Today’s Dietitian
Vol. 17 No. 2 P. 50
Suggested CDR Learning Codes: 4000, 4040, 5150; Level 2
Take this course and earn 2 CEUs on our Continuing Education Learning Library
The largest organ in the human body, skin serves as an outer layer of protection, defending the body against light, extreme heat or cold, injury, and infection and also regulating water and lipid stores and body temperature. Both external influences (eg, sun exposure) and internal influences (eg, an individual’s nutritional status) can compromise the skin’s ability to perform these functions and can lead to cutaneous diseases such as skin cancer, or the abnormal growth of skin cells. Skin cancer is the most common form of cancer in the United States, affecting nearly one in five Americans. In recent years, skin cancer has been diagnosed more than all other types of cancers combined.1
Basal cell carcinoma (BCC), the most common type of skin cancer, rarely is fatal. Basal cells are located beneath squamous cells and are responsible for the production of new skin cells.
Actinic keratosis is a common precancerous scaly growth or lesion that strongly predicts all major types of skin cancer, with nearly 10% of actinic keratoses leading to squamous cell carcinoma (SCC). SCC is the second most common type of skin cancer.2 Squamous cells lie just below the skin’s surface (epidermis) and function as its inner lining. Fortunately, there was a 98% survival rate among SCC patients in the United States in 2012.1
Melanocytes are located in the lower part of the epidermis and produce the pigments that give skin its unique color. Cancer of melanocytes, or melanoma, is the rarest type of skin cancer, accounting for less than 5% of all cases, but it’s also the most dangerous and most fatal.1 If detected early, the survival rate for melanoma is 98%, but once it metastasizes or spreads to the lymph nodes, the survival rate drops to 62%.1 The average age at which melanoma is diagnosed is 63 for men and 56 for women.3
From an economic standpoint, skin cancer costs American taxpayers millions in health care dollars. In 2008, allowable charges paid to physicians by Medicare Part B for skin cancer treatment was nearly $633 million, a 137% increase from 1996.4
There are several well-established risk factors for skin cancer. The disease is more prevalent in individuals who have fair skin, light eyes, or light hair, possibly because their skin contains less melanin (color pigmentation), which serves as a protective layer from ultraviolet (UV) radiation. Other risk factors include having a family history of skin cancer; having a history of erythema (sunburns); living in sunny, warm climates or at higher elevations where UV rays are the strongest; and having abnormal moles, called dysplastic nelvi, that are irregular in shape and larger than regular moles.
One of the most prominent risk factors for skin cancer is excessive sun or UV exposure. UV radiation can induce premature aging and DNA damage and can act as a tumor initiator to the skin.5 Nearly 90% of nonmelanoma skin cancers are associated with exposure to UV radiation from the sun.1
One of the lesser-known methods for potentially lowering skin cancer risk is diet. There’s promising evidence that dietary interventions may benefit individuals who are at high risk of skin carcinoma. This continuing education course evaluates the current research on dietary interventions that may affect the risk of developing skin cancer and analyzes the possible mechanisms involved with the disease.
Plant-Based Diet
A plant-based diet rich in antioxidants has been associated with a reduced risk of many types of cancers, such as those of the lung, mouth, throat, stomach, and colon. For other types of cancers, evidence is limited or inconsistent.
