Today’s Dietitian
Vol. 25 No. 9 P. 24
Patient Care and Counseling Guidance for RDs
Obesity management is at an inflection point and entering a new era with new pharmacologic interventions. These include mono agonists, glucagonlike peptide-1 receptor agonists (GLP-1 agonists), and dual agonists that combine a glucose-dependent insulinotropic polypeptide (GIP) with a GLP-1 agonist (GIP/GLP-1), which have demonstrated a 15% and greater weight loss in people with obesity and/or type 2 diabetes, says Richard E. Pratley, MD, medical director of Advent Translational Research Institute and AdventHealth Diabetes Institute in Orlando, Florida.
Over the last couple of decades, Pratley says, the scientific research community has learned that incretin hormones, including GLP-1, GIP, and others, are important regulators of metabolism with impacts on glycemia, lipids, and body weight.
Due to the dramatic benefits observed with these medications, barely a day goes by without health care providers and consumer-aimed headlines either raving or raising concerns about them. RDs find themselves counseling patients who are curious or take these medications and often are peppered with questions about their actions, side effects, and implications for short- and long-term use.
After providing some background about these drugs, including a brief explanation of how they work, this article will focus on patient care and counseling guidance for RDs. To delve deeper into various other aspects of these medications, see the sidebar “Resources” below.
Bit of Background
These new classes of antiobesity medications (ie, the GLP-1 agonists and dual agonists), referred to in this article as weight management medications, aren’t really new.1-4 The basic science and pharmaceutical research and development to bring these to market began more than two decades ago when two scientists, Matthias Tschop, MD, and Richard DiMarchi, PhD, hypothesized that the actions of various gut hormones may offer safe and unprecedented weight loss. Tschop recounted his research with DiMarchi and that of others while he accepted the 2023 Banting Medal for Scientific Achievement at the 2023 American Diabetes Association Scientific Sessions.5
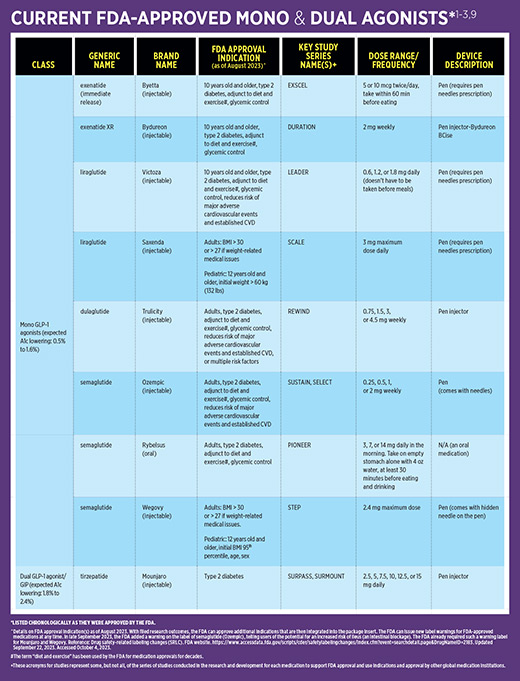
The FDA approved the first GLP-1 agonist, twice-a-day Byetta (exenatide), in 2005.1 Since then, several newer and more powerful medications in the GLP-1 agonist class, such as liraglutide and semaglutide, have received FDA approval for type 2 diabetes, with a higher dose of semaglutide FDA approved for weight loss.2 In mid-2022, the first dual agonist, tirzepetide (a combination of a GLP-1 agonist and a GIP), was FDA approved for type 2 diabetes. Later in 2022, the FDA granted tirzepetide fast track designation for overweight and obesity in adults.6 To date, tirzepetide hasn’t been FDA approved for weight loss (see table “Current FDA-Approved Mono and Dual Agonists” for details about weight management medications).
While there are other weight management medications to prescribe, these drug classes have demonstrated dramatic weight loss, improved glycemia, and potential benefits for cardiovascular health. As a result, they’ve shifted the weight management paradigm and rapidly have been integrated into clinical algorithms and recommendations.7-11
How and Why They Work
GLP-1 has several actions, whether secreted endogenously from the intestine or used as a medication. GLP-1 agonists within the gut assist with weight loss by decreasing appetite and promoting satiety.3 They slow gastric emptying, promote satiety, and decrease postprandial glucose levels. GLP-1 agonists also stimulate pancreatic beta cells to secrete insulin and tamp down glucagon secretion from the pancreatic alpha cells. The second incretin, GIP, whose receptors reside in adipose tissue, increases insulin secretion and suppresses glucagon release. GIP also decreases postprandial glycemia and improves insulin sensitivity.
