Today’s Dietitian
Vol. 27 No. 5 P. 32
Sneezing, runny nose, itchy eyes, congestion, headache … all signs of the changing seasons for many. Seasonal allergies are one of the most common chronic inflammatory conditions and affect over 50 million people worldwide.1 They can impair quality of life, lower productivity, and disturb sleep. Diet and lifestyle modifications can be an effective part of the prevention and treatment of seasonal allergies, and dietitians can play a role in helping educate individuals on the most appropriate nutrition support for symptom management.
Seasonal allergies, also known as hay fever or allergic rhinitis (AR), result from a complex interaction between the body’s immune system and environmental antigens.1,2 The most common triggers include tree pollen, grass pollen, mold, and ragweed.3 When the body is exposed to these allergens, histamine is released and this can lead to more inflammation, fatigue, and other symptoms. A cascade of events starting within the nasal mucosa with an immunoglobulin E–mediated response leads to bothersome symptoms such as nasal itching, sneezing, rhinorrhea, and nasal congestion.2, 3
In North America, spring allergies often start in February and last through summer. Those with allergies to ragweed may suffer from symptoms in late summer to fall. According to the American College of Allergy, Asthma, & Immunology1, the following facts are key for understanding when individuals may experience more problems with seasonal allergies:
• Pollen thrives when it is cool at night and warm during the day.
• Molds grow quicker in heat and high humidity.
• Pollen levels peak in the morning.
• Rain washes pollen away but counts increase after rainfall.
• Pollen counts surge on windy, warm days.
Research Supports Diet-Seasonal Allergy Connection
Both epidemiological and clinical studies over the last 20 years have supported the notion that diet can positively impact those suffering from seasonal allergies.4 Incorporating dietary changes may be a practical and affordable strategy for sufferers to take control of their symptoms and find relief. However, the majority of studies on this topic have been observational, not experimental. While there are some higher-quality controlled trials, more are needed before we can offer firm guidance on certain points.
Immunonutrition refers to using a dietary approach to modulate specific mechanisms involved in immune and inflammatory pathways.4 Immunonutrition strategies for seasonal allergies aim to prime the immune system to properly respond, calm excessive inflammation, and provide the body with antiallergic supportive nutrients.2,4,5
Dietary Foundations for Seasonal Allergy Prevention
Multiple studies have found that a diet with excessive calories, saturated fat, and lower dietary fiber, such as the typical Western diet, may increase the risk of seasonal allergies through various mechanisms, including its negative impact on the gut microbiome.2,4,6 Alternatively, a Mediterranean dietary pattern rich in plant-based foods such as fruits, vegetables, and unsaturated fats from olive oil and omega-3-rich fatty fish has been linked to a lower risk for seasonal allergies.4
To provide the body with what it needs to prevent and manage seasonal allergies, focusing on gut health and key dietary factors is a good starting point.2,4,7 These work together to create a foundation to protect against the overreaction of the immune system and support proper modulation of inflammation.2
Consider Gut Health
AR is thought to be related to dysregulation of the development of the intestinal mucosal immune system. Providing breastmilk during the first year of life may help reduce this risk in children. Breastfed infants may have a marked difference in their gut microbiome.5,7 The rich supply of galactooligosaccharides in breastmilk promotes the growth of beneficial Bifidobacterium and Lactobacillus, which may help reduce the risk of AR in children.5 Being fed breastmilk with higher amounts of omega-3 fatty acids was also associated with a decreased risk of developing allergic symptoms.5
Beyond breastfeeding, other factors may influence the developing infant microbiome such as Caesarian birth or antibiotic use during infancy.7 Probiotic supplementations has been effective in clinical trials to improve beneficial gut microbiota and correct undesirable changes in microbiota composition and function caused by antibiotic treatments or Caesarean birth.7,8
A healthy gut positively influences the immune system in older children as well. Multiple studies have found that certain probiotics may improve seasonal allergies in kids, particularly L. casei, L. rhamnosus HN001, L. gasseri, L. rhamnosus GG, and B. longum.5,9,10 Probiotic treatment may help decrease seasonal allergy symptoms and lower the need for over-the-counter medications for those who suffer from the condition.5
Studies in adults also show a connection between probiotic use and AR symptoms. In a 2022 systematic review and meta-analysis of clinical trials using probiotics to treat symptoms of AR, authors found that probiotics significantly relieved AR symptoms.9 However, these researchers also noted high heterogeneity in some results after subgroup analysis that led them to conclude more clinical trials are needed to gather more conclusive evidence on using probiotics to treat AR.