Unfortunately, the majority of Americans don’t consume adequate amounts of fruits and vegetables. In fact, only 14.8% to 19.1% of skin cancer survivors are meeting the American Cancer Society’s recommendation to consume at least five servings (or 21/2 cups) of fruits and vegetables each day.6
Because of this deficiency, vitamin and mineral supplementation may seem like a viable alternative. However, the American Cancer Society also recommends choosing whole foods over dietary supplements since there are many still-unidentified components of fruits and vegetables that haven’t been condensed into pill form.7 Table 1 lists some antioxidants and their food sources.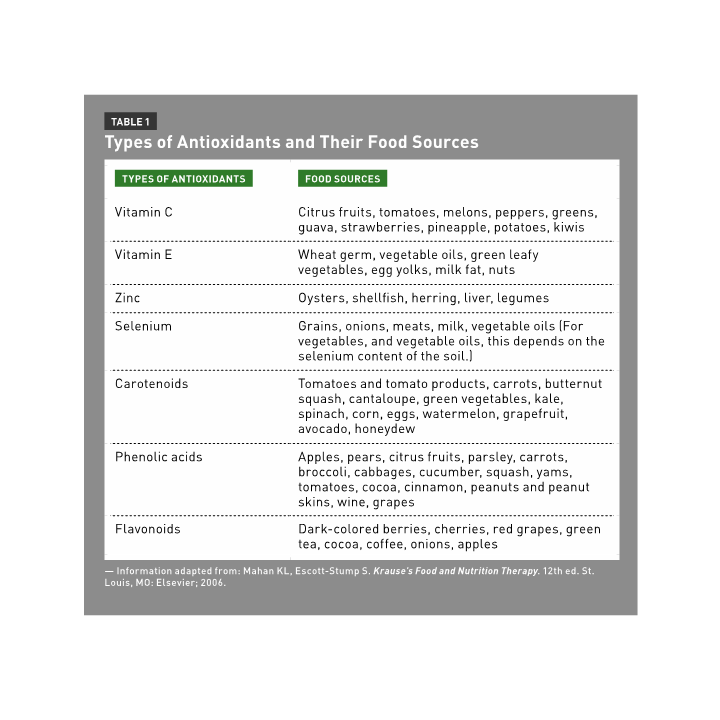
In a 10-year prospective study, subjects who consumed the highest percentage of fruits and vegetables had a 54% reduced risk of SCC. In particular, eating green leafy vegetables was associated with decreased risk. However, the study found that no dietary pattern was associated with BCC tumors.8
Another study asked patients who were newly diagnosed with melanoma to complete a food frequency questionnaire. High intake of the following micronutrients was associated with a significantly reduced risk of melanoma compared with low intake: vitamins C and D, retinol (vitamin A), alpha- and beta-carotene, cryptoxanthin, lutein, and lycopene. Compared with the lowest tertiles, high daily intake of the following food groups were associated with a significantly reduced risk of melanoma:9
• Fruits/fruit juices: 1.6 or more servings;
• Vegetables: 1.1 or more servings;
• Fruits and vegetables combined: 2.1 or more servings;
• Citrus fruits and juices: 0.6 or more servings;
• Dark green/yellow fruits and vegetables: 0.5 or more servings; and
• Fish: 0.3 or more servings.
In another study, regular consumption (three or more servings per week) of celeriac and pomegranates was associated with a significantly reduced risk of BCC and SCC. Celeriac, more commonly known as celery root, also was associated with a significantly reduced risk of melanoma. Parsnips, red wine, and red berries, however, were associated with an increased risk of melanoma. These results were adjusted for age, sex, skin reaction to the sun, and country of origin.10
Antioxidants found in fruits and vegetables function by eliminating free radicals and reactive oxygen species that can attack DNA and lead to diseases. Vitamins C and E are abundant nutrients in plants that act as antioxidants and may help protect against skin cancer. Vitamin C scavenges free radicals and restores the activity of other antioxidants, enhances the immune system, and hydroxylates lysine and proline in the synthesis of connective tissues proteins, which may alter tumor growth. Vitamin E is an intracellular antioxidant that prevents lipid peroxidation.11
Plant Components
Vitamin A
Due to its antioxidant properties, vitamin A is sometimes referred to as the “oral skin protectant.” It’s a fat-soluble vitamin that can be consumed in the form of retinols from animal products such as eggs, milk, and liver as well as from plants in the form of alpha- and beta-carotene. Beta-carotene is efficiently converted into retinol, whereas only one-half of alpha-carotene is converted into retinol.
