Today’s Dietitian
Vol. 17 No. 9 P. 56
Because malnutrition screening remains unstandardized for hospital discharge, dietitians must recognize malnutrition diagnostic criteria and make appropriate recommendations to ensure proper nutrition following inpatient stays.
An 81-year-old Fayetteville, North Carolina, man who lives alone called 911 operators asking for food after being discharged home from the hospital and rehabilitation center for cancer treatment. Weighing only 115 lbs and unable to “get out of his chair,” he reported being hungry and had returned home to an empty refrigerator. He requested some food items to hold him over until his home care visits started.1 This story exemplifies the risk factors for malnutrition in older adults including the psychosocial, functional, and economic risk factors, as well as the traditional physiological risk factors related to acute and chronic diseases. More importantly, this real-life story underscores the importance of proper food and nutrition during care transitions.
The aging American population will continue to exert an impact on the US health care system. In 2010, 38.7% of hospital discharges and 44.8% of days of hospital care were attributed to older adults.2 As the number of older adults receiving acute care increases, so will their postdischarge needs. However, there are significant differences in posthospital health care utilization in the elderly. The oldest (aged 85 and older) are less likely to be discharged to home after a hospital stay and more likely to be discharged to long term care, compared with older adults in the 65 to 74 and 75 to 84 age groups.3 Older adults are at risk of malnutrition across the care continuum. What’s more problematic is that while nutrition screening often is performed on admission to an acute care hospital or long term care facility, an older adult’s nutrition status can worsen during an inpatient acute care or rehabilitation stay. Malnutrition screening isn’t performed routinely at discharge so it becomes critical for physicians to pay careful attention to nutrition status during follow-up office visits.
Prevalence Across Care Settings
Due to the lack of national prevalence rates for malnutrition across care settings, much of what’s known about the prevalence of malnutrition in older adults comes from research studies. Further, the wide range of malnutrition prevalence rates reported are due to different methodologies and measures used across studies. For example, a review of studies on malnutrition in hospitalized older adults reported a prevalence rate of 12% to 70%.4 In nursing homes, as in the hospitalized setting, the reported prevalence also varies widely, ranging from 1.5% to 67% or more of the population having some degree of malnutrition.5 Less is known about the rate of malnutrition in community-dwelling older adults in the United States. Using a probability sample of 3,209 community-dwelling older adults (aged 60 years and older) living in southeast Pennsylvania, researchers reported that 56.3% were at risk of malnutrition and 5.9% were malnourished.6
While The Joint Commission requires nutrition screening upon hospital admission, there’s no mandate for a standardized tool, and even if a patient has malnutrition, this may not be appropriately coded in the medical record. A recent study examined the diagnosis of malnutrition using ICD-9 codes and the associated demographic and clinical characteristics.7 This nationally representative sample of US hospital discharges from the 2010 Healthcare Cost and Utilization Project found that only 3.2% had a reported diagnosis of malnutrition. However, those with malnutrition were older, had longer lengths of stay, and higher costs of care.7
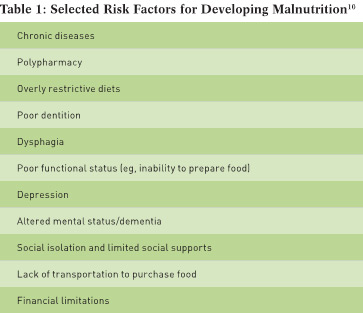
Risk Factors
With aging, there are a number of factors that contribute to the risk of malnutrition. Chronic disease can be a major contributor. Many diseases, such as cardiac disease, renal impairment, and malignancy contribute to inflammation that can lead to significant loss of muscle mass.8 In addition, many diseases may prompt the prescription of restrictive diets that may not always be necessary. Overly restrictive diets may be unpalatable or difficult to follow, leading to a decline in oral intake and, eventually, malnutrition.9 Functional status changes that limit ability to perform activities of daily living such as cooking and shopping can impact an older adult’s dietary intake. Significant psychosocial changes that also may occur with aging (eg, depression or simply eating alone), as with the loss of a spouse, can lead to a dramatic decrease in oral intake. Changes in finances also can impact the ability to purchase adequate food.10 Contributors to the development of malnutrition are summarized in Table 1.
Screening for Malnutrition
For physician practices certified by The Joint Commission, it’s recommended that, “Nutrition screening may be performed at the first visit for primary care, an ambulatory clinic, or office practice. Thereafter, the screens and assessment would be needed only as appropriate for the reason the patient is presenting for care or services.”11 However, this recommendation may not be sufficient for older adults. If an older adult has experienced an acute medical or surgical condition, a change in a chronic condition, or recent discharge from a hospital, rehabilitation, or long term care setting, it may be prudent to rescreen of nutritional problems. The diagnosis of malnutrition, risk for malnutrition, or the nutrition plan of care may not be included on the discharge summaries.
