Today’s Dietitian
Vol. 17 No. 9 P. 52
Learn about the three main reasons dairy foods are problematic for many patients and tips for helping them live symptom free.
Many people have removed dairy from their diets to prevent gastrointestinal (GI) symptoms, such as gas, bloating, and diarrhea, which make them uncomfortable. Perhaps they haven’t asked the question, “Why can’t I tolerate dairy?” Or maybe they have asked this question, but haven’t received an adequate answer.
Dietitians can help answer this question and play a central role in providing relief for clients who suffer from unwanted symptoms due to dairy food intake. However, to counsel patients effectively, RDs must be able to differentiate among a dairy allergy (immunoglobulin E [IgE] immune-mediated food hypersensitivity), a dairy sensitivity (non-IgE immune-mediated food hypersensitivity), and lactose intolerance (nonimmune adverse reaction). Differentiating among these three main causes of dairy-induced food reactions is crucial to providing appropriate counsel and treatment.
The USDA and the Department of Health and Human Services jointly publish dietary guidelines every five years. The 2010 guidelines recommend Americans consume “low-fat milk and nonfat milk products” in their diets to ensure they meet daily requirements of calcium, vitamin D, and protein while limiting saturated fat. In addition, dairy alternatives are included in the USDA MyPlate recommendations. The new 2015 Dietary Guidelines Advisory Committee Report recommends healthful diet patterns that include low-fat/nonfat dairy or dairy alternatives without added sugars.1-3 As the 2010 Dietary Guidelines are being revised this year, it’s the perfect time for dietitians to address dairy intake, the three main causes of dairy-induced food reactions, and strategies for counseling clients.
Dairy Allergy
A food allergy is one of the three chief reasons a person may feel ill after consuming dairy products. Food allergy, as defined by the American Academy of Allergy, Asthma, and Immunology is a condition caused by an IgE-mediated reaction to a food substance. In the allergic individual, the body’s exposure to allergens stimulates lymphocytes (specialized white blood cells) to produce and release IgE antibodies. The IgE antibodies circulate through the blood and attach to the surface of cells, such as mast cells. Mast cells are specialized cells that store chemicals, such as histamine, and are found in all tissues of the body. When a person eats a food to which he or she is allergic, IgE antibodies on the surface of mast cells trigger the release of histamine and other chemicals. These substances cause various food allergy symptoms in the tissues in which they’re released, such as the nose, throat, lungs, skin, and GI tract.4
Symptoms of an allergic reaction develop quickly and can include reddening or swelling of the face, lips, eyes, tongue, and throat. Itching of the mouth, lips, and tongue also are signs of a severe allergic reaction. A runny or congested nose and sneezing also may develop. Hives or a rash may emerge on the skin. Coughing or wheezing is common in an allergic reaction involving the upper respiratory system. Nausea, cramping, abdominal pain, diarrhea, and vomiting may occur as the GI tract attempts to rid the body of the offending food. Decreased blood pressure, fainting, chest pain, heart rhythm abnormalities, and even death can occur with the progression of a severe allergic reaction.5
To determine whether someone has a dairy food allergy, an allergist may perform a skin prick test (SPT), a radioallergosorbent blood test, or an enzyme-linked immunosorbent assay blood test. About 50% to 60% of all SPTs are false positives; the test indicates a positive result, but the patient isn’t actually allergic to the food tested. In addition, as with skin testing, false positives are possible with blood tests; positive blood test results don’t conclusively establish that one has a food allergy. Nonallergic causes of raised IgE levels include dermatitis, asthma, and parasitic infection. Conversely, a negative test result doesn’t necessarily exclude a clinically significant allergy. Therefore, when making a diagnosis, it’s important to take into account symptoms that one experiences after consuming various types of dairy products.6-8 The patient’s history and the results of skin prick testing or the measurement of food-specific IgE antibodies in the blood should encompass the diagnostic workup of a suspected food allergy.8
However, because none of these parameters can accurately predict tolerance, the gold standard for diagnosing food allergy is still the double-blind, placebo-controlled food challenge.9 An oral challenge should only be done in an allergist’s office in the event of an anaphylactic reaction, which can be fatal. Initially, the dose of food is very small, but the amount is gradually increased during the challenge. The health care professional monitors the patient to determine if an allergic reaction takes place. If no reaction occurs, then presumably the individual isn’t allergic to the food that has been challenged.7
Currently there’s no cure for food allergy, although new preliminary research in the treatment of food allergy is showing promising results for some who are mildly to moderately allergic to milk. Jennifer Kim, MD, and colleagues in the department of pediatrics at the Jaffe Food Institute at Mount Sinai School of Medicine, studied the effects of dietary baked milk intake to determine whether it hastened the resolution of cow’s milk allergy in children. Kim and colleagues concluded that adding baked milk products to the diet of children who tolerate milk in a baked form appears to accelerate tolerance of unheated milk compared with strict avoidance.10 Dietitians can play a supportive role in the treatment of dairy allergic children who are tolerant of baked milk products by providing parents with recipes of baked dairy foods and recommending baked dairy products found in supermarkets. RDs also can offer parents suggestions to help their children avoid products containing dairy foods that are insufficiently heated and could potentially lead to an allergic reaction, such as pancakes, waffles, omelets, or pudding. Moreover, dietitians can provide suggestions to help ensure children get enough calcium and vitamin D for optimal bone growth and development.