Vitamin A performs many important biological functions, including those involved with vision, reproduction, and immune regulation. Vitamin A also is essential in skin cell proliferation, differentiation, and maintenance and may decrease the amount of UV light that reaches the underlying layers of the skin by increasing epidermal thickness.3
Carotenoid consumption through food and supplements has been shown to decrease the risk of skin cancer. In one study, subjects consumed a 25-mg carotenoid supplement or the same carotenoid supplement plus alpha-tocopherol (vitamin E) daily for 12 weeks. UV light irradiation was used to induce erythema in a small area of the skin. Erythema is redness of the skin and is commonly used in scientific studies as an indicator of sunburn reaction. Researchers found that erythema induced by UV light was significantly reduced in both treatment groups compared with the placebo group, with the greatest photoprotective effect found in the combination of carotenoids plus alpha-tocopherol.12
In a similar study, supplementation with 24 mg of beta-carotene or 24 mg of a mixture of carotenoids daily for 12 weeks were both shown to have photoprotective effects by decreasing UV-induced erythema in human skin, providing protection against exposure to UV radiation.13
In contrast, some studies in which subjects were given carotenoid supplements resulted in no differences in carotenoid-dependent protection against UV radiation.14-16
Lycopene is the major carotenoid in tomatoes and tomato products. It acts as an antioxidant against photo-oxidative stress. Lycopene is more bioavailable from tomato products than from tomato juice or fresh tomatoes. In a study by Stahl and colleagues, nine subjects consumed 40 g of tomato paste for 10 weeks; the paste contained about 16 g of lycopene, 0.5 mg of beta-carotene, and 0.1 mg of lutein. Results found that tomato paste consumption significantly decreased erythema formation by 40% at 10 weeks compared with controls.17
A double-blind, placebo-controlled study found supplementation with retinol (25,000 IU) significantly reduced the incidence of SCC but not BCC.18 However, a large prospective study found no association with melanoma and dietary carotenoid or retinol intake through food or the combination of supplement and dietary intake.19
One potential mechanism by which carotenoids may inhibit skin carcinogenesis is their antioxidant abilities; beta-carotene enhances immune system functioning, while provitamin A carotenoids may prevent skin cancer through its conversion to retinoids.11 However, there are some concerns about the safety of extremely high doses of carotenoid supplementation due to the results of the Beta-Carotene and Retinol Efficacy Trial, which revealed increased lung cancer incidence and mortality among smokers consuming supplemental beta-carotene. Authors suspect high doses of beta-carotene can act as pro-oxidants and result in secondary reactive oxygen species.20
Flavonoids
Flavonoids are naturally occurring compounds found in fruits and vegetables as well as cocoa, tea, and red wine. More than 5,000 types of flavonoids have been identified and are commonly classified into the following subgroups: anthoxanthins (flavones and flavonols), flavanones, flavanonols, flavanols, and anthocyanidins. These compounds have been found to have antioxidant properties that may be beneficial in the prevention of many types of cancers.
Quercetin
Quercetin, a common flavonoid found in fruits and vegetables such as onions, kale, and broccoli, has many antioxidant and anticarcinogenic properties. In one study, mice fed a quercetin-rich diet had delayed skin tumor development, reduced skin tumor growth, and decreased tumor number and size. Scientists attribute these results to quercetin-fed mice having suppressed insulin-like growth factor-1 (IGF-1) signaling, a protein that regulates cell proliferation, growth, and apoptosis.21
Apigenin
Apigenin is a flavone that naturally occurs in fruits such as oranges and grapefruits; vegetables such as onions; herbs such as parsley, chamomile, and wheat sprouts; some seasonings; and plant-based drinks such as tea. Studies have shown that apigenin is effective in reducing skin carcinogenesis by suppressing cyclooxygenase-2 (COX-2) expression and mRNA in mouse and human skin lines. COX-2 is a key enzyme in which overexpression results in carcinogenesis.22
Flavanols
In one study, a group of women drank a high flavanol drink made from cocoa powder (326 mg of total flavanols, mostly epicatechin and catechins), comparable to about 100 g of dark chocolate, while another group drank a low flavanol drink (27 mg). After a small area of skin was exposed to UV light, results found that the high-flavanol group had significantly decreased erythema: 15% after six weeks of treatment and 25% after 12 weeks of treatment. This may indicate that the flavanols found in small amounts of cocoa and dark chocolate may reduce the severity of a sunburn and thus could reduce the risk of skin cancer development. However, this was a small study with only 12 subjects in each treatment group.23
Mediterranean Diet
The Mediterranean diet, which refers to the dietary patterns of European societies located near the Mediterranean Sea and traditionally consists of fruits, vegetables, fish, olive oil, wine, and fresh herbs, has been shown to lower the risk of overall mortality. For every two-point increase in the score of adherence to a Mediterranean diet, the relative risk of overall mortality decreases by 8%.24 However, there have been only a limited number of scientific studies regarding the association between the Mediterranean diet and skin cancer risk.
In one case-control study in a hospital in Rome, 304 patients newly diagnosed with melanoma and 305 control subjects were asked to complete a food frequency questionnaire. After controlling for several confounding factors, such as medical history, sun exposure, and skin pigmentation, results showed that those who consumed a typical Mediterranean diet had a lower incidence of melanoma.
