Suggested CDR Performance Indicators 1.7.2, 1.7.4, 2.1.1, 12.1.1
CPE Level 2
Take this course and earn 2 CEUs on our Continuing Education Learning Library
Increased research into the effects of social determinants of health (SDoH)—the circumstances and environment in which people live and the resources they have access to—in addition to greater awareness of the impact of systemic inequality, has resulted in individuals, organizations, and institutions in the United States examining how they may improve outcomes and reduce inequity for all groups. The health care field, including dietetics, is no exception. It’s become clear that good health and adequate health care aren’t equally accessible to all.1
A key to understanding inequity is recognizing that, throughout American history, power and resources traditionally have been concentrated among a few privileged groups, to the detriment of, most notably, people with low socioeconomic status; those with disabilities; women; Black, Indigenous, and people of color (BIPOC); and LGBTQ+ individuals, including people with lesbian, gay, bisexual, transgender, queer, asexual, and intersex identities. Both historically and in the present, members of these populations typically experience poorer health outcomes.1
Discriminatory actions toward historically marginalized and oppressed populations are built on long-standing structural and systemic inequities, including those in health care systems. Additionally, the chronic stress perpetuated by inequitable structures, environments, and distribution of resources, as well as everyday discriminatory encounters, has been identified as a key contributor to poorer health outcomes and, thus, health disparities among traditionally oppressed groups.1
Although the terms health disparity and health inequity are used interchangeably to represent a discrepancy between groups, they’re different. Health disparity simply implies there’s a difference in health-related risks and outcomes between people groups. Health inequities articulate that the inequality is unfair and due to injustices in a system.1
This continuing education course explores the roots of health inequities and disparities in the United States. It offers suggestions on how dietitians and other health care providers can engage in interpersonal work to reduce bias and advocate on behalf of their patients.
Historical Perspective
Racial inequities in the United States today can be traced back to the country’s founding, which is inextricable from the forcible removal of Indigenous Americans as settler-colonizers from Europe landed on the continent in 1492 and expanded westward. These Europeans brought diseases such as smallpox, which alone killed an estimated 90% of the Indigenous population by the early 1600s, and thousands more Native Americans died in violent attacks meant to drive them from their homes.2 The US government typically broke treaties promising land or resources to Indigenous Americans, with the government providing nothing and responding to Native resistance with military force. Then, from 1860 to 1978, the US government forced Indigenous children into boarding schools to eradicate the traditions, languages, and cultures of Indigenous peoples.3
Similarly, the institution of slavery set the stage for centuries of violence against Black Americans. As much as abolition of slavery was an enormous achievement, it was followed by decades of race-related violence (eg, individual physical and sexual violence against Black Americans; bombings and arsons of Black churches, community organizations, businesses, and homes; and everyday harassment and intimidation of Black Americans in public spaces) that went unprosecuted, as well as institutional, industrial, and government policies that crystalized discriminatory practices.
One such practice, redlining, affected (and still affects) many Black Americans’ ability to find safe and affordable housing. Redlining refers to the color-coded maps developed and used by the federal government in the 1930s and later adopted by the VA to designate locales for “safe” mortgage lending. Those areas with predominantly BIPOC populations were colored red to indicate “risky” lending, denying BIPOC individuals’ access to new suburban communities and prioritizing housing for the white middle class. The Federal Housing Administration went so far as to subsidize only builders who refused to sell the houses they built to Black Americans.4
Such segregation continues today in policies such as those that seek to prevent higher-density affordable housing from being constructed in certain neighborhoods. Inequities in BIPOC neighborhoods, including limited access to affordable and healthful food, few resources available to public schools, and poor public and residential infrastructure are just a few of the modern scars left by redlining.4
While the displacement of Indigenous peoples and slavery were key events in the physical and economic expansion of the United States, many other groups and populations have faced and continue to face other forms of discrimination and systemic oppression. Women, people with disabilities, LGBTQ+ individuals, and nonwhite people other than Black and Indigenous Americans all have been excluded from aspects of American culture and life, including certain jobs and professions and aspects of family life (eg, marriage, romantic and sexual relationships, parenthood). Such discrimination has resulted in violence, financial vulnerabilities, limited opportunities, social isolation, and health inequities.
