcomes.1 Updated guidelines and new recommendations for enteral nutrition (EN) and parenteral nutrition (PN) were recently released, and important new safety features and nutritional products are now available. As key members of the nutrition support team, dietitians must be aware of these changes.
New Guidelines
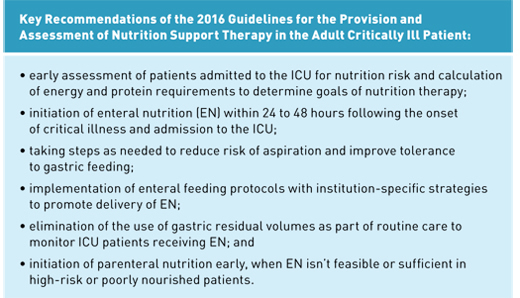
In January 2016, the American Society for Parenteral and Enteral Nutrition (ASPEN) and the Society of Critical Care Medicine (SCCM) released new guidelines for the provision and assessment of nutrition support therapy in critically ill adult patients. “Appropriate nutrition support therapy can improve clinical outcomes for medical and surgical patients in the ICU,” says Ainsley Malone, MS, RD, LD, CNSC, FAND, FASPEN, a member of the nutrition support team at Mt. Carmel West Hospital in Columbus, Ohio, and a clinical practice specialist with ASPEN. “The authors used evidence on positive clinical outcomes to provide recommendations that guide best practice in nutrition care for critically ill patients.” The guidelines address nutrition assessment; initiation, dosing, and monitoring of EN; EN formula selection; adjunctive therapy (eg, fiber, probiotics, antioxidant vitamins, minerals, and glutamine); when to use PN; and how to maximize PN efficacy. They also include recommendations on the treatment of specific conditions (eg, pulmonary, renal, and hepatic failure; pancreatitis; and sepsis) and patient populations (eg, postsurgical, the chronically critically ill, the obese, and end-of-life situations).1 “The Guideline recommendations can help RDs make practice decisions for nutrition care of the ICU patient at the bedside,” Malone says, “and they can be incorporated into procedures utilized by the whole health care team.”
The 2016 guidelines contain some significant changes over the previous guidelines, issued in 2009. In addition to nutrition status, the guidelines recommend disease severity be taken into account when performing a nutrition assessment. Two assessment tools, Nutrition Risk Screening (NRS 2002) and NUTRIC (Nutrition Risk in Critically Ill) are recommended. With regard to EN formula selection, the new guidelines recommend the use of standard polymeric formula for patients receiving EN in the ICU. The 2009 recommendation to use omega-3 specialty formulas in acute respiratory distress syndrome and acute lung injury patients has been eliminated based on conflicting data in more recent studies. However, immune-modulating enteral formulas containing both fish oil and arginine may decrease hospital length of stay and reduce infections, and are recommended for postoperative surgical ICU patients requiring EN.1,2
The 2016 guidelines also offer some new information on monitoring EN. The biggest change involves the measurement of gastric residual volumes (GRVs). Citing evidence that eliminating the measurement of GRVs improves delivery of EN without jeopardizing patient safety, the guidelines suggest that GRVs not be used as part of routine care to monitor patients in the ICU receiving EN. If GRVs continue to be used, it’s recommended that, unless there are other signs of intolerance, EN orders be placed on hold only if GRV is greater than 500 mL.1,2
The guidelines also state that protein is the key macronutrient for ICU patients, and diet should be evaluated regularly to ensure adequate protein intake. The new recommended blood glucose level for the general ICU patient population is 140 to 180 mg/dL, according to ASPEN, and 150 to 180 mg/dL, according to SCCM.1 (For more details about the new guidelines, read “Nutrition Support for the Critically Ill,” in the September 2016 issue of Today’s Dietitian.)
While the adult critical care guidelines state that using alternative intravenous lipid emulsions in PN may lead to better outcomes than soy-based emulsions, they were unable to make a recommendation regarding alternative lipid sources, since there were no such products on the market.1 With the FDA approval of Smoflipid in July 2016, an alternative oil-based IV lipid emulsion, this circumstance has changed.