Consuming fruits, vegetables, tea, fish, shellfish, and fish rich in omega-3 fatty acids was found to have a protective effect. Fish rich in omega-3 fatty acids include sardines, anchovies, tuna, and salmon. The consumption of cooked vegetables (more than five times per week), cruciferous vegetables (more than three times per week), green leafy vegetables (three times per week), fruits (more than once daily), citrus fruits (more than five times per week), and the use of fresh herbs (four or more regularly) was significantly associated with a decreased risk of melanoma.25
Fat and Red Meat
Many epidemiologic studies have suggested that excessive consumption of red and processed meats is associated with an increased incidence of cancer and risk of all-cause mortality. Processed meats include bacon, sausage, luncheon meats, and hot dogs, and red meats include beef, pork, and lamb. Meat can contain several carcinogens that may raise cancer risk, including heterocyclic amines, polycyclic aromatic hydrocarbons (produced by high temperate/charcoal cooking), and nitrates and nitrites (used as preservatives).7
A high-fat diet has been shown to contribute to oxidative stress, DNA damage, increased inflammatory cytokines in the skin, and decreased cell apoptosis. A high-fat diet may enhance skin carcinogenesis by influencing the composition of cell membrane lipids and intercellular communication.11
There’s suggestive evidence that a high-fat diet and high intakes of red meat and processed meats are associated with skin cancer. One study showed a trend, though not statistically significant, for melanoma with increasing consumption of total fat as a percent of calories and a significant trend for melanoma with increasing consumption of saturated fat and linoleic acid as a percent of calories.9
In a 10-year prospective study, higher consumption of meat and fat was associated with a significantly greater risk of developing SCC. The meat and fat food groups included red meats, processed meats, discretionary fat (habitual consumption of fried foods and visible fat on meat), processed grains, junk food snacks, sweet drinks, and high-fat dairy products. In particular, the consumption of high-fat dairy was associated with an increased risk of SCC.8 Several studies have shown that dairy consumption is positively associated with increased IGF-1 expression, which may induce SCC.26 The risk ratio of developing SCC, after adjustment for multiple variables, from the lowest, median, and highest tertile groups of high-fat dairy was 1, 1.84, and 2.38, respectively.8 However, a case-control study found no association of skin cancer with the consumption of meat, cheese, butter, eggs, or milk.25
A longitudinal study demonstrated that individuals who consumed the highest amounts of eggs and pizza had a 45% and 37% increased risk of actinic keratoses, respectively.27
To investigate nutritional counseling regarding the effects of a low-fat diet on skin cancer risk, more than 48,000 postmenopausal women were randomized to a control or dietary intervention group. The dietary intervention included several educational sessions in which nutritionists educated subjects on how to decrease total fat intake to less than 20% of total calories, consume five or more daily servings of vegetables, and consume six or more daily servings of grains.28
After an eight-year follow-up, there were no differences in the incidence of melanoma or nonmelanoma skin cancer between the two groups of women. Even after sensitivity analysis, in which participants who may not have fully complied with the trial requirements were excluded, there still was no association between the low-fat intervention and skin cancer risk.28
In another study, a significantly lower risk of nonmelanoma skin cancer was found in the intervention group following a diet consisting of 21% of calories from fat. The groups successfully maintained the low-fat diet throughout the two-year study. The dietary intervention included weekly and monthly classes in which a dietitian educated subjects about decreasing fat intake by modifying recipes and food preparation techniques, choosing low-fat food options, increasing complex carbohydrates, and increasing fruit and vegetable intake. Because of this increase in fruit and vegetable consumption, dietary analysis revealed vitamin C, beta-carotene, and fiber intake was significantly higher in the intervention group compared with control subjects.29 However, maintaining total fat consumption of less than 20% of calories may be difficult since Americans typically consume an average of 34% of calories from fat.30
Omega-3 Fatty Acids
There’s strong evidence that omega-3 polyunsaturated fatty acids (PUFAs), more specifically the ratio between omega-3 and omega-6 fatty acids, have a protective effect on overall cancer risk. The primary omega-3 fatty acids include EPA (20:5-n3) and DHA (22:6-n3). Omega-3 fatty acids commonly are found in fatty fish such as salmon and mackerel, and the USDA recommends consuming about two servings of fish per week, with an emphasis on fatty fish.30
In a longitudinal study, individuals who consumed the highest amounts of oily fish (one serving every five days) had a 28% lower risk of actinic keratosis.27 In a meta-analysis of five research studies, dietary omega-3 consumption wasn’t associated with BCC.31 High levels of omega-3 PUFAs were inversely associated with SCC, but the association wasn’t statistically significant.31 However, Fortes and colleagues found the consumption of fish, shellfish, and fish rich in omega-3 fatty acids was significantly associated with a decreased risk of melanoma.25