One recent study from Japan found that adequate dietary vitamin A intake (in carotenoid and retinol forms) was associated with decreased odds of AR, which they suggested may be related to the role of vitamin A in modulating intestinal immune responses. Additionally, they found that plant-rich diets abundant in fiber and certain carbohydrates as may be more typical in a Mediterranean diet pattern were associated with a Prevotella enterotype, which was also associated with lower incidence of AR.11
Studies on fermented foods have many limitations due to the high variability of microbial cultures and ingredients present. We are far from fully understanding how these foods may help with seasonal allergies, but it’s an exciting area of research. However, some preliminary research suggests intake of fermented foods can help maintain the integrity of the gut epithelial barrier and immune homeostasis.11,12,13
Some artificial sweeteners such as aspartame and sucralose may alter the gut microbiota, increase bacterial translocation, and increase allergy symptoms.4
Look at Dietary Patterns
Following a Mediterranean diet pattern may have protective effects on seasonal allergies.2,4,5 It is important to consider that different studies define the Mediterranean diet differently and use different methodology; however, they generally include guidelines for high intake of extra virgin (cold pressed) olive oil; vegetables including leafy greens, fruits, cereal grains, nuts/seeds, and pulses; moderate intakes of fish, other meat, and dairy products; and low intakes of eggs and sweets.2,4,5,14 This eating style also focuses on including a variety of sources of dietary fiber and fermented foods while limiting more heavily processed and fried foods, refined grains, and added sugars.
The Western diet, in contrast to the Mediterranean diet, is defined by many researchers as containing lower levels of antioxidants and higher levels of saturated fats, processed meats, added sugar, and omega-6 fatty acids (relative to omega-3s), with lower dietary fiber, all of which may increase the risk of allergic diseases.4,5
Understand the Role of Specific Nutrients
There is a dose-response effect for many nutrients and food components. Dosages of any nutrient exceeding estimated needs are not likely to bring any additional allergy relief or immune support and in some cases could even impair or harm the immune system. Therefore, it’s always important to consider dose and overall dietary context when considering the role of individual nutrients in immunonutrition.
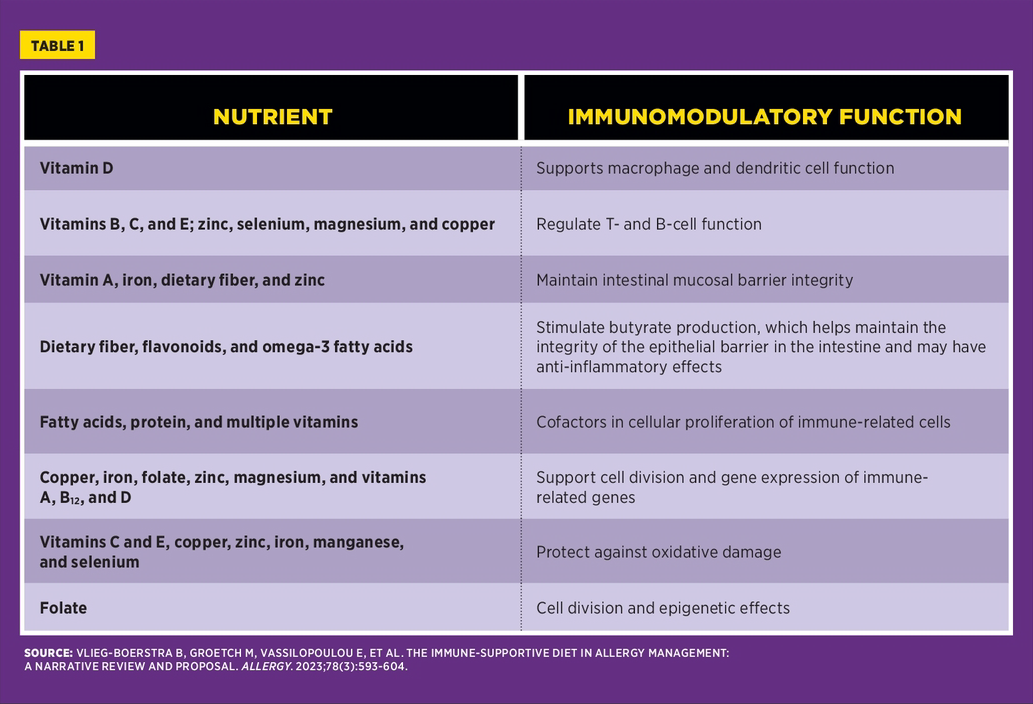
Table 1 details the mechanism behind different antiallergic nutrients.4,15
Use a Customized Approach
Although certain generalized dietary patterns show promise for standard recommendations, many RDs will appreciate that further customization based on individual needs, tolerance, and preferences is still a gold standard of applied nutrition in a clinical or counseling setting.
