Today’s Dietitian
Vol. 25 No. 5 P. 38
CPE Level 1
On December 29, 2020, the USDA and US Department of Health and Human Services released the 2020 Dietary Guidelines for Americans (DGAs). The DGAs are updated every five years to equip health professionals with the most up-to-date information when providing guidance on what to eat and drink to meet nutrient needs and promote good health. Historically, the DGAs have focused on adults and children over the age of 2. The newest edition marks the first to provide specific recommendations across the lifespan, recognizing that each age and stage of life has unique nutrition needs. This includes new recommendations for pregnant and lactating women, as well as infants and toddlers aged 0–24 months. These populations are included in this edition as mandated by the Agricultural Act of 2014, which is a Congressional act that authorizes agriculture, food, and nutrition policies and programs.1 The addition of these stages acknowledges that good nutrition from pregnancy through a child’s second birthday is vital for brain development, growth, disease prevention, and establishing healthful dietary patterns later in life. Pregnancy and lactation are known to be times of high nutrient demand for mothers. Establishing a healthful diet pattern during this time is important to improve pregnancy outcomes, maintain health during pregnancy and postpartum, and restore nutrients that have been depleted during pregnancy.2
This continuing education course dives into the new recommendations for pregnant and lactating mothers, as well as children aged 0–24 months, and explores potential areas for expansion or revision in the future.
Pregnancy and Lactation
While eating healthfully is essential at any stage of life, during pregnancy and lactation is especially important due to increased calorie and nutrient demands. Following a balanced dietary plan can improve outcomes during pregnancy and lactation for both mother and baby and set the stage for healthful behaviors later in life.
Healthy US-Style Dietary Pattern for Adults
The four core principles set forth in the DGAs for adults are applicable during pregnancy. The first guideline recommended by the USDA is to “follow a healthy dietary pattern at every stage of life” to support health at the current stage of life and support continued health for the lifetime. Choosing healthful foods and beverages can prevent chronic disease and improve overall health status.2
The second core principle is to “customize and enjoy nutrient-dense food and beverage choices to reflect personal preferences, cultural traditions, and budgetary considerations.”2 While this concept isn’t new to the DGAs, putting it in the spotlight as a core principle acknowledges the diverse eating patterns of Americans and promotes inclusivity among cultural groups. Considering the racial disparities in maternal health, this distinction is significant.3 Recognizing that factors including culture and socioeconomic status influence eating patterns and choices also is important. One of the most common reasons cited for not following dietary guidelines is that “healthy food” is too expensive.4 Dietitians and health care providers should be conscious of recognizing and tailoring their recommendations to fit the unique cultural, personal, and socioeconomic constraints of their patients.
The final two principles in the DGAs are to “focus on meeting food group needs with nutrient-dense foods and beverages, and stay within calorie limits,” and “limit foods and beverages higher in added sugars, saturated fat, and sodium, and limit alcoholic beverages.” Americans should be consuming the majority of their calories from nutrient-rich foods such as vegetables, fruits, whole grains, low-fat dairy or soy alternatives, protein, and oils. Although the DGAs recognize that a small amount of added sugars, saturated fat, or sodium may be added to foods and still fit within a healthful dietary pattern, these nutrients should be limited.2
Weight Management
The DGAs source their weight gain recommendations during pregnancy from the National Academies of Sciences, Engineering, and Medicine. The guidelines for total weight gain recommended are as follows for each prepregnancy weight category and are based on a single pregnancy2:
• underweight (BMI <18.5): 28 to 40 lbs;
• healthy weight (BMI 18.5 to 24.9): 25 to 35 lbs;
• overweight (BMI 25 to 29.9): 15 to 25 lbs; and
• obese (BMI >30): 11 to 20 lbs.
It should be noted that the DGAs don’t provide references for healthy weight gain for twin or multifetal pregnancies. For women expecting twins, the National Academy of Medicine recommends a gestational weight gain of 37 to 54 lbs for those with a healthy weight, 31 to 50 lbs for women who are overweight, and 25 to 42 lbs for those considered obese. There’s currently insufficient data to make weight gain recommendations for triplet and higher-order pregnancies.5
Healthy weight gain during pregnancy is beneficial for infant and maternal health. It’s associated with lower rates of small- and large-for-gestational-age babies, macrosomia, cesarean delivery, gestational diabetes, preeclampsia, postpartum weight retention, and childhood obesity. In a 2017 systemic review and meta-analysis of more than 1 million pregnant women, 47% gained more than the National Academy of Medicine recommendations, while 23% gained less.6
Newer research suggests the weight recommendations may need to be adjusted. The American College of Obstetricians and Gynecologists notes that in overweight women, several studies have shown that a weight gain of 6 to 14 lbs, which is less than the current recommendation, wasn’t associated with poor fetal growth or negative neonatal outcomes. In addition, lower weight gain led to less postpartum weight retention compared with those who gained within the current recommendations.5
Currently, there’s no differentiation in the obese category between Class 1 (BMI of 30–34.9), Class 2 (BMI of 35–39.9), and Class 3 obesity (BMI of 40 or greater), which the National Academy of Medicine attributes to a lack of data to differentiate between groups. While gaining less weight than the National Academy of Medicine recommendations may have possible benefits including decreased rates of cesarean delivery, large-for-gestational-age babies, and postpartum weight retention, there are concerns that it may increase the incidence of small-for-gestational-age infants.5 The subject is nuanced, and more research is warranted.