Discrimination Amid Progress
Undoubtedly, historically oppressed groups have made leaps and bounds throughout the 20th century and so far in the 21st, from the civil rights movement of the 1950s and ’60s to the 2015 legalization of same-sex marriage, and beyond. Still, policies and norms within systems continue to impact social, professional, and health-related opportunities, taking a severe toll on the mental and physical well-being of these groups.1 Even as policies change for the better, interpersonal interactions can be just as harmful; chronic exposure to microaggressions (ie, indirect, subtle, and/or unintentional discriminatory actions against members of marginalized groups in their everyday lives) appears to exert a greater effect on well-being than a single traumatic event as allostatic load and the expression of genes (epigenetic changes).5,6
SDoH
SDoH have a significant downstream impact on a person’s health-related risk, quality of life, and health care outcomes. Healthy People 2030, a public health project of the US Department of Health and Human Services, categorizes SDoH into five major domains: 1) education, 2) economic stability, 3) social and community context, 4) the built environment, and 5) health and health care.7 They may appear to be related to individual behavior, but all have roots in systemic inequities resulting in the observed disparities.
Education and Economic Stability
Historically, higher education was an opportunity reserved for the elite majority in the United States. As a result, this privilege was often denied based on gender, LGBTQ+ identity, religion, race/ethnicity, ability, and social class. The 20th century brought about monumental changes that opened the door to education for people in marginalized groups.8 Despite greater access, disparities remain large in the education system.
A higher education level is correlated with better health and greater longevity, an association attributed to how education increases general and specific skillsets, improves critical thinking and problem solving, and diversifies and enhances employment opportunities, resulting in greater income.8 There are significant differences in lifetime earnings or the accrued income from the age of 20 to 69 based on an individual’s educational attainment. Those who have a bachelor’s degree earn $630,000 to $900,000 (women and men, respectively) more over a lifetime than those with a high school diploma.9 However, it doesn’t appear that being in a historically marginalized group but having greater privilege in other areas—for example, a higher socioeconomic status or greater wealth—is protective from the harm caused by discrimination.1 Inequities in education that perpetuate health disparities are associated with the systemic differences in school resource distribution—which often is based on locale—quality of instruction, student demographics, and development and support of instructional staff. Parents’ or caregivers’ socioeconomic status and education level also strongly influence students’ educational experiences.8
Education level also is strongly correlated with health literacy, or the process of obtaining, processing, and understanding necessary health information. Gaps in health literacy can lead to patients misunderstanding their health care providers’ guidance or failing to seek care for specific symptoms. Inequities in health literacy are more pronounced in BIPOC communities than in white communities, likely due to socioeconomic and educational factors.10
Social and Community Context and the Built Environment
Neighborhoods vary in physical safety as determined by crime rates, measured pollutants, age of buildings and quality infrastructure, and the availability of outdoor spaces. Interventions at all levels of government can support health and promote built environments that encourage safety, community engagement, and physical activity.11
It’s widely accepted that physical activity plays a pivotal role in preventing and managing disease. Unsafe built environments—such as neighborhoods where walking outside poses a risk due to inadequate distance from the road or crime—thus have downstream impacts on chronic disease and national health care costs. Investments in the construction of neighborhood parks, community gardens, athletic facilities, trails, and natural preservation can lay the foundation for access to safe and enjoyable physical movement.12
An individual’s relationships and social interactions with their family, friends, colleagues, and communities positively impact their overall well-being. Social isolation and loneliness, which are highly prevalent in American society, are now recognized as contributing to morbidity and early mortality. Lack of social and community support can drive negative coping strategies—such as excessive alcohol and drug use—in response to mental illness or emotional difficulties.13 These support systems can be improved through an emphasis on inclusive (ie, accessible and safe for all) built environments and positive community attitudes (ie, acceptance and inclusion regardless of identity) to offer individuals a sense of belonging, comfort, and safety to flourish.14
Health and Health Care
Discrepancies in access to quality health care in the United States are multifactorial. Many Americans, about 10%, are uninsured. Without health insurance, individuals are less likely to have a primary care provider and more likely to postpone or forgo necessary medical care and medications, including preventive services and routine lab tests.15 Historical marginalization exacerbates inequities in insurance coverage: In 2019, compared with white Americans, Native Americans and Alaska Natives, Hispanic Americans, and Black Americans were 2.8, 2.6, and 1.5 times more likely to be uninsured, respectively.16
The COVID-19 pandemic has widened the gap in health-related inequities even further. Recent data from the CDC indicate that Native Americans and Alaska Natives had an age-adjusted COVID-19 hospitalization rate about three times that of non-Hispanic white Americans, while rates among non-Hispanic Black and Hispanic/Latinx Americans were both about 2.3 times the rate of white Americans.17 Several factors, including health conditions, dense living conditions, access to health care, employment as an essential worker, and systemic racism, contribute to these disproportionate rates.