In a population, case-control study in Arizona, there was a trend of lower SCC risk with higher omega-3 fatty acid intake but no significant associations between SCC and total energy, fat, and cholesterol intake. There also was a consistent pattern for lower SCC risk with increasing intakes of EPA, DHA, and arachidonic acid, but these results weren’t statistically significant. The protective effect against SCC also was found with increasing omega-3 to omega-6 ratios.32
In a small study of 20 subjects, 4 g/day of fish oil supplementation (containing 2.8 g of EPA and 1.2 g of DHA) for four weeks was associated with a small but statistically significant increase in minimal erythema dose compared with a placebo. Minimal erythema dose is known as the minimum amount of UV exposure that produces sunburn.33
Potential mechanisms by which omega-3 fatty acids may prevent skin carcinogenesis include COX-2 inhibition (high levels are found during inflammation), prostaglandin synthesis deregulation, membrane fluidity alterations, transcription factor activation, and oxidative stress modulation.25,34
Coffee and Caffeine
In one study, caffeine intake from all dietary sources was inversely associated with BCC risk but not SCC or melanoma risk. After adjusting for multiple variables, individuals who drank more than three cups of coffee per day had the lowest risk of BCC compared with individuals who drank less than one cup per month. The consumption of caffeinated coffee (100 mg/day) was associated with a decreased risk of BCC, but decaffeinated coffee didn’t have this effect. Caffeine (100 mg/day) from other dietary sources, such as tea, cola, and chocolate, wasn’t significantly associated with a decreased risk of BCC. The authors suggested that caffeine might promote elimination of UV-damaged keratinocytes via apoptosis.35
In a study of more than 50,000 individuals, coffee consumption was associated with a decreased risk of melanoma in women but not in men.36 A 36% decrease in nonmelanoma skin cancer was found in women who drank six or more cups of coffee per day compared with nondrinkers.37
In a population from the southwestern United States, no association was found between tea consumption and SCC. However, adjusted odds ratios for hot tea and iced black tea were 0.63 and 1.02, respectively. After adjustment for brewing time, a significant association was found for hot tea consumption and a decreased risk of skin SCC compared with nontea drinkers.38
In a rodent study, the administration of green tea and caffeine has been found to inhibit UVB-induced carcinogenesis in mice. The cancer-preventing caffeine doses in mice were considered equivalent to two to five cups of coffee per day in humans. Green tea, caffeinated coffee, and a caffeine solution, but not decaffeinated green tea, significantly increased apoptosis of the UVB-treated skin.39
Alcohol
While moderate alcohol consumption has been associated with a lower risk of cardiovascular disease, heavy or excessive drinking has been well established as increasing the risk of mouth, throat, liver, colon, and female breast cancers.7 Heavy drinking for women is defined as more than three drinks per day or more than seven per week, and for men is more than four drinks per day or 14 per week.30
There have been mixed results regarding alcohol consumption and skin cancer. In one study, the risk of melanoma was significantly increased in those who consumed 1.4 or more alcoholic drinks per week compared with nondrinkers.9 On the other hand, in a population, case-control study of men from Montreal, Canada, no significant association was found between excessive alcohol consumption and melanoma risk. Interestingly, of the men with melanoma, 31.8% reported drinking one to six alcoholic beverages per week, and 48.6% reported drinking seven or more per week.40 Another study found that regular alcohol use was associated with a significantly increased risk of BCC and melanoma but not of SCC.10
On the other hand, it also has been suggested that individuals who consumed the highest amounts of wine had a 27% decrease in actinic keratoses compared with the lowest consumers. The highest consumers drank an average of one half-glass of wine every day. There was no association with beer or spirits consumption with actinic keratoses.27
In a large Danish study of more than 50,000 people, there was no association between cumulative alcohol intake and the risk of SCC and BCC, but the specific type of alcoholic beverage did appear to play a role. A dose-responsive effect for wine and spirits was found to be associated with BCC, whereas beer consumption was found to be inversely associated with BCC. The authors concluded that alcohol may promote skin cancer by interfering with normal DNA replication and mitosis in the skin, altering oncogenes and tumor-suppressor genes, inducing skin inflammation, and enhancing the accumulation of UV-damaged cell DNA and mutations. In addition, the by-product of ethanol metabolism, acetaldehyde, is believed to be carcinogenic.41
Practice Applications
For clients and patients who want to protect themselves from harmful UV rays, it’s important to emphasize environmental protection from the sun, such as using sunscreen and wearing protective clothing. However, a secondary line of defense from the sun’s harmful UV rays may be diet related.