“In people with normoglycemia and without excess adiposity, the incretin hormones GLP-1 and GIP work in concert to manage postprandial insulin levels,” says Colleen Dawkins, FNP-C, RDN, CSOWM, a family nurse practitioner at Big Sky Medical Wellness, in Lakeside, Montana. However, in the presence of excess adipose tissue, GLP-1, GIP, glucagon, and insulin are altered, Dawkins says. With insulin resistance, common in people with excess adiposity, prediabetes, and type 2 diabetes, glucagon and insulin levels may be elevated. Even if GLP-1 and GIP secretion are present in these scenarios, both hormones usually have decreased effectiveness. Dawkins and Pratley note that while studies show people with obesity and type 2 diabetes experience significant weight loss on a GLP-1 agonist or dual agonist, people with type 2 diabetes experience slightly less weight loss compared with those with overweight and obesity without type 2 diabetes.1-3
Counseling Tips for RDs
Despite the success of these classes of weight management medications, patients can receive anywhere from a little to a lot of information on how to optimize their use since a wide variety of clinicians, from primary care providers to obesity medicine experts, prescribe them. Patients may or may not obtain follow-up and/or referrals to RDs. The following counseling tips can help dietitians, and all clinicians, improve short- and long-term use of these weight management medications.
• Explain the basics of how the medications work. Discuss the fact that the medication contains hormones naturally made by the body but are deficient in people with excess weight and/or who have type 2 diabetes. Helping patients understand the actions of these medications can alert them to the potential gastrointestinal (GI) side effects (see sidebar “Tips to Minimize GI Side Effects” below).
• Show patients how to use the injectables. Ask whether they’ve previously used an injectable and how they feel about self-injecting. Teach the proper technique, and check their technique at follow-up visits. RDs can practice with a demo injector, if available.
• Discuss the importance of taking medication timely. “It’s important to take the injectable medication the same day and same time each week,” Dawkins says. Encourage patients to choose a time and day of the week that will work, and encourage them to set a calendar reminder alert.
• Be aware of key contraindications. Review the package insert for each medication.
• Encourage patients to avoid nonprescription forms of these weight management medications. This includes compounded forms. “There’s concern about the safety of different salt formulations,” says Diana Isaacs, PharmD, BCADM, CDCES, an endocrinology clinical pharmacy specialist at the Cleveland Clinic Endocrinology and Metabolism Institute in Cleveland. Doses can’t be guaranteed, and they may be mixed with other ingredients that may lead to adverse effects, Isaacs says. The FDA issued a warning about these formulations.12 Isaacs also raises safety concerns about obtaining these medications online and from other countries.
• Warn patients about the potential for hypoglycemia. Low blood sugar may occur if these weight management medications are taken in addition to glucose-lowering drugs that can cause hypoglycemia (eg, insulin or a sulfonylurea). Prescribers should be notified if clients experience hypoglycemia so they can lower the dose of the medication that’s likely contributing most to hypoglycemia (insulin or sulfonylurea) or omit it altogether.
• Tell patients they may need to stop taking medication before surgery or diagnostic GI procedures due to possible risks caused by delayed gastric emptying.13,14 Recommend patients speak with their prescribers and/or physicians doing the procedure.
• Inform clients that the maximum dose may not be necessary. Suggest clients take one dose increase at a time, monitor GI disturbances and other side effects, and keep tabs on the rate of weight loss (see “Case Study Meet P.B.”).
• Discuss the possibility of losing facial fat. Patients may talk about “Ozempic face,” characterized by the loss of facial fat. This makes the face look hollowed out or gaunt, although it isn’t specific to Ozempic and generally can occur with any rapid weight loss.
• Provide individualized care and monitor patients. “A person with a BMI of 28 and a history of gestational diabetes may benefit from one of these medications to lose weight while concomitantly mastering lifestyle behaviors, and then transition off the weight management medications to lifestyle alone,” says Linda Gigliotti, MS, RDN, CDCES, CSOWM, an obesity and weight management specialist based in Irvine, California. Gigliotti contrasts such a patient with a person who has a BMI of 40 and diagnoses of hypertension, type 2 diabetes, CVD, and musculoskeletal issues, who may benefit from lifelong use of weight management medications.