The concept of “atopic march” is thought to be a progressive allergic condition where sufferers may have eczema, food allergies, asthma, and/or AR in a connected pathophysiology.16 In these instances, avoiding or minimizing certain known triggers may help improve symptoms and management of these conditions. A careful assessment of individual tolerance is key to any successful dietary intervention.
If a patient notices symptoms of other inflammatory responses such as gastrointestinal discomfort, skin irritation/rash, or respiratory difficulties, it could be helpful to dig deeper for potential intolerances with discernment and care. Trialing temporary reductions or eliminations of certain foods to see if symptoms improve may be useful. However, sometimes people may unnecessarily restrict foods and elimination of nutrient-dense foods may lead to deficiencies in dietary fiber, B vitamins, iron, and calcium, which are also important nutrients for proper immune function.
Other techniques for addressing potential intolerances may include adjusting frequency of consumption or trying different preparation methods to help individuals discover what dietary approaches help them feel their best.
Supplements: A Word of Caution
It is common for people to reach for supplements instead of committing to broader diet changes; however, the research has not found micronutrient supplementation as a generalized approach to offer special benefit for seasonal allergies.2,4 Although research has linked vitamin D deficiency with increased AR risk and vitamin D supplements may be one option for helping deficient individuals meet needs and therefore reduce this risk, excess intake of this or any nutrient via supplementation may lead to adverse effects and caution should always be taken under professional guidance when administering such supplements.4
With regard to other types of supplements for AR, research is ongoing. Bioactive compounds such as quercetin are under review for their potential ability to alleviate AR symptoms. However, limited in vivo research has been conducted and most of it has taken place in animal models. More controlled human trials are needed.17,18
Taking a diet-centered approach to provide relief supports the body in multiple ways simultaneously. One study looking at adults aged 20 to 63 found that higher dietary diversity had a significant inverse dose-response relationship with allergic disease and AR in women.19 In this study, they quantified diversity through the Quantitative Index for Dietary Diversity, which calculates a score based on the proportions of foods from various food groups contributing to total food energy.
Summing It Up
An immune-supportive diet to help reduce the risk and severity of seasonal allergies should encourage diversity of nutrient-dense foods, meeting nutrient needs of the individual while limiting excess intake of trans- and saturated fats and added sugar and emphasizing antioxidant-rich and fiber-rich foods. A Mediterranean diet pattern, including foods rich in omega-3s (eg, fatty fish) and polyphenols (eg, berries, kiwis, pears, peaches, and avocados), may provide a good foundation to consider, though further individual customization based on food tolerance and other personal needs is important. Attention should be placed on gut health and supporting the microbiome through multiple avenues. Fermented foods and probiotics may have their place, though research still seeks to identify the most beneficial strains and doses. A whole-diet approach is likely more effective than an approach driven by supplements.
— Alyssa Salz, MS, RD, LDN, is a registered dietitian nutritionist in Northern Illinois, serving as the lead dietitian at Seattle Sutton’s Healthy Eating. In her role, she oversees nutritional standards, manages the Nutrition Ambassador Program, and provides personalized counseling to customers, drawing from her extensive experience in various areas of dietetics.
References
1. Allergy facts. American College of Allergy, Asthma, & Immunology website. https://acaai.org/allergies/allergies-101/facts-stats/. Accessed February 13, 2025.
2. Zhang P. The role of diet and nutrition in allergic diseases. Nutrients. 2023;15(17):3683.
3. Xie ZJ, Guan K, Yin J. Advances in the clinical and mechanism research of pollen induced seasonal allergic asthma. Am J Clin Exp Immunol. 2019;8(1):1-8.
4. Vlieg-Boerstra B, Groetch M, Vassilopoulou E, et al. The immune-supportive diet in allergy management: a narrative review and proposal. Allergy. 2023;78(3):593-604.