Access to Care
Geographical differences in health care are rooted in the economic well-being and predominant demographics of the region. Higher-income communities and individuals who aren’t part of marginalized groups have greater access to high-quality health care.15 There’s also variation in regional utilization of health care services among rural, regional, and urban communities, possibly due to instability of resources, including variations in primary care physician and clinic presence, legal obstacles related to citizenship, lack of transportation, literacy or language barriers, and discrimination.18
Telemedicine has proven to be successful for improving the efficiency and effectiveness of health care while containing costs. This modality improves access to care for both urban and rural communities but often doesn’t address access for historically marginalized patient groups. Telemedicine and other health technologies can be used to monitor patients in their homes (eg, evaluating fall risk), decrease hospital lengths of stay, address health care staffing shortages, and offer consistent support for patients who may struggle to follow prescribed therapies.19,20
Quality of Care
Inequities also emerge in the quality of care typically available to those in historically marginalized groups, including differences in the efficacy of diagnostic and treatment methods. Health care providers unconsciously and/or consciously may treat patients from historically oppressed groups differently. For example, research suggests that BIPOC patients are less likely than white patients to receive organ transplants or interventions for pain despite medical necessity.21,22 In addition, this bias drives poor provider communication with, especially, people of oppressed races/ethnicities, further negatively affecting health outcomes.22
Care Costs and Outcomes
Health care spending in the United States is projected to grow 5.4% annually, reaching $6.2 trillion by 2028.23 Ninety percent of the nation’s current $4.1 trillion in annual health care expenditures are attributed to chronic disease and mental health conditions, rates of which vary by race/ethnicity.24
Nutrition-related chronic disease states are more prevalent in BIPOC communities. These include rates of obesity (49.6%, 44.8%, 17.4%, and 42.2% among Black, Hispanic, Asian, and white Americans, respectively), diabetes (14.7% among Native Americans and Alaska Natives, and 12.5% of Hispanic, 11.7% of Black, 9.2% of Asian, and 7.5% of white Americans), and hypertension (56%, 39%, 46%, and 48% among Black, Hispanic, Asian, and white Americans, respectively.25-27
Mortality rates among these groups also demonstrate inequities. For example, Black Americans have been documented to have the highest mortality rates for most major cancers and the highest infant mortality rate (2.3 times that of non-Hispanic white Americans).28,29 With new information available, experts have begun to question whether increased mortality has more to do with stress and inequities than racial identity.22 Recently, more studies have begun to investigate the effects of epigenetic changes, which can cause negative health effects of stress (allostatic load) and trauma passed from generation to generation, increasing health disparities in the children of those in historically oppressed groups. Epigenetic changes don’t change a person’s genetic sequence but alter how those genes are expressed.6
Moving Forward: Strategies for Equitable Health Care
RDs are well positioned to address health inequities and disparities through promoting equitable access to healthful and culturally appropriate foods, advocating for, and practicing cultural humility, and combating bias in the health care system. In addition, any health care team members who focus on the nutrition status of their patients can incorporate strategies to combat nutrition-related inequities.
Food Is Medicine Interventions
Food is Medicine (FIM) is a concept that leverages the role of community benefit organizations in revamping health care to prevent, treat, and manage nutrition-related illnesses.30 Popular FIM interventions include those in the table below.
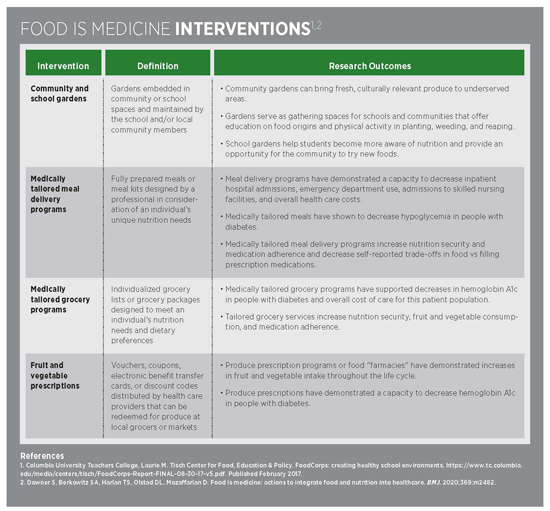
Investments in interventions such as FIM connect several domains of health (eg, health care, community, school, personal habits) and can confer benefits in access to nutritious, culturally appropriate foods that build healthful habits and drive equity in health outcomes.