• Monitor patients to minimize loss of lean body mass. “Make sure people get sufficient nutrition and are not losing too much muscle mass,” Isaacs says. And make sure GI side effects aren’t preventing them from getting the nutrition they need. Gigliotti recommends dietitians encourage clients to eat sufficient amounts of protein by including it at each meal and snack and eating it first to ensure it’s consumed. And they should engage in regular physical activity, including strength training to help retain lean body mass.
“It’s important to recognize that the loss of lean body mass is seen with virtually all methods to achieving significant weight loss. It reflects normal physiological adaptation,” Pratley says. It doesn’t impair function. In fact, most studies suggest that function improves with significant weight loss.
• Explain that healthful lifestyle changes must be made in concert with weight management medications. “Treating obesity requires a comprehensive and multifaceted approach that acknowledges the biological, psychological, social, and environmental factors that drive obesity, many of which are outside an individual’s control,” says Lisa Neff, MD, MS, a board-certified obesity medicine physician and endocrinologist with training in clinical nutrition, and executive director of global medical affairs at Eli Lilly and Company in Indianapolis. “By recognizing that obesity is a complex, chronic disease and not a lifestyle choice or a matter of willpower, we can help people find an integrated and personalized treatment approach that promotes long-term health and well-being,” Neff adds.
According to Gigliotti, “[Weight management medications] can make eating healthier easier because people may experience fewer cravings and less temptation to overeat.”
• Share that stopping weight management drugs can result in weight regain. “As weight is lost, the body adapts (metabolically) and requires fewer calories to support a lower weight,” Dawkins says. This is referred to as metabolic adaptation, which reduces GLP-1 and GIP levels and increases the orexigenic hormone ghrelin. These adaptive changes increase the likelihood of weight regain. Ongoing use of weight management medications supports normalization of these hormones and aids long-term weight maintenance, Dawkins adds.
• Discuss the need for long-term medication use. Explain to clients that weight management medications aren’t a magic bullet or short-term weight loss fix. “People need to know from the start that these are prescribed as long-term medications for their effect on body weight, glucose levels, and potentially cardiovascular protection,” Pratley says, adding that people don’t stop antihypertensives or statins because they achieve or reach normal blood pressure or LDL cholesterol levels, respectively.
• Integrate ongoing conversations about obesity as a chronic disease. Inform patients that management requires implementing a long-term plan, setting realistic weight goals, and overcoming ongoing challenges of weight maintenance. “Weight reduction triggers adaptive changes in hunger and satiety hormones and energy expenditure, which favor weight regain,” Neff says. “As a result, maintaining weight loss with lifestyle modification alone can be challenging,” due, in part, to metabolic adaptation as explained.
The Future
The future is bright for GLP-1 agonists and their close relatives. Far along in research and development is Eli Lilly’s retatrutide, a triple agonist that adds glucagon to GLP-1 and GIP, and the requisite studies are underway.1,14 In addition, there’s cagrisema from NovoNordisk, a blend of semaglutide (GLP-1 agonist) and a long-acting amylin (another pancreatic hormone) analog cargrilintide.
A medication being codeveloped by Boehringer Ingelheim and Zealand Pharma is survodutide, which combines a GLP-1 agonist and glucagon. Another medication in the works is dapiglutide, a blend of GLP-1 and GLP-2 agonists, and there are more therapies coming down the pike. Currently in research and development are several small molecule nonpeptide oral GLP-1 agonists that have positive human research results. And there are what’s called the -gliprons, such as danuglipron and oroforglipron, that researchers are studying.1,15
As more people choose to take these weight management medications, RDs must educate themselves about them. Dietitians can embrace weight management medications as a helpful element of successful short- and long-term management of type 2 diabetes, excess weight, CVD, and potentially other comorbidities. RDs also can advocate for the safe and proper use of weight management medications in tandem with promoting the critical roles of healthful eating, lifestyle modifications, and medication adherence.