Currently, if a patient has a severe allergy to dairy, he or she is instructed to avoid all dairy products, even in miniscule amounts. To that end, dietitians can teach dairy-allergic clients how to read labels and provide lists of ingredients that indicate the presence of dairy, such as caramel flavoring, natural flavoring, chocolate, lactoalbumin, sodium caseinate, whey, and confectioner glaze. Furthermore, dietitians can recommend dairy-free products, including spreads such as nut butters (eg, cashew, almond, peanut, hazelnut), mashed avocado, or hummus to take the place of cream cheese, butter, or dairy-based dips. Dietitians also can suggest dairy substitutions for cooking such as rice milk, almond milk, oat milk, hemp milk, fortified orange juice, nondairy cheese, and soy or almond yogurt. And they can discuss nutrient shortfalls that can arise from excluding dairy from the diet and recommend nondairy foods rich in those nutrients, such as calcium-fortified nondairy milk substitutes, nondairy cheeses, soy or almond yogurt, tofu, edamame, and calcium-fortified juices. If supplementation is necessary to compensate for nutrient gaps in the diet, dietitians can recommend well-absorbed, high-quality vitamin and mineral supplements, including calcium citrate and vitamin D3.
Dairy Sensitivity
Individuals who have ruled out IgE immune-mediated food hypersensitivity (food allergy) but who still experience symptoms after consuming dairy may have non-IgE immune-mediated food hypersensitivity (food sensitivity). Non-IgE immune-mediated food hypersensitivity can be defined as “any inflammation-generating reaction against a specific food or food component that doesn’t involve type 1 IgE-mediated hypersensitivity.”11 “Immunology research has begun to make clear the various mechanisms of the reaction of foods on the human body, and true food allergy mediated by IgE is probably only a small part of the problem,” says immunologist Jonathan Brostoff, MD, a professor emeritus of allergy and environmental health at King’s College London, and former head of the diagnostic immunology laboratory at University College London Hospitals. “The involvement of T-lymphocytes is now becoming recognized as well as other cells in producing the ‘late phase’ and ‘delayed’ responses that one sees clinically.”
According to Mark Pasula, PhD, an immunologist and a leading authority on adverse food reactions, the inflammatory process associated with food sensitivity is much more complicated than IgE-mediated food allergy because it includes multiple classes of reacting white blood cells and many proinflammatory mediators.11 Furthermore, food sensitivity can be responsible for a wide variety of symptoms, including, but not limited to, abdominal pain, gas, bloating, diarrhea, constipation, heartburn, headache/migraine, joint pain, eczema, sinus congestion, and postnasal drip.11,12
Since different mediators are involved in a food sensitivity reaction compared with a food allergy reaction, a different test must be administered to detect food sensitivity. One test that can be administered is the Mediator Release Test (MRT), a blood test that determines the degree of non-IgE immune-mediated hypersensitivity that one has to a food.8,11,13 When a food sensitivity reaction occurs, symptoms can be immediate or delayed up to several days after ingesting the offending food.
Moreover, food sensitivity is dose dependent. Some foods and chemicals can be tolerated in small amounts but not in higher quantities, while others may not be tolerated even in small doses. Unlike someone with a true dairy allergy, an individual with dairy sensitivity may be sensitive to one dairy product but not another. For example, a person may be able to tolerate milk but not cheddar cheese, or vice versa.14
To further complicate the diagnosis of an adverse dairy reaction, an individual may be sensitive to an antigen in the animal’s milk, aside from or in addition to the milk proteins. Mammalian mothers, including cows and humans, pass along antigens in their breast milk to their babies. The composition of both bovine and human milk is determined, in part, by what the mothers eat. To some extent, offspring will consume what their mothers ate when they drink their mother’s milk. “All feed flavors are absorbed through the cow’s system rather directly into the milk. Cows impart an odor and taste within 30 minutes of eating or breathing silage. It is strongest after about one hour,” according to the Penn State Extension, College of Agriculture.15 “Just as a breast-feeding woman may have to avoid foods her infant is allergic or sensitive to, we’ve noted many times that adults who are highly reactive to corn or soy, may react to milk from soy- and corn-fed dairy animals,” says Jan Patenaude, RD, CLT, director of medical nutrition at Oxford Biomedical Technologies. “This same person may tolerate dairy from a 100% grass-fed animal with no problems.”