Community-led advocacy heightens awareness of necessary policies and practices that influence the SDoH responsible for disease and compromising the effectiveness of health-related services in the local resident. However, community organizations and individuals should be the ones to identify a community’s needs rather than people and groups who don’t live in the community, such as public health experts. Interventions such as FIM must be community approved. In the spirit of asset-based care, community benefit organizations can maximize the strengths of a community, which eventually tend to improve weaknesses. Collaborations between health care providers, communities, and community members must prioritize the beliefs, customs, and values of the populations impacted by the interventions.31
Understanding Culture and Intersectionality
Culture comprises a structure of beliefs, practices, and values that influence the perspectives, communication styles, and behaviors of a group of people. Culture also affects how a person understands health, wellness, illness, disability, and death. All cultures are fluid and variation exists between individuals and subgroups of a culture, so assumptions never should be made about persons from a certain culture.32
Intersectionality is a concept that illuminates how social categories—eg, socioeconomic status, race, gender, disability status, LGBTQ+ identity—are interconnected. It’s often used to describe the overlap of different social inequities and how they shape a person’s experience in society and in relation to others. For example, two Black Americans both experience systemic racism; however, one individual also is transgender, has a disability, and has a poor socioeconomic status, while the other is cisgender and heterosexual, has no disabilities, and has a high socioeconomic status. According to the premise of intersectionality, these individuals have unique experiences and perspectives by the nature of how their identities overlap. These realities must be considered when exploring power imbalances in communities, schools, and health care settings, as each of these groups may require a different public health strategy or form of assistance. Recognizing differences and that individuals in a group have distinct needs and views helps ensure that public health measures promote equitable outcomes—ie, address the needs of all community members.33
Bias, Cultural Competence, and Cultural Humility
On a “micro” (individual) level, health care providers must interrupt their own biases to advance health equity and undertake public health measures and counseling. This interruption starts with introspection and challenging preconceived notions about cultural groups.
Practitioners also may choose to engage with Harvard University’s Project Implicit, which offers the Implicit Association Test to assess one’s attitudes and resulting biases.34
Although the terms often are used interchangeably, cultural competence and culturally humility are synergistic processes. The aim of cultural competency is to create a foundation for cross-cultural awareness and communication to provide more inclusive environments and care. Cultural competency can be a continuum toward building skill and awareness; however, to do so, one also must practice cultural humility.35 Cultural humility emphasizes that a provider has something to learn from their clients and patients and prioritizes connecting, listening, learning, and respect. It requires lifelong learning, self-critique, and understanding of the history and attitudes that have shaped life for people in traditionally oppressed communities through the present.36
Dietitians and other health care professionals can assess their personal readiness to engage in cultural humility and competency by asking themselves the following questions based on the acronym ASKED35:
• Awareness: Do I recognize my own biases and prejudices?
• Skill: Am I able to evaluate the patient’s physical and mental health, behaviors, and medications in a culturally specific manner?
• Knowledge: Do I understand the views of different cultures and how to address SDoH?
• Encounters: Do I have consistent meetings with people from cultures other than my own that promote understanding and help resolve cultural conflicts?
• Desire: Am I committed to engaging with this process?
Once providers have decided to commit to engage with the work of cultural competency and humility, they can use the following spectrum to evaluate their baseline and progress toward advanced competency and humility, as well as set goals for practice37:
• Cultural incapacity: Someone at this stage lacks recognition of history and context of oppression and has a limited skill set for working with people of other cultures. They perpetuate stereotypes and are paternalistic toward historically oppressed groups. This may be seen in, for example, an authoritative clinician who often adopts the role of decision-maker and dictates what would be best for the client or patient without their input.
• Cultural blindness: Someone at this stage diminishes and devalues individuals or communities by erasing differences. This is often referred to as “color-blindness” with regard to race, or the perspective that “we’re all the same; we’re all human.”
• Cultural precompetence: This individual has increased awareness of cultural differences but may hesitate to make or advocate for changes.