Energy Needs
The DGAs recommend that pregnant women with a healthy prepregnancy weight should consume +0 additional kcal per day compared with prepregnancy needs in the first trimester, +340 kcal in the second trimester, and +452 kcal in the third trimester.2 There’s no mention of energy requirements needed for women who are overweight or obese before pregnancy, which is a gap of information considering 50% of women in the United States have a BMI classified as overweight or obese before becoming pregnant. There doesn’t seem to be a clear consensus on energy requirements for pregnant women with overweight or obesity, although newer research suggests that women with obesity don’t require any additional calories throughout pregnancy.7
Lactation during the first six months of an infant’s life requires an additional 330 kcal per day for the mother compared with prepregnancy needs. This number was determined by calculating 500 kcal per day for milk production but subtracting 170 kcal per day to account for postpartum weight loss. During the second six months of breast-feeding, additional maternal energy needs are set at 400 kcal per day. This is based on energy required for milk production and assumes weight maintenance.2 Aiming to achieve a healthy prepregnancy BMI and following energy and weight gain recommendations during pregnancy and postpartum can help prevent weight retention and avoid complications associated with overweight and obesity.2 The DGAs note that postpartum weight retention is common, however, stating that about half of women retain 10 or more pounds after one year.2 Practitioners should approach this topic with compassion considering the unique challenges of early parenthood. Increased family and work obligations, the stress of caring for a newborn, lack of childcare, a shifting focus away from self-care, and eating as a means to relieve stress are among the challenges new mothers face, which may hinder weight loss.8
Physical activity is a tool women can use to aid with appropriate weight gain during pregnancy and weight loss postpartum. The DGAs recommend at least 150 minutes per week of moderate-intensity aerobic activity, if possible. Women can continue with strength training and vigorous-intensity aerobic activity if they’d been doing these activities regularly before becoming pregnant. In addition to weight regulation, regular exercise conveys benefits to the mother and baby, including increased cardiorespiratory fitness, improved mood, and decreased risk of gestational diabetes.2
Nutrients of Concern
While the nutrients of public health concern for adults cited in the DGAs (eg, calcium, vitamin D, potassium, and fiber), apply to pregnant and lactating women, there are several additional nutrients specific to pregnancy that are mentioned for this population. These include folate/folic acid, iron, iodine, and choline.2
Folate/folic acid needs are higher during pregnancy than other stages because it’s essential to prevent neural tube defects. For women who aren’t pregnant, the RDA is set at 400 mcg dietary folate equivalents (DFE), while pregnant women require 600 mcg DFE.2 Because birth defects in the spine and brain occur around three to four weeks after conception, before many women know they’re pregnant, it’s recommended that all women of childbearing age take a supplement containing 400 to 800 mcg DFE daily and consume folate as part of a healthful diet.9 The DGAs note that only folic acid has demonstrated efficacy for preventing neural tube defects; however, dietary supplements generally contain either folic acid or 5-methyltetrahydrofolate (5-MTHF). 5-MTHF is a metabolically active form of folate, whereas folic acid is the synthetic form used to fortify food products because it’s more stable.9 Further examination of the benefit of 5-MTHFR in dietary supplements should be warranted given the frequency with which it’s used in supplements and the prevalence of people with MTHFR mutation, rendering them less able to convert folic acid into the active form.
Iron is another nutrient of concern for pregnant women. The RDA for nonpregnant women is 15 mg for females aged 14 to 18 and 18 mg for those aged 19 to 50. This jumps to 27 mg for all pregnant women. Because of the large increase in iron needs during pregnancy, iron deficiency is common, affecting approximately 10% of all pregnant women and up to 25% of pregnant women in their third trimester.2 The increased need for iron stems from the increase in blood volume required during pregnancy to supply oxygen to the baby.10 Heme iron found in animal