Research shows dietary factors may play a role in the prevention of skin cancer in both rodents and humans. However, the results of these research studies are mixed and conflicting. A plant-based diet rich in fruits and vegetables and low in fat has shown promising results in altering skin cancer development. The American Cancer Society recommends consuming at least five servings of fruits and vegetables per day for overall cancer prevention. Dietitians can recommend that clients and patients increase their intake of the foods listed in Table 2 and also suggest decreasing fat intake to less than 20% of calories.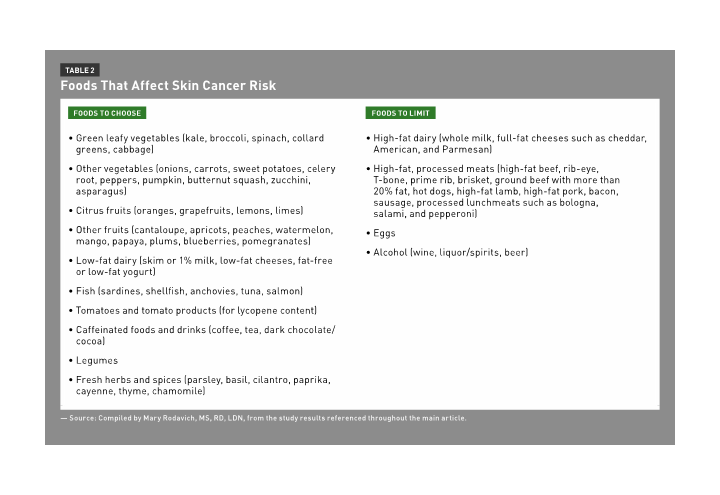
Another beneficial strategy for dietitians is to have clients and patients keep a food diary or complete a food frequency questionnaire. If certain nutrients through food sources are lacking, such as vitamin A and omega-3s, clients and patients may want to consider supplementation, and dietitians can provide guidance.
The dietary strategies with implications in skin cancer prevention also are conducive to an overall healthful lifestyle. A diet high in fruits and vegetables and low in fat may prevent other types of cancers and chronic diseases such as obesity, heart disease, and diabetes, and therefore have an added benefit above skin cancer prevention.
— Mary Rodavich, MS, RD, LDN, is a clinical dietitian and freelance writer based in Pittsburgh.
Learning Objectives
After completing this continuing education course, nutrition professionals should be better able to:
1. Differentiate among the different types of skin cancers and identify risk factors for the disease.
2. Evaluate proposed dietary interventions that may affect skin cancer risk.
3. Advise patients about which foods to choose to reduce skin cancer risk and address the mechanisms involved in its development.
Examination
1. What is the most fatal type of skin cancer?
a. Actinic keratosis
b. Squamous cell
c. Basal cell
d. Melanoma
2. Which of the following is a major risk factor for skin cancer?
a. Living at lower elevations
b. Dark skin, eyes, and hair
c. Younger age
d. Excessive sun exposure
3. Skin cancer is the most common form of cancer in the United States.
a. True
b. False
4. The American Cancer Society recommends at least how many servings of fruits and vegetables per day for cancer prevention?
a. Three
b. Four
c. Five
d. Six
5. In a case-control study of the Mediterranean diet, which food (or foods) didn’t protect against skin cancer?
a. Fatty fish
b. Meat, eggs, and milk
c. Fruits and vegetables
d. Fresh herbs
6. A low-fat diet may increase the risk of skin cancer because it may contain several carcinogens and has been shown to contribute to oxidative stress, DNA damage, increased inflammatory cytokines in the skin, and decreased cell apoptosis.
a. True
b. False
7. For skin cancer prevention, research has suggested that fat should be limited to less than what percentage of calories?
a. 15
b. 20
c. 25
d. 30
8. What component of tomatoes positively affects skin cancer risk?
a. Lycopene
b. Vitamin A
c. Vitamin C
d. Zinc
9. Which of the following foods has been associated with an increased risk of skin cancer?
a. Citrus fruits
b. Alcohol
c. Green leafy vegetables
d. Caffeinated coffee
10. Antioxidants found in fruits and vegetables function by eliminating free radicals and reactive oxygen species.
a. True
b. False
References
1. Skin cancer facts. Skin Cancer Foundation website. http://www.skincancer.org/skin-cancer-information/skin-cancer-facts. Last updated June 4, 2014. Accessed January 3, 2014.