• Basic cultural competency: Someone at this stage accepts, understands, and respects differences by consistently asking for the opinions of members of traditionally oppressed groups.
• Advanced cultural competency: This individual actively interacts with and learns from diverse groups. They maintain humility as they do so and maintain a posture of lifelong learning.
When health care providers use the tenets of cultural humility and culturally responsive care, they can be equipped to engage with individuals and communities in a respectful and active way that promotes equitable health outcomes for all.
Improving Communication
In addition to using the tenets of cultural humility and culturally responsive care, effective communication between providers and their patients is essential for high-quality, equitable care. Fifty-eight percent of people who speak a language other than English at home self-report that they speak English “very well”; for others, however, interpreters can be difficult to access due to institutional shortages. Without access to an interpreter, patients may receive an incorrect diagnosis, misuse their medications, or fail to receive proper follow-up care.38
Moreover, patients with limited literacy have less knowledge of disease management, medication usage, and disease prevention than those with higher literacy levels.37 The National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care from the Department of Health and Human Services are foundational to providing effective, equitable, understandable, and respectful care that’s responsive to culture, learning style, health literacy, and ability.39
Providers should avoid ambiguous language and medical jargon or slang. Open-ended questions such as the following can be an effective way to gauge whether patients understand what’s being communicated:
• “What can you tell me about high blood pressure?”
• “Which foods will raise your blood sugar?”
• “Which foods do you normally eat during the day?”
Effective communication also must honor the whole person; gender identity, correct pronouns, and how a patient prefers to be addressed are important inquiries to include on an intake form or to cover in provider and patient introductions. For those with chronic diseases and/or disabilities, it’s generally preferred to use person-first language, such as “person with diabetes” rather than “diabetic.”39,40
Engage and Advocate
The American Health Information Management Association maintains a position statement on SDoH that may be a roadmap to encourage action and improvement through engagement and advocacy. It calls clinicians, informaticists, policy makers, and other stakeholders to do the following41:
• Establish standards to collect, use, maintain, and share SDoH data to support data- and outcomes-driven interventions.
• Promote health care delivery and financing models that integrate SDoH into the clinical setting in a culturally responsive manner.
• Build trust and foster authentic patient-provider relationships and communication that encourages patients to share their social struggles.
• Enhance the sharing of SDoH data between clinical and community partners to increase collaborative initiatives and sustainability.
Through the establishment, promotion, and enhancement of data-driven interventions and clinical-community collaborations, real change is probable. Possible outcomes include improved acute and chronic disease prevention and treatment technologies, and culturally responsive care and documentation within and outside of patient interactions.39
Putting It Into Practice
RDs are in a unique position to address SDoH when engaging in culturally responsive care. Active learning modalities that increase cultural competency and humility must be incorporated into nutrition and health education programs, including didactic programs in dietetics and supervised experiential learning for future RDs. In fact, these modalities have been included in the new 2022 accreditation standards and competencies for dietetic education programs.32
Innovative care strategies, such as FIM interventions, may present opportunities to address the disparities in health care access and quality in collaboration with communities affected by disparities and inequities. Telemedicine can improve access to and utilization of health care, as well as adherence to treatments.
But the call to interrupt disparity can’t be done alone. It must be accomplished in collaboration with patients, communities—including fellow health care providers—leaders, and policymakers.
— Cassie Vanderwall, PhD, RDN, CDCES, CPT, FAND, is a Madison, Wisconsin–based freelance food and nutrition writer and the manager of diabetes clinical services at Quartz Health Solutions.
Learning Objectives
After completing this continuing education course, nutrition professionals should be better able to:
1. Evaluate the historical roots of modern health inequities.
2. Distinguish the social determinants of health that influence nutrition-related health disparities.
3. Explore the projected impact of Food is Medicine interventions.
4. Employ strategies to address health disparities in nutrition education and advocacy.
CPE Monthly Examination
1. What is the primary difference between health disparity and health inequity?
a. Health disparities cause observed health inequities.
b. Health inequities are not preventable and are unjust.
c. Health inequities lead to health disparities.
d. Health disparities are the result of relational hierarchies.