— Hope Warshaw, MMSc, RD, CDCES, BC-ADM, FADCES, is owner of Hope Warshaw Associates, LLC, a diabetes- and nutrition-focused consultancy based in Asheville, North Carolina. She’s a book author and freelance writer specializing in diabetes care and education. Warshaw served as the 2016 president of ADCES and is chair of the Academy of Nutrition and Dietetics, 2022–2023.
References
1. Sheahan KH, Wahlberg EA, Gilbert MP. An overview of GLP-1 agonists and recent cardiovascular outcomes trials. Postgrad Med J. 2020;96:156-161.
2. Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus. UpToDate website. https://www.uptodate.com/contents/glucagon-like-peptide-1-based-therapies-for-the-treatment-of-type-2-diabetes-mellitus. Accessed August 17, 2023.
3. Isaacs, D, Bellini N, Stahl-Salzman R. A deep dive into GLP1 agonists. Lifescan Diabetes Institute website. https://www.lifescandiabetesinstitute.com/glucose-management/deep-dive-glp1-agonists. Accessed August 24, 2023.
4. Prillaman M. Four key questions on the new wave of anti-obesity drugs. Nature website. https://www.nature.com/articles/d41586-023-02445-4. Published August 2, 2023. Accessed August 24,2023.
5. Tschop M, Noguieras R, Ahren B. Gut hormones-based pharmacology: novel formulations and future possibilities for metabolic disease therapy. Diabetologia. 2023;66:1796-1808.
6. Lilly receives U.S. FDA Fast Track designation for tirzepatide for the treatment of adults with obesity, or overweight with weight-related comorbidities. Eli Lilly and Company website. https://investor.lilly.com/news-releases/news-release-details/lilly-receives-us-fda-fast-track-designation-tirzepatide. Published October 6, 2022.Accessed August 24,2023.
7. ElSayed NA, Aleppo G, Aroda VR, et al. 8. Obesity and weight management for the prevention and treatment of type 2 diabetes: standards of care in diabetes – 2023. Diabetes Care. 2023;46(Supp 1):S128-S139.
8. ElSayed NA, Aleppo G, Aroda VR, et al. 9. Pharmacological approaches to glycemic treatments: standards of care in diabetes – 2023. Diabetes Care. 2023;46(Supp 1):S140-S157.
9. ElSayed NA, Aleppo G, Aroda VR, et al. 10. Cardiovascular disease and risk management: standards of care in diabetes – 2023. Diabetes Care. 2023;46(Supp 1):S158-S190.
10. Samson SL, Vellanki P, Blonde L, et al. American Association of Clinical Endocrinology consensus statement: comprehensive type 2 diabetes management algorithm – 2023 update. Endocr Pract. 2023;29(5):305-340.
11. Bays H, Fitch A, Christensen S, et al. Anti-obesity medications and investigational agents: an Obesity Medicine Association (OMA) clinical practice statement (CPS) 2022. Obesity Pillars. 2022;2:100018.
12. Medications containing semaglutide marketed for type 2 diabetes or weight loss. FDA website. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/medications-containing-semaglutide-marketed-type-2-diabetes-or-weight-loss. Published May 31, 2023. Accessed August 24,2023.
13. American Society of Anesthesiologists consensus-based guidance on preoperative management of patients (adults and children) on GLP-1 receptor agonists. American Society of Anesthesiologists website. https://www.asahq.org/about-asa/newsroom/news-releases/2023/06/american-society-of-anesthesiologists-consensus-based-guidance-on-preoperative. Published June 29, 2023. Accessed August 24,2023.
14. Johnson DA. GI side effects, anesthesia risk with GLP-1 agonists: what to know. Medscape website. https://www.medscape.com/viewarticle/994762#vp_1. Published August 4, 2023. Accessed August 29, 2023.
15. ADA2023 in San Diego: watching the tides roll in. ConscienHealth website. https://conscienhealth.org/2023/06/ada2023-in-san-diego-watching-tides-roll-in/. Published June 24, 2023. Accessed August 17, 2023.
16. Choi J. Inside the push to get weight loss treatment covered by Medicare. The Hill. August 11, 2023. https://thehill-com.cdn.ampproject.org/c/s/thehill.com/policy/healthcare/4148133-inside-the-push-to-get-weight-loss-treatment-covered-by-medicare/amp/. Accessed August 17, 2023.