2. Actinic keratosis. Skin Cancer Foundation website. http://www.skincancer.org/skin-cancer-information/actinic-keratosis. Accessed January 26, 2014.
3. Siegel R, DeSantis C, Virgo K, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62(4):220-241.
4. Rogers HW, Coldiron BM. Analysis of skin cancer treatment and costs in the United States medicare population, 1996-2008. Dermatol Surg. 2013;39(1 Part 1):36-42.
5. Nichols JA, Katiyar SK. Skin photoprotection by natural polyphenols: anti-inflammatory, antioxidant and DNA repair mechanisms. Arch Dermatol Res. 2010;302(2):71-83.
6. Blanchard CM, Courneya KS, Stein K; American Cancer Society’s SCC-II. Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American Cancer Society’s SCS-II. J Clin Oncol. 2008; 26(13):2198-2204.
7. Kushi LH, Doyle C, McCullough M, et al. American Cancer Society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2012;62(1):30-67.
8. Ibiebele TI, van der Pols JC, Hughes MC, Marks GC, Williams GM, Green AC. Dietary pattern in association with squamous cell carcinoma of the skin: a prospective study. Am J Clin Nutr. 2007;85(5):1401-1408.
9. Millen AE, Tucker MA, Hartge P, et al. Diet and melanoma in a case-control study. Cancer Epidemiol Biomarkers Prev. 2004;13(6):1042-1051.
10. de Vries E, Trakatelli M, Kalabalikis D, et al. Known and potential new risk factors for skin cancer in European populations: a multicenter case-control study. Brit J Dermatol. 2012;167(Suppl 2):1-13.
11. McNaughton SA, Marks GC, Green AC. Role of dietary factors in the development of basal cell cancer and squamous cell cancer of the skin. Cancer Epidemiol Biomarkers Prev. 2005;14(7):1596-1607.
12. Stahl W, Heinrich U, Jungmann H, Sies H, Tronnier H. Carotenoids and carotenoids plus vitamin E protect against ultraviolet light-induced erythema in humans. Am J Clin Nutr. 2000;71(3):795-798.
13. Heinrich U, Gärtner C, Wiebusch M, et al. Supplementation with beta-carotene or a similar amount of mixed carotenoids protects humans from UV-induced erythema. J Nutr. 2003;133(1):98-101.
14. Wolf C, Steiner A, Hönigsmann H. Do oral carotenoids protect human skin against ultraviolet erythema, psoralen phototoxicity, and ultraviolet-induced DNA damage? J Invest Dermatol. 1988;90(1):55-57.
15. Garmyn M, Ribaya-Mercado JD, Russel RM, Bhawan J, Gilchrest BA. Effect of beta-carotene supplementation on the human sunburn reaction. Exp Dermatol. 1995;4(2):104-111.
16. Frieling UM, Schaumber SDA, Kupper TS, Muntwyler J, Hennekens CH. A randomized, 12-year primary-prevention trial of beta carotene supplementation for nonmelanoma skin cancer in the physician’s health study. Arch Dermatol. 2000;136(2):179-184.
17. Stahl W, Heinrich U, Wiseman S, Eichler O, Sies H, Tronnier H. Dietary tomato paste protects against ultraviolet light-induced erythema in humans. J Nutr. 2001;131(5):1449-1451.
18. Moon TE, Levine N, Cartmel B, et al. Effect of retinol in preventing squamous cell cancer in moderate-risk subjects: a randomized, double-blind, controlled trial. Southwest skin cancer prevention study group. Cancer Epidemiol Biomarkers Prev. 1997;6:949-956.
19. Asgari MM, Brasky TM, White E. Association of vitamin A and carotenoid intake with melanoma risk in a large prospective cohort. J Invest Derm. 2012;132(6):1573-1582.
20. Omenn GS, Goodman GE, Thornquist MD, et al. Risk factors for lung cancer and for intervention effects in CARET, the Beta-Carotene and Retinol Efficacy Trial. J Natl Cancer Inst. 1996;88(21):1550-1559.