2. Redlining is described as:
a. An act of racial segregation
b. A by-product of slavery in the United States
c. Commentary on maps to support just lending
d. Alteration of district lines to support a political party
3. The civil rights movement accomplished which of the following?
a. Distracted the public from inequities in rights
b. Reversed discrimination
c. Advanced rights for Black Americans
d. Made sustainable progress in economic disparity
4. Some research suggests that a single traumatic event is ____ harmful to overall well-being compared with exposure to ____ microaggression(s).
a. Less, chronic
b. Equally, a single
c. Equally, several
d. More, chronic
5. Food is Medicine interventions include all but which of the following?
a. Medically tailored meal delivery programs
b. Fruit and vegetable prescription programs
c. Home-delivered meal kit programs
d. Community and school gardens
6. Which of the following statements does not accurately reflect culture?
a. Culture reflects our morals, customs, and identities.
b. Culture is static and does not change over time.
c. Culture serves as a roadmap for how we perceive the world.
d. Culture is a system of learned beliefs, principles, and traditions.
7. Which of the following is not a tenet of the acronym ASKED, which is often used by health care professionals to assess their readiness to engage in cultural competency?
a. Awareness
b. Skill
c. Knowledge
d. Environment
8. Which of the following accurately articulates cultural competency?
a. Cultural competency is more important than cultural humility.
b. Cultural competency is foundational to cultural humility.
c. Cultural humility exists apart from cultural competency.
d. Cultural competency is a spectrum starting with humility.
9. Which of the following is not an accurate use of people-first language?
a. Diabetic person
b. Person with a disability
c. Patients with obesity
d. Stroke survivor
10. Which of the following is not a tenet of honorable communication?
a. Person-first language
b. Use of correct pronouns
c. Respectful name traditions
d. Use of a family interpreter
References
1. The root causes of health inequity. In: Weinstein JN, Geller A, Negussie Y, Baciu A, eds. Communities in Action: Pathways to Health Equity. Washington, D.C.: National Academies Press (US); 2017.
2. The story of … smallpox – and other deadly Eurasian germs. PBS website. https://www.pbs.org/gunsgermssteel/variables/smallpox.html
3. Mejia M. The U.S. history of Native American Boarding Schools. The Indigenous Foundation website. https://www.theindigenousfoundation.org/articles/us-residential-schools
4. Gross T. A ‘forgotten history’ of how the U.S. government segregated America. NPR website. https://www.npr.org/2017/05/03/526655831/a-forgotten-history-of-how-the-u-s-government-segregated-america. Published May 3, 2017. Accessed March 2022.
5. American Psychological Association. Stress in America: the impact of discrimination. https://www.apa.org/news/press/releases/stress/2015/impact-of-discrimination.pdf. Published March 10, 2016.
6. Yehuda R, Lehrner A. Intergenerational transmission of trauma effects: putative role of epigenetic mechanisms. World Psychiatry. 2018;17(3):243-257.
7. About social determinants of health (SDOH). Centers for Disease Control and Prevention website. https://www.cdc.gov/socialdeterminants/about.html. Updated March 10, 2021. Accessed April 2022.
8. Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health. 2018;39:273-289.
9. Tamborini C, ChangHwan K, Sakamoto A. Education and lifetime earnings in the United States. Demography. 2015;52:1383-1407.
10. Rikard RV, Thompson MS, McKinney J, Beauchamp A. Examining health literacy disparities in the United States: a third look at the National Assessment of Adult Literacy (NAAL). BMC Public Health. 2016;16(1):975.
11. Neighborhood and built environment. Healthy People 2030 website. https://health.gov/healthypeople/objectives-and-data/browse-bjectives/neighborhood-and-built-environment
12. Increase the proportion of adults who walk or bike to get places — PA-10. Healthy People 2030 website. https://health.gov/healthypeople/objectives-and-data/browse-objectives/physical-activity/increase-proportion-adults-who-walk-or-bike-get-places-pa-10
13. Holt-Lunstad J. Social isolation and health. Health Affairs. June 21, 2020. https://www.healthaffairs.org/do/10.1377/hpb20200622.253235/full/
14. Community. Healthy People 2030 website. https://health.gov/healthypeople/objectives-and-data/browse-objectives/community
15. Health care access and quality. Healthy People 2030 website. https://health.gov/healthypeople/objectives-and-data/browse-objectives/health-care-access-and-quality
16. Artiga S, Hill L, Orgera K, Damico A. Health coverage by race and ethnicity, 2010-2019. KFF website. https://www.kff.org/racial-equity-and-health-policy/issue-brief/health-coverage-by-race-and-ethnicity/. Published July 16, 2021.