Alternative IV Lipid Emulsion Approved for PN
Smoflipid, manufactured by Fresenius Kabi, is a mix of 30% soybean oil, 30% medium-chain triglyceride oil, 25% olive oil, and 15% fish oil.3 It has been used in other global markets for many years.4
The new SCCM/ASPEN guidelines for nutrition support in critically ill adults state that alternative lipid emulsions derived from sources other than soybean oil “provide a component that may improve the risk/benefit ratio for PN,” and suggest that they be considered for use in critically ill patients requiring PN.1
According to an August 2016 product review in Nutrition in Clinical Practice, the soybean oil-based lipid emulsions used in the United States have certain limitations: They can’t be used in patients allergic to soy; they may play a role in the development of PN-associated liver disease; and they’re linked with inflammatory effects related to their fatty acid profile. Soybean oil-based lipid emulsions are high in potentially proinflammatory omega-6 fatty acids and have been shown in several studies to increase serum inflammatory markers within hours following administration. However, the omega-3 fatty acids provided by the fish oil in Smoflipid tip the omega-6:omega-3 fatty acid ratio to 2.5:1, which is believed to be less proinflammatory than the 7:1 ratio in soybean oil-based emulsions.3,5 It should be noted, however, that the prescribing information for Smoflipid is required to state, “the omega-6:omega-3 fatty acid ratio and medium-chain triglycerides in Smoflipid have not been shown to improve clinical outcomes compared to other intravenous lipid emulsions.”3
Smoflipid has the same safety and efficacy profile as the commonly used Intralipid and may have an increased triglyceride clearance rate.5 “I’m looking forward to having another lipid option available for use in those populations where 100% soybean oil emulsions may not be beneficial,” Malone says. “This alternative lipid will be a desirable choice for critically ill patients as well as those who require long-term parenteral nutrition support.” Smoflipid is contraindicated in those with hypersensitivity to fish, egg, soybean, or peanut protein, or to any of its ingredients, and with severe hyperlipidemia or severe disorders of lipid metabolism with serum triglycerides greater than 1,000 mg/dL.6
According to the prescribing information, the usual daily dosage in adults is 1 to 2 g/kg per day and shouldn’t exceed 2.5 g/kg per day.6 Smoflipid has a lipid content of 0.2 g/mL in 100 mL, 250 mL, and 500 mL bags.6 There are 0.163 to 0.225 mg of vitamin E (alpha-tocopherol) per mL of Smoflipid, which should be taken into account when determining the need for supplementation (the Recommended Dietary Allowance for alpha-tocopherol is 15 mg).6
“RDs need to know when using an alternative lipid source may be beneficial and also how to meet essential fatty acid requirements with this new lipid formulation,” says Liz Zorzanello Emery, MS, RD, LDN, CNSC, an assistant professor and director of the coordinated program in dietetics at La Salle University School of Nursing and Health Sciences. More information is available at www.smoflipid.com.
Safe Practices for EN Therapy
In November 2016, ASPEN released new EN safe practice recommendations. “These recommendations promote the safe delivery of enteral nutrition and were developed entirely with this theme in mind,” Malone says.
Peggi Guenter, PhD, RN, FAAN, senior director of clinical practice, quality, and advocacy for ASPEN, emphasizes that these aren’t just an update of the 2009 practice recommendations. “Our goal is decreasing adverse events across the process,” Guenter says. With that goal in mind, the recommendations propose best practices for each step involved in EN therapy, including patient assessment, prescribing and treatment plan implementation, review and communication with the nutrition and patient support teams, placement of enteral devices and medication delivery, administration and documentation standardization, monitoring and error reporting protocols, and transition of care.7
“We tried to cover all of the processes that anyone would run into in all health care settings, not just hospitals,” Guenter continues. The recommendations are built around a question-and-answer format. “We pose a question, then offer basic practice recommendations, the rationale behind them, and areas for future research,” Guenter says. Some new topics addressed in these recommendations include the use of electronic health records throughout the process and safety issues related to the increasing popularity of blenderized diets. Like the guidelines for critically ill patients, the new EN safety recommendations support less use of GRVs.7
“RDs are key clinicians in the enteral nutrition process and should utilize these enteral nutrition practice recommendations to promote patient safety and maximize the benefits of enteral nutrition to their patients,” Malone says.
The complete ASPEN Safe Practices for Enteral Nutrition Therapy is available at the ASPEN website, nutritioncare.org.
Introducing ENFit Connectors
In accordance with new International Organization for Standardization (ISO) standards, the connectors used to administer EN therapy have changed. Until recently, connectors used where tubing enters a patient’s body were interconnectable. This uniformity raised the risk of dangerous, potentially fatal misconnections.8 “Although RDs aren’t typically responsible for connecting feeding tubes, they need to be aware of the safety concerns associated with enteral misconnections,” Emery says.