RESOURCES
• View LifeScan Diabetes Institute’s webinar, “A Deep Dive Into GLP1 Agonists,” and earn 1 CPEU through the Commission on Dietetic Registration. Membership is free at www.lifescandiabetesinstitute.com.
• Join the Diabetes Dietetic Practice Group (www.diabetesdpg.org) and Weight Management Dietetic Practice Group (www.wmdpg.org) of the Academy of Nutrition and Dietetics (the Academy). RDs can access webinars and print resources.
• Visit manufacturers’ websites and develop a relationship with their medical science liaisons, who fulfill specific roles in diabetes care and education.
• Subscribe to the daily blog at ConscienHealth (https://conscienhealth.org), an organization that works with experts and other groups to promote evidence-based approaches to health and obesity and serve as a voice for individuals affected by obesity.
• Earn CDR’s Certificate of Training in Obesity for Pediatrics and Adults. The training focuses on foundational concepts in weight management science and evidence-based practice to build knowledge, skills, and competence in pediatric and adult populations. Visit https://www.cdrnet.org/obesity-pediatrics-adults?preview=true.
• Use the Academy’s Evidence Analysis Library and read the Journal of The Academy of Nutrition and Dietetics to access recently published evidence-based practice guidelines and various types of literature reviews on overweight and obesity.
• Read the upcoming book Health Professional’s Guide to Treatment of Overweight and Obesity, edited by Hollie A. Raynor, PhD, RD, and Linda M. Gigliotti, MS, RDN, CDCES, CSOWM. With contributions from weight management experts, this book provides an in-depth exploration of adult weight management. It’s published by the Academy and will be released early 2024 and available at www.eatrightstore.org.
• Access “Lifestyle Approaches for Managing Type 2 Diabetes — Which Option Should I Choose?” This new toolkit is available on the Weight Management Dietetic Practice Group website and aims to assist RDs who counsel adults with type 2 diabetes to integrate shared decision making with counseling.
• Support and advocate for the federal legislation The Treat and Reduce Obesity Act. For more information, visit https://www.eatrightpro.org/advocacy/public-policy-priorities/all-legislation/treat-and-reduce-obesity-act.
• Explore the efforts of the Obesity Care Advocacy Network (https://obesitycareadvocacynetwork.com), a group of national organizations and corporations that advocate for improved Medicare coverage for obesity services.
— HW
TIPS TO MINIMIZE GI SIDE EFFECTS
One or more gastrointestinal (GI) side effects are observed in roughly 10% to 50% of people who take one of these weight management medications.1,2 From nausea and vomiting to acid reflux, bloating, stomach cramps, diarrhea, and/or constipation, patients can minimize GI side effects with a “start low, go slow” approach, starting with the lowest dose and titrating as recommended (see table “Currently FDA-Approved Mono and Dual Agonists”).
Symptoms frequently decrease over time as the body adapts and individuals change their eating habits and food choices. Here are some strategies dietitians can put into practice when counseling patients.
• Recommend some remedies for clients who are having GI side effects, but let them know that the side effects vary and likely will be transient. “These side effects may recur when the person titrates the dose,” Dawkins says. So, taking lower doses or titrating more slowly can help.
• Encourage patients to report side effects early so you can provide recommendations to alleviate symptoms or refer them to their prescribing physician, who can determine whether a medication intolerance exists before symptoms worsen. Some recommendations may include the following:
> Eat smaller portions of food than usual.
> At home, eat on smaller plates.
> In restaurants, ask for an empty container when ordering food. Put a portion of the food in the container to take home when the meal arrives, or order from the appetizers and/or sides on the menu.
> Eat slowly.
> Stop eating at the first sign fullness.
> Don’t forget to eat, eat regularly, and don’t let many hours pass by without eating. Remind clients to not rely on hunger to eat, as they may not get hungry.
> Limit high fat and greasy foods. These can take longer to digest.
> Limit spicy foods and choose bland foods that are easily tolerated.
> Stay hydrated.
> If constipation is a problem, encourage clients to consume high fiber foods such as fruits, vegetables, and whole grains. They also can eat dried fruit, which has a laxative property.
> To manage nausea, Dawkins suggests that patients drink ginger tea or take an antiemetic medication. Others suggest ginger or peppermint tea. Dawkins says, “Since the GIP [glucose-dependent insulinotropic polypeptide] hormone acts as an antiemetic, the dual agonist tirzepitide is associated with fewer adverse side effects and better tolerance.”