17. Disparities in COVID-19–associated hospitalizations: racial and ethnic health disparities. Centers for Disease Control and Prevention website. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/disparities-hospitalization.html. Updated May 23, 2022. Accessed April 2022.
18. Centers for Disease Control and Prevention. Strategies for reducing health disparities — selected CDC-sponsored interventions, United States, 2016. https://www.cdc.gov/mmwr/volumes/65/su/pdfs/su6501.pdf. Published February 12, 2016.
19. Snoswell CL, Chelberg G, De Guzman KR, et al. The clinical effectiveness of telehealth: a systematic review of meta-analyses from 2010 to 2019 [published online June 29, 2021]. J Telemed Telecare. doi: 10.1177/1357633X211022907.
20. Telehealth and remote patient monitoring. Telehealth.HHS.gov website. https://telehealth.hhs.gov/providers/preparing-patients-for-telehealth/telehealth-and-remote-patient-monitoring/. Updated April 22, 2022.
21. Brunelli SM, Hunt A, Colson C, Tentori F. Exploration of racial disparities in the kidney transplant process among dialysis patients. Paper presented at: American Society of Nephrology Kidney Week; October 25, 2020.
22. Ghoshal M, Shapiro H, Todd K, Schatman ME. Chronic noncancer pain management and systemic racism: time to move toward equal care standards. J Pain Res. 2020;13:2825-2836.
23. NHE fact sheet. Centers for Medicare & Medicaid Services website. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet. Updated December 15, 2021. Accessed March 2022.
24. Health and economic costs of chronic diseases. Centers for Disease Control and Prevention website. https://www.cdc.gov/chronicdisease/about/costs/index.htm. Updated June 6, 2022.
25. Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief. 2020;(360):1-8.
26. Centers for Disease Control and Prevention. National Diabetes Statistics Report 2020: estimates of diabetes and its burden in the United States. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
27. Facts about hypertension. Centers for Disease Control and Prevention website. https://www.cdc.gov/bloodpressure/facts.htm. Updated September 27, 2021.
28. Cancer and African Americans. U.S. Department of Health and Human Services, Office of Minority Health website. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=16. Updated August 26, 2021.
29. Infant mortality and African Americans. U.S. Department of Health and Human Services, Office of Minority Health website. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=23. Updated July 8, 2021.
30. Downer S, Berkowitz SA, Harlan TS, Olstad DL, Mozaffarian D. Food is medicine: actions to integrate food and nutrition into healthcare. BMJ. 2020;369:m2482.
31. von Hippel C. A next generation assets-based public health intervention development model: the public as innovators. Front Public Health. 2018;6:248.
32. McCabe CF, O’Brien-Combs A, Anderson OS. Cultural competency training and evaluation methods across dietetics education: a narrative review. J Acad Nutr Diet. 2020;120(7):1198-1209.
33. Bowleg L. The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267-1273.
34. Preliminary information. Project Implicit website. https://implicit.harvard.edu/implicit/takeatest.html. Accessed March 2022.
35. The process of cultural competemility. Transcultural C.A.R.E. Associates website. http://transculturalcare.net/the-process-of-cultural-competence-in-the-delivery-of-healthcare-services/
36. Masters C, Robinson D, Faulkner S, Patterson E, McIlraith T, Ansari A. Addressing biases in patient care with The 5Rs of Cultural Humility, a clinician coaching tool. J Gen Intern Med. 2019;34(4):627-630.
37. Vanderwall C, Anna E. Building cultural humility in dietetics to advance health. Presented at: WAND Annual Conference; April 9, 2021. https://cdn.ymaws.com/www.eatrightwisc.org/resource/resmgr/2021_annual_conference/handouts/1.2_wand_cultural_humility_2.pdf. Accessed June 2022.
38. Language and literacy. Healthy People 2030 website. https://health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/language-and-literacy
39. What is CLAS? Think Cultural Health website. https://thinkculturalhealth.hhs.gov/clas/what-is-clas . Accessed March 2022.
40. People first language. Office of Disability Rights website. https://odr.dc.gov/page/people-first-language. Accessed March 2022.41. American Health Information Management Association. AHIMA policy statement social determinants of health. https://www.ahima.org/media/pi4jj1on/ahima-sdoh-policy-statement.pdf. Accessed March 2022.