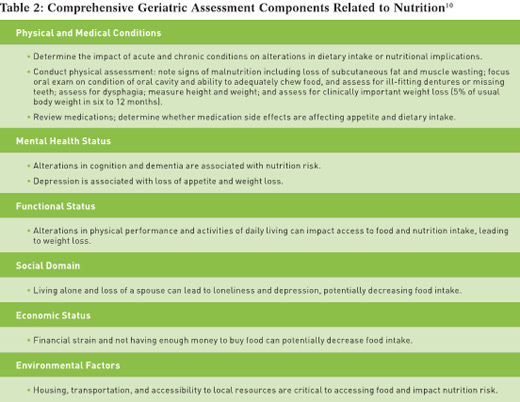
Furthermore, older adults may become more vulnerable to malnutrition during recovery, especially if they have a weakened state, are unable to perform the routine activities of daily living, and live alone. At the present time, nutrition screening is always conducted upon admission to the hospital but not standardized upon discharge. Therefore it’s prudent to implement nutrition screening as part of the routine geriatric assessment and to be on alert especially after an older patient has been discharged from the hospital or a skilled care or rehab facility. The best age-appropriate tool for nutrition screening in older adults is the Mini Nutritional Assessment (MNA) tool. It was developed specifically for the geriatric population and has two validated forms. The short form (MNA-SF) consists of only seven questions regarding changes in food intake, weight, mobility status, current disease or psychological stress, presence of neuropsychological problems, and BMI. The full MNA consists of a total of 18 questions, which include all of the questions in the MNA-SF as well as additional data collection including anthropometric measurements.12 Both the MNA-SF and full MNA have been used in many studies internationally, and the forms are available in 30 languages and are free to download (www.mna-elderly.com). Many of the components of a nutrition screen and/or nutrition assessment can be easily gathered from an in-depth comprehensive geriatric assessment as noted in Table 2.
New Diagnostic Criteria
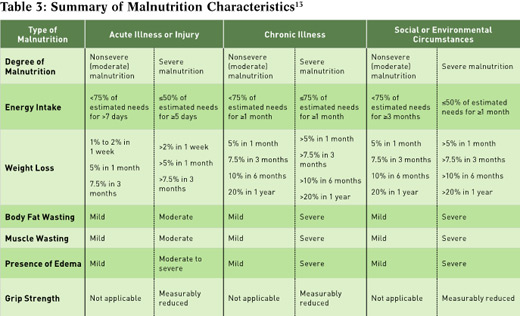
It’s difficult to consistently identify malnutrition in clinical research, as there hasn’t been a single unifying definition of malnutrition. Definitions of malnutrition range from simple, such as degree of unintentional weight loss, to complex calculations that include anthropometric measurements and biochemical measures (generally serum albumin). In 2012, the Academy of Nutrition and Dietetics and the American Society for Parenteral and Enteral Nutrition (ASPEN) collaborated to develop clear characteristics to define three broad categories of malnutrition.13 These characteristics include the etiology of malnutrition, recognizing the influence of illness and inflammation on nutritional status. Starvation-related malnutrition describes pure starvation or anorexia nervosa; this type of malnutrition is caused by energy deficit, without any underlying inflammation. Chronic disease-related malnutrition is characterized by mild to moderate inflammation in the setting of chronic disease (defined as a disease or condition lasting three months or more), such as end-stage renal disease or rheumatoid arthritis. Acute disease or injury-related malnutrition is characterized by severe inflammation in the setting of acute illness, such as severe sepsis or trauma. These types of malnutrition have subcategories of moderate (or nonsevere) or severe malnutrition, depending on specific parameters described in Table 3. It’s important to note that classifying a patient with a specific type of malnutrition requires only two criteria.
Biochemical indicators are no longer used to identify malnutrition. Albumin was a popular method of evaluating visceral protein status. However, albumin and prealbumin (another popular circulating protein used to evaluate nutritional status) are negative acute phase proteins. In the setting of inflammation, these proteins are depressed, and acute phase proteins such as C-reactive protein are produced. Thus, a low albumin or prealbumin actually may be indicators of illness and inflammation rather than measures of nutritional status.8,13
Nutrition Interventions
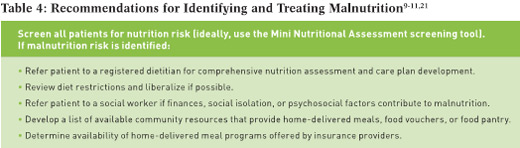
Once a patient is identified as being at nutrition risk or suffering from malnutrition, interventions should be implemented in a timely fashion. These include referrals to dietitians and social workers (see Table 4). Dietitians can suggest appropriate meal choices and interventions, and social workers can help facilitate referrals for home-delivered meal services, supplemental nutrition assistance programs such as SNAP or food stamps, and in-home support to assist with cooking and shopping. Nutrition interventions may include lifting diet restrictions, encouraging frequent nutrient-dense meals with adequate calories and proteins, and use of oral nutrition supplements to increase calories and protein. The advantages of supplements are that they are easy to use and readily available. However, the downside is that some older adults may not like the taste, and even more so, might lack adequate resources to pay for supplements. Alternative menu planning such as specialized recipes for homemade nutritional drinks may be more acceptable and cost-effective. Nutrition counseling also can include ways to increase nutrient density of meals and snacks in a palatable and cost-effective manner. Reimbursement for outpatient nutrition counseling will depend on the type of insurance. Medicare Part B will cover medical nutrition therapy for patients with diabetes or kidney disease, and for patients who have had a kidney transplant within the past 36 months.14 Other disease states may be covered if a patient has private insurance coverage in addition to Medicare.