References
1. Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus. UpToDate website. https://www.uptodate.com/contents/glucagon-like-peptide-1-based-therapies-for-the-treatment-of-type-2-diabetes-mellitus. Updated September 8, 2023. Accessed August 17, 2023.
2. Isaacs, D, Bellini N, Stahl-Salzman R. A deep dive into GLP1 agonists. Lifescan Diabetes Institute website. https://www.lifescandiabetesinstitute.com/glucose-management/deep-dive-glp1-agonists. Accessed August 24, 2023.
CASE STUDY: Meet P.B.
P.B., a 5’ 7” male, aged 65, has struggled with his weight since middle school. He remembers attending WW (formerly Weight Watchers) with his mother. He lost weight in high school when enrolled in an ROTC program. He kept the weight off through college and during the early years of marriage. “After our second of four children, I began to pack the pounds back on,” P.B. says. He tried WW again, various eating plans, and the YMCA’s year-long Diabetes Prevention Program. He lost 10 lbs, then gained 20. P.B. has hypertension that’s managed on amlodipine. He’s also had a history of chronic lower gastrointestinal (GI) tract issues.
When P.B.’s A1c rose to 6.3%, (prediabetes range) in November 2022 and he weighed in at 240 lbs, his primary care provider suggested he take the medication Mounjaro at the starting 2.5 mg dose for four weeks. His primary care provider said P.B. may have some nausea the first week, but provided minimal guidance on managing the GI side effects. An incentive P.B. now had for weight loss turned into an episode of vertigo accompanied by cardiac symptoms and a hospitalization for evaluation.
P.B. defines the first week of taking Mounjaro as “hell,” as there was much nausea and vomiting. However, he says, “These symptoms could have come from a GI bug going around.” But P.B. stuck it out. Within two weeks, he started to feel full after eating small-to-medium portions of food. He says, “It’s the first time in decades that I’ve felt full.” P.B. stayed on the prescribed starting dose for four weeks. At his primary care provider’s direction, he then increased to 5 mg weekly for 12 weeks. He felt bloated for a couple of days but no nausea. “The portions of food I’m eating are now smaller than my wife’s. She’s still hungry while my eating is slowing down or stopping,” P.B. says.
P.B. has experienced, “massive benefits” to his gut health. “My gut is working normally for the first time in a decade.” P.B. also notes that his craving for sweets is essentially gone. He has less knee pain, and he’s walking more easily. He now walks 10,000 to 15,000 steps per day.
At a visit with his primary care provider in May 2023, he agreed to maintain the 5 mg per week dose due to his sufficient and steady weight loss.
As of late August 2023, P.B. weighed 198 lbs, a 40-lb weight loss with four inches off his waistline. His A1c has decreased to 5.6%. He’d like to reach 170 to 180 lbs and maintain it.
Regarding the cost of Mounjaro, “It’s been a roller coaster ride,” P.B. says. His employer-based health plan wouldn’t cover it. At his pharmacy, P.B. was told the starting one-month supply would cost $1,500. That was a no-go for P.B. However, he got a manufacturer’s discount that lowered the cost to $500. Still expensive, but P.B. took a leap of faith and paid for it. When P.B. filled his prescription for a three-month supply of the 5 mg dose, the price was $25 total. “A nice surprise,” P.B. says. However, before starting Medicare with a Part D policy (P.B. just turned 65), he got another three-month supply for $150.* P.B. recommends that people ask questions, take advantage of manufacturer discount coupons and assistance programs, and advocate for themselves.
*P.B.’s Medicare Part D plan for medications won’t cover Mounjaro due to a federal law passed in 2003 that prohibited Medicare from covering weight management medications because of supposed dangerous side effects. This prohibition remains in effect. However, an effort to change this and allow Medicare to cover obesity medications is within the Federal Treat and Reduce Obesity Act legislation (see sidebar “Resources”).1
Reference
1. Choi J. Inside the push to get weight loss treatment covered by Medicare. The Hill. August 11, 2023. https://thehill-com.cdn.ampproject.org/c/s/thehill.com/policy/healthcare/4148133-inside-the-push-to-get-weight-loss-treatment-covered-by-medicare/amp/. Accessed August 17, 2023.