The ISO created standards for all small-bore connectors and decided that each therapeutic need should have its own connector. “In addition to the new enteral connectors, there will be different connectors for IV, blood pressure, neuraxial procedures like epidurals, respiratory needs like ventilators and oxygen, and urology in the future,” Guenter says. While the new enteral connector will be available from multiple manufacturers, the Global Enteral Device Supplier Association (GEDSA) has chosen to brand the product ENFit to encourage all companies to use the same name.8
Companion products have now been developed to support the transition to ENFit, such as new compatible low-dose syringes, transition sets to allow the ENFit tubing to be used for patients with connectors installed before the change, and adaptors to fit drainage bags.9 While the pressure and flow rate is basically the same as the catheter-tip syringes used previously when using standard formulas with ENFit, independent testing is currently being done on home blenderized diets, Guenter says. “They may flow more slowly depending on the thickness of the feeding,” she says, “so the FDA and an independent academic laboratory are currently testing a wide variety of formulas.
“While many issues around connectors are nursing issues, dietitians need to be aware that this transition is happening,” Guenter continues. “They can be integral to improving patient care and safety. For example, I see a very important role for RDs in the transition of care: By being aware of what kind of tube a patient has, particularly when examining them before discharge, RDs can help ensure home care or other agencies know what kind of equipment this patient might need.” At the hospital where Malone works in nutrition support, the transition to ENFit already has impacted practice for her and her colleagues. “We have needed to stay abreast of the implementation timeline and work with our pharmacy and nursing colleagues to assist with education and implementation,” Malone says.
Not all providers are transitioning to the new products immediately. “The FDA doesn’t have a hard and fast deadline for when the changeover needs to be complete,” Guenter says. “Companies are still stocking legacy product. Some hospitals are doing a total changeover, but some are waiting for old stock to be used up.”
It’s important for RDs to understand the effects of this transition. “RDs may be part of a management team that makes decisions on the types of enteral devices and tubings available in their facility,” Emery says. “They also are involved in patient teaching both in the hospital and at home. They need to be able to recognize potential problems with enteral connections and work with their team to provide the safest and most effective care possible.”
“This exciting new product will be a leap forward in enteral nutrition safety,” Guenter says. “This is happening, and we need to be prepared.” For more information, go to StayConnected.org, a website set up by GEDSA to keep practitioners updated on all connector modifications.
With all of these changes in the world of nutrition support therapy, it’s important for RDs to stay informed and up to date. “Registered dietitians work as a part of an interprofessional team to deliver optimal nutrition support in a safe and timely manner to patients,” Emery says. “Being aware of safety recommendations and critical care guidelines is an essential first step in demonstrating the proficiency needed to recommend, order, and manage enteral and parenteral nutrition support,” Emery adds. “Safety, professionalism, and constant improvement are prerequisites for competent practice and for maintaining standards of practice at a proficient or expert level.”
— Judith C. Thalheimer, RD, LDN, is a freelance nutrition writer, a community educator, and the principal of JTRD Nutrition Education Services, LLC.
References
1. McClave SA, Taylor BE, Martindale RG, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parental and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2016;40(2):159-211.
2. Corrigan ML. New guidelines on nutrition support for the critically ill. Today’s Geriatr Med. 2016;9(6):8-9.
3. Smoflipid. Fresenius Kabi website. http://smoflipid.com/smoflipid-composition.html
4. Smoflipid approved by FDA and available in US. American Society for Parenteral and Enteral Nutrition website. http://www.nutritioncare.org/News/General_News/Smoflipid%C2%AE_Approved_by_FDA_and_Available_in_US/
5. Biesboer AN, Stoehr NA. A product review of alternative oil-based intravenous fat emulsions. Nutr Clin Pract. 2016;31(5):610-618.
6. US Food and Drug Administration. Highlights of prescribing information: Smoflipid. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/207648lbl.pdf. Published May 2016.
7. ASPEN releases new enteral nutrition safe practice recommendations. American Society for Parenteral and Enteral Nutrition website. http://www.nutritioncare.org/News/General_News/ASPEN_Releases_New_Enteral_Nutrition_Safe_Practice_Recommendations/. Published November 7, 2016.
8. Guenter P, Lyman B. ENFit enteral nutrition connectors: benefits and challenges. Nutr Clin Pract. 2016;31(6):769-772.
9. Global Enteral Device Supplier Association. ENFit enteral system connector changes. http://stayconnected.org/wp-content/uploads/2016/10/GEDSA-Stayconnected-Checklist-1-page.pdf