To determine which dairy products are causing a reaction due to food sensitivity, RDs can employ an elimination diet, although it has some limitations. Symptomatic individuals usually are sensitive to several foods, not just one. Many people are sensitive to artificial and natural chemicals, which are difficult to pinpoint because they’re so pervasive in the food supply. In addition, people may begin experiencing symptoms up to four days after eating a food. Elimination diets can provide a clinician with more useful information than antiquated testing methods, but they may not be the best choice of treatment for someone with multiple food sensitivities or chronic symptoms.
A more effective option is to recommend MRT.11,13,14 This blood test is used to determine which of the 150 foods and chemicals tested are triggering reactions. “Food sensitivity management starts with identification of trigger foods and food chemicals,” Pasula says. “The more precisely practitioners can identify and remove inflammation-generating food items, the greater the clinical value of the method.”11
Using MRT results, dietitians can create an elimination diet specifically tailored to the patient’s unique needs.13 For those who have food sensitivity, avoiding their trigger foods for a period of time will enable them to regain tolerance to at least some of those foods. “Food sensitivity management is a dietary approach that often needs no supplemental intervention,” says Susan Linke, MBA, MS, RD, LD, CLT, owner of an integrative and functional nutrition-based private practice in Dallas, who specializes in immunology, adverse food reactions, and dietary treatment of food sensitivities. “It’s the perfect therapy suited for dietitians.”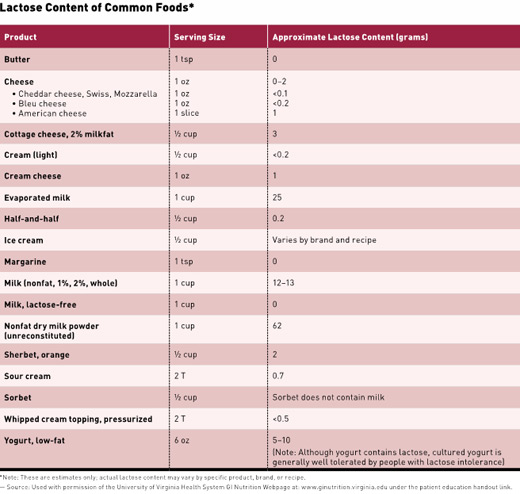
Lactose Intolerance
The third reason people may not tolerate dairy foods is lactose intolerance. If the small intestines don’t produce the enzyme lactase in sufficient quantities to break down the milk sugar lactose, a person typically experiences GI symptoms such as abdominal pain, gas, bloating, diarrhea, and sometimes vomiting. Causes of lactase deficiency include genetic predisposition, parasitic infection, celiac or Crohn’s disease, chemotherapy, small intestinal bacterial overgrowth, and small intestinal surgery.16
A breath test, blood test, and a stool test are available to determine if an individual is lactose intolerant.16 Some people who are lactose intolerant can tolerate eating aged cheeses and yogurt, but not foods containing a higher lactose content, such as milk and ice cream. However, lactose-intolerant individuals can tolerate lactose-free cow’s milk and other lactose-free dairy foods, in which the lactose has already been broken down. Some people who consume lactase enzyme tablets, available in most pharmacies and supermarkets, can tolerate a wide variety of dairy products. Dietitians can play a primary role in helping clients manage lactose intolerance through diet. And they can ensure patients meet their calcium and vitamin D requirements—nutrients that may be lacking in a dairy-free diet.
Final Recommendations
To safely maximize the intake of dairy products, diagnostic testing is essential to determine why dairy may be causing GI and other symptoms. While children with dairy allergy often outgrow it, adults tend to experience dairy allergy for a lifetime. On the other hand, both children and adults with food sensitivity usually regain tolerance to foods that once triggered symptoms, provided they avoid them for a period of time. People with lactose intolerance should limit dairy products to those low in lactose or replace dairy products with suitable nondairy or lactose-free dairy alternatives. They also can consider using a lactase enzyme supplement. Dietitians can help clients achieve optimal health by determining which dairy products, if any, they can safely consume. A client’s diet should include foods rich in calcium and vitamin D, and possibly a supplement if necessary to meet vitamin and mineral requirements they don’t get through foods.