Patients with swallowing disorders may benefit from enteral nutrition, and those with gastrointestinal failure may benefit from parenteral nutrition. Short-term nutrition support generally is initiated as a bridge to an oral diet. Examples of this type of situation include a patient who has dysphagia after a cerebrovascular accident and requires a short-term nasogastric tube until swallowing function improves, or a patient who has had gastrointestinal surgery that has been complicated by a prolonged ileus. Long-term enteral access should be considered carefully in patients with advanced dementia, as a number of studies suggest high mortality associated with feeding tube insertion.15-17 The International Clinical Ethics Section of ASPEN recently published a useful review with a decision-making algorithm to help in the decision-making process in this population.18
Need for Nutrition Transition Programs
In 2011, the Institute of Medicine convened a public workshop on Nutrition and Healthy Aging in the Community.19 Presenters highlighted issues related to community-based delivery of nutrition services for older adults and the need to identify and develop nutrition programs that promote successful transitions from acute, subacute, and chronic care to the home.19 Nutrition services often aren’t coordinated between the hospital and home, and there’s a need to ensure coordination of medical and social services for frail, vulnerable older adults, many of whom live alone and experience transient or permanent alterations in activities of daily living in the early postdischarge period.20 A study published in the October 2013 issue of Clinical Nutrition Insight calls for health care providers to be “well informed about nutrition resources available in the communities they serve and establish direct contact with these organizations.”21
Local branches of the Administration on Aging often list available programs for seniors in the communities they serve. Home-delivered meals (HDM) ensure older adults are receiving nourishing meals during the transition from hospital to home. HDM programs are funded either through the federal Title III C Older Americans Act Nutrition Program or through local community-based or faith-based organizations. Meal delivery varies according to agencies, with some agencies delivering one meal per day and others delivering a week’s worth of frozen meals. In addition to HDM programs, a variety of flexible meal services are available in local communities. For example, voucher programs provide participants the option of purchasing nutritious food at a grocery store, restaurant, or hospital cafeteria.19 Some health insurance plans now offer meal services. For example, Humana’s Well Dine program provides nutritional meals to eligible Medicare members recovering following an inpatient stay or after discharge from a skilled nursing facility, as well as those with a qualified chronic-condition special needs plan.22
Hospitals also are recognizing the need to provide continued nutrition services to at-risk older adults. As part of Boston Medical Center’s Elders Living at Home Program, the Healthy Eating for At Risk Older Adults program provides fresh nutritious foods free of charge, HDM to those with limited mobility, and nutrition education programs.23 The basic need for food during care transitions isn’t a problem limited to the United States. For example, in the United Kingdom, some hospitals are sending patients home with “food-to-go” bags, consisting of basic staples to help ease the transition when patients first return home from the hospital.24
Role of Health Care Providers
Nutrition plays a vital role for successful aging. While older adults are at risk of malnutrition due to physiological, psychosocial, and economic factors, transition from an inpatient stay to the home can intensify the risk. Geriatricians and primary care providers play an important role in the early recognition and treatment of nutrition disorders, including prescribing nutrition interventions and placing consults for dietitians and social workers to ensure older adults have access to nutritious food to enable recovery during care transitions.
— Kris M. Mogensen, MS, RD, LDN, CNSC, is a team leader dietitian at Brigham and Women’s Hospital and an instructor in nutrition at Boston University College of Health and Rehabilitation Sciences: Sargent College. Her clinical focus centers on enteral and parenteral nutrition and critical care while her research focuses on the impact of malnutrition on clinical outcomes.
— Rose Ann DiMaria-Ghalili, PhD, RN, CNSC, FASPEN, is an associate professor in the doctoral nursing department and holds a secondary appointment in the nutrition sciences department at Drexel University in Philadelphia. Her research focuses on the impact of nutrition on recovery and health outcomes in older adults across the care continuum.