5. Hendaus MA, Jomha FA, Ehlayel M. Allergic diseases among children: nutritional prevention and intervention. Ther Clin Risk Manag. 2016;12:361-372.
6. Kim SY, Sim S, Park B, Kim JH, Choi HG. High-fat and low-carbohydrate diets are associated with allergic rhinitis but not asthma or atopic dermatitis in children. PLoS One. 2016;11(2):e0150202.
7. Navarro-Tapia E, Sebastiani G, Sailer S, et al. Probiotic supplementation during the perinatal and infant period: effects on gut dysbiosis and disease. Nutrients. 2020;12(8):2243.
8. Korpela K, Salonen A, Vepsäläinen O, et al. Probiotic supplementation restores normal microbiota composition and function in antibiotic-treated and in caesarean-born infants. Microbiome. 2018;6(1):182.
9. Luo C, Peng S, Li M, Ao X, Liu Z. The efficacy and safety of probiotics for allergic rhinitis: a systematic review and meta-analysis. Front Immunol. 2022;3:848279.
10. Sestito S, D’Auria E, Baldassarre ME, et al. The role of prebiotics and probiotics in prevention of allergic diseases in infants. Front Pediatr. 2020;8:583946.
11. Sahoyama Y, Hamazato F, Shiozawa M, et al. Multiple nutritional and gut microbial factors associated with allergic rhinitis: the Hitachi Health Study. Sci Rep. 2022;12(1):3359.
12. Chiu CY, Chan YL, Tsai MH, Wang CJ, Chiang MH, Chiu CC. Gut microbial dysbiosis is associated with allergen-specific IgE responses in young children with airway allergies. World Allergy Organ J. 2019;12(3):100021.
13. Wastyk HC, Fragiadakis GK, Perelman D, et al. Gut-microbiota-targeted diets modulate human immune status. Cell. 2021;184(16): 4137-4153.
14. Davis C, Bryan J, Hodgson J, Murphy K. Definition of the Mediterranean diet; a literature review. Nutrients. 2015;7(11):9139-9153.
15. Anshory M, Effendi RMRA, Kalim H, et al. Butyrate properties in immune-related diseases: friend or foe? Fermentation. 2023;9(3):205.
16. Vega F, Panizo C, Dordal MT, et al. Relationship between respiratory and food allergy and evaluation of preventive measures. Allergol Immunopathol (Madr). 2015;43(5):489-495.
17. Jafarinia M, Sadat Hosseini M, Kasiri N, et al. Quercetin with the potential effect on allergic diseases. Allergy Asthma Clin Immunol. 2020;16:36.
18. Roth-Walter F, Afify SM, Pacios LF, et al. Cow’s milk protein β-lactoglobulin confers resilience against allergy by targeting complexed iron into immune cells. J Allergy Clin Immunol. 2021;147(1):321-334.e4.
19. Katanoda K, Kim HS, Matsumura Y. New Quantitative Index for Dietary Diversity (QUANTIDD) and its annual changes in the Japanese. Nutrition. 2006;22(3):283-287.
20. Asha’ari ZA, Ahmad MZ, Jihan WS, Che CM, Leman I. Ingestion of honey improves the symptoms of allergic rhinitis: evidence from a randomized placebo-controlled trial in the East coast of Peninsular Malaysia. Ann Saudi Med. 2013;33(5):469-475.
21. Aw Yong PY, Islam F, Harith HH, Israf DA, Tan JW, Tham CL. The potential use of honey as a remedy for allergic diseases: a mini review. Front Pharmacol. 2021;11:599080.
WHAT ABOUT LOCAL HONEY?
Some believe that honey made from the pollen in one’s local environment may provide added support. According to research, local honey consumed in small doses may help individuals with seasonal allergies better modulate an immune response to the pollen in their surroundings.20 Although there is limited evidence, a 2021 mini review pointed to some studies showing remarkable improvements in certain types of allergic illnesses, including AR, and concluded that honey may be an effective antiallergic agent.21 However, it’s unclear which compounds are responsible for these effects and a more detailed mechanism of action may be needed to further justify its role as a standard therapeutic tool.
When consuming added sugar, including honey, it’s wise to take into consideration dietary recommendations for added sugar, appreciating individual glycemic response and the contribution of added sugar to the diet overall.