“Dairy allergy, sensitivities, and intolerances often manifest in similar ways but can also have some differences,” Linke says. “Some patients have only one of those but some have all three simultaneously. Many people would much rather adopt a natural solution to their health problems than be dependent on supplements or medications.”
Renata Mangrum, MPH, RD, CLT, a private practitioner in the Washington, D.C., area, who specializes in food sensitivity, adds, “Our clientele is looking to dietitians for answers. Are we ready to step up to the challenge? If we don’t have the answers, it [will be] a missed opportunity.”
— Lori Langer, MEd, RD, LDN, CLT, is a nutrition consultant in private practice in Pennsylvania, who has teaching certifications in biology and general science. She specializes in food allergies, sensitivities, intolerances, and inflammatory conditions, such as irritable bowel syndrome, migraines, and fibromyalgia.
References
1. Dietary guidelines. US Department of Agriculture website. www.choosemyplate.gov/dietary-guidelines.html. Accessed June 13, 2015.
2. US Department of Agriculture, US Department of Health and Human Services. 2015 Dietary Guidelines for Americans. http://www.health.gov/dietaryguidelines. Published December 2014. Accessed June 13, 2015.
3. Scientific report of the 2015 Dietary Guidelines Advisory Committee. Part B. Chapter 2: 2015 DGAC themes and recommendations: integrating the evidence. Office of Disease Prevention and Health Promotion website. http://health.gov/dietaryguidelines/2015-scientific-report/04-integration.asp. Updated July 31, 2015. Accessed July 31, 2015.
4. Stöppler, MC. Food allergy: what causes allergic reactions to food? MedicineNet website. http://www.medicinenet.com/food_allergy/page2.htm. Accessed June 5, 2015.
5. Sampson HA, Muñoz-Furlong A, Bock SA, et al. Symposium on the definition and management of anaphylaxis: summary report. J Allergy Clin Immunol. 2005;115(3):584-591.
6. About food allergies. Food Allergy Research and Education website. http://www.foodallergy.org/diagnosis-and-testing/skin-tests. Accessed June 5, 2015.
7. Food allergy. National Institute of Allergy and Infectious Disease website. http://www.niaid.nih.gov/topics/foodallergy/understanding/pages/diagnosis.aspx. Updated February 29, 2012. Accessed June 5, 2015.
8. Laboratory tests in the diagnosis of allergic diseases. Australasian Society of Clinical Immunology and Allergy website. http://www.allergy.org.au/health-professionals/hp-information/asthma-and-allergy/tests-in-the-diagnosis-of-allergic-diseases. Accessed June 5, 2015.
9. Niggemann B, Beyer K. Diagnosis of food allergy in children: toward a standardization of food challenge. J Pediatr Gastroenterol Nutr. 2007;45(4):399-404.
10. Kim JS, Nowak-Wegrzyn A, Sicherer SH, Noone S, Moshier EL, Sampson HA. Dietary baked milk accelerates the resolution of cow’s milk allergy in children. J Allergy Clin Immunol. 2011;128(1):125-131.
11. Pasula MJ. The patented Mediator Release Test (MRT): a comprehensive blood test for inflammation caused by food and food-chemical sensitivities. Townsend Letter. 2014;62-66.
12. Pasula, MJ. Particle size measurement in suspensions. Part 2: an in vitro procedure for screening adverse reactions to foods and chemicals. Am Clin Lab. 1999;18(9):14-15.
13. Williams FH. Use of the LEAP mediator release test to identify non-IgE mediated immunological food reactions that trigger diarrhea predominant IBS symptoms results in marked improvement of symptoms through use of an elimination diet. Research presented at: American College of Gastroenterology Annual Meeting; November 2004; Orlando, FL.
14. Department of Laboratory Technology, Department of Medical Nutrition Therapy, Signet Diagnostic Corporation. The clinical significance and utility of laboratory testing for delayed-type hypersensitivity reactions to food antigens in the irritable bowel syndrome. http://nutritionadvancement.com/uploads/Z_CLINICAL_REVIEW_IBS_1_3.pdf. Published January 1, 2009.
15. Troubleshooting milk flavor problems. Penn State Extension website. http://extension.psu.edu/animals/dairy/nutrition/nutrition-and-feeding/troubleshooting-guides/troubleshooting-milk-flavor-problems. Accessed June16, 2015.
16. Diseases and conditions: lactose intolerance. Mayo Clinic website. http://www.mayoclinic.org/diseases-conditions/lactose-intolerance/basics/symptoms/con-20027906. Accessed June 5, 2015.