References
1. ‘I can’t get out of my chair,’ elderly man with cancer calls 911 because he has no food. Fox 13 website. http://fox13now.com/2015/05/13/elderly-man-with-cancer-calls-911-because-he-has-no-food/. Updated May 14, 2015. Accessed June 3, 2015.
2. National hospital discharge survey. Centers for Disease Control and Prevention website. http://www.cdc.gov/nchs/nhds/nhds_tables.htm#number. Updated August 28, 2012. Accessed May 15, 2015.
3. Levant S, Chari K, DeFrances CJ. Hospitalizations for patients aged 85 and over in the United States, 2000-2010. Centers for Disease Control and Prevention website. http://www.cdc.gov/nchs/data/databriefs/db182.htm. Updated January 14, 2015.
4. Heersink JT, Brown CJ, DiMaria-Ghalili RA, Locher JL. Undernutrition in hospitalized older adults: patterns and correlates, outcomes, and opportunities for intervention with a focus on processes of care. J Nutr Elder. 2010;29(1):4-41.
5. Bell CL, Lee AS, Tamura BK. Malnutrition in the nursing home. Curr Opin Clin Nutr Metab Care. 2015;18(1):17-23.
6. DiMaria-Ghalili RA, Michael YL, Rosso AL. Malnutrition in a sample of community-dwelling older Pennsylvanians. J Aging Res Clin Pract. 2013;2(1):39-45.
7. Corkins MR, Guenter P, DiMaria-Ghalili RA, et al. Malnutrition diagnoses in hospitalized patients: United States, 2010. JPEN J Parenter Enteral Nutr. 2014;38(2):186-195.
8. Jensen GL. Inflammation as the key interface of the medical and nutrition universes: a provocative examination of the future of clinical nutrition and medicine. JPEN J Parenter Enteral Nutr. 2006;30(5):453-463.
9. Zeanandin G, Molato O, Le Duff F, Guérin O, Hébuterne X, Schneider SM. Impact of restrictive diets on the risk of undernutrition in a free-living elderly population. Clin Nutr. 2012;31(1):69-73.
10. DiMaria-Ghalili RA. Integrating nutrition in the Comprehensive Geriatric Assessment. Nutr Clin Pract. 2014;29(4):420-427.
11. Nutritional, functional, and pain assessments and screens. The Joint Commission website. http://www.jointcommission.org/mobile/standards_information/jcfaqdetails.aspx
?StandardsFAQId=471&StandardsFAQChapterId=1. Updated November 24, 2008. Accessed June 4, 2015.
12. Anthony PS. Nutrition screening tools for hospitalized patients. Nutr Clin Pract. 2008;23(4):373-382.
13. White JV, Guenter P, Jensen G, et al. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN J Parenter Enteral Nutr. 2012;36(3):275-283.
14. Nutrition therapy services (medical). Medicare website. http://www.medicare.gov/coverage/nutrition-therapy-services.html. Accessed May 31, 2015.
15. Sampson EL, Candy B, Jones L. Enteral tube feeding for older people with advanced dementia. Cochrane Database Syst Rev. 2009;(2):CD007209.
16. Hanson LC. Tube feeding versus assisted oral feeding for persons with dementia: using evidence to support decision-making. Ann Longterm Care. 2013;21(1):36-39.
17. Givens JL, Selby K, Goldfield KS, Mitchell SL. Hospital transfers of nursing home residents with advanced dementia. J Am Geriatr Soc. 2012;60(5):905-909.
18. Schwartz DB, Barrocas A, Wesley JR, et al. Gastrostomy tube placement in patients with advanced dementia or near end of life. Nutr Clin Pract. 2014;29(6):829-840.
19. Institute of Medicine. Nutrition and healthy aging in the community — workshop summary. http://www.iom.edu/reports/2012/nutrition-and-healthy-aging-in-the-community.aspx. Published March 20, 2012.
20. Sahyoun NR, Vaudin A. Home-delivered meals and nutrition status among older adults. Nutr Clin Pract. 2014;29(4):459-465.
21. Sahyoun NR, Vaudin A. Nutrition in the transition of care from hospital to home. Clin Nutr Insight. 2013;39(10):1-4.
22. Humana Well Dine. Humana website. https://www.humana.com/provider/support/clinical/health/meals. Accessed June 3, 2015.
23. Elders Living at Home Program. Boston Medical Center website. http://bmc.org/eldersathome/nutrition.htm. Accessed June 4, 2015.
24. Local hospitals offer patients ‘Food-to-Go” bags when they are discharged. Fresh Start website. http://freshstart.uhmb.nhs.uk/consultants-blog/local-hospitals-offer-patients-food-go-bags-when-they-are-discharged. Updated April 2, 2015. Accessed June 3, 2015.