21. Jung M, Bu SY, Tak K, Park J, Kim E. Anticarcinogenic effect of quercetin by inhibition of insulin-like growth factor (IGF)-1 signaling in mouse skin cancer. Nutr Res Pract. 2013;7(6):439-445.
22. Shukla S, Gupta S. Apigenin: a promising molecule for cancer prevention. Pharm Res. 2010;27(6):962-978.
23. Heinrich U, Neukam K, Tronnier H, Sies H, Stahl W. Long-term ingestion of high flavanol cocoa provides photoprotection against UV-induced erythema and improves skin condition in women. J Nutr. 2006;136(6):1565-1569.
24. Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr. 2010;92(5):1189-1196.
25. Fortes C, Mastroeni S, Melchi F, et al. A protective effect of the Mediterranean diet for cutaneous melanoma. Int J Epidemiol. 2008;37(5):1018-1029.
26. Hughes MC, van der Pols JC, Marks GC, Green AC. Food intake and risk of squamous cell carcinoma of the skin in a community: the Nambour skin cancer cohort study. Int J Cancer. 2006;119(8):1953-1960.
27. Hughes MCB, Williams GM, Fourtanier A, Green AC. Food intake, dietary patterns, and actinic keratoses of the skin: a longitudinal study. Am J Clin Nutr. 2009;89(4):1246-1255.
28. Gamba CS, Stefanick ML, Shikany JM, et al. Low-fat diet and skin cancer risk: the women’s health initiative randomized controlled dietary modification trial. Cancer Epidemiol Biomarkers Prev. 2013;22(9):1509-1519.
29. Jaax S, Scott LW, Wolf JE Jr, Thornby JI, Black HS. General guidelines for a low-fat diet effective in the management and prevention of nonmelanoma skin cancer. Nutr Cancer. 1997;27(2):150-156.
30. US Department of Agriculture, US Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th ed. Washington, DC: US Government Printing Office; 2010.
31. Noel SE, Stoneham AC, Olsen CM, Rhodes LE, Green AC. Consumption of omega-3 fatty acids and the risk of skin cancers: a systematic review and meta-analysis. Int J Cancer. 2014;135(1):148-156.
32. Hakim IA, Harris RB, Ritenbaugh C. Fat intake and risk of squamous cell carcinoma of the skin. Nutr Cancer. 2000;36(2):155-162.
33. Orengo IF, Black HS, Wolf JE Jr. Influence of fish oil supplementation on the minimal erythema dose in humans. Arch Dermatol Res. 1992;284(4):219-221.
34. Pilkington SM, Watson RE, Nicolaou A, Rhodes LE. Omega-3 polyunsaturated fatty acids: photoprotective macronutrients. Exp Dermatol. 2011;20(7):537-543.
35. Song F, Qureshi AA, Han J. Increased caffeine intake is associated with reduced risk of basal cell carcinoma of the skin. Cancer Res. 2012;72(13):3282-3289.
36. Veierod MB, Thelle DS, Laake P. Diet and risk of cutaneous malignant melanoma: a prospective study of 50,757 Norwegian men and women. Int J Cancer. 1997;71(4):600-604.
37. Abel EL, Hendrix SO, McNeeley SG, et al. Daily coffee consumption and prevalence of nonmelanoma skin cancer in Caucasian women. Eur J Cancer Prev. 2007;16(5):446-452.
38. Hakim IA, Harris RB, Weisgerber UM. Tea intake and squamous cell carcinoma of the skin: influence of type of tea beverages. Cancer Epidemiol Biomarkers Prev. 2000;9(7):727-731.
39. Conney AH, Zhou S, Lee MJ, et al. Stimulatory effect of oral administration of tea, coffee or caffeine on UVB-induced apoptosis in the epidermis of SKH-1 mice. Toxicol Appl Pharmacol. 2007;224(3):209-213.
40. Benedetti A, Parent ME, Siemiatycki J. Lifetime consumption of alcoholic beverages and rick of 13 types of cancer in men: results from a case-control study in Montreal. Cancer Detect Prev. 2009;32(5-6):352-362.
41. Jensen A, Birch-Johansen F, Olesen AB, Christensen J, Tjonneland A, Kjaer SK. Intake of alcohol may modify the risk for non-melanoma skin cancer: results of a large Danish prospective cohort study. J Invest Derm. 2012;132:2718-2726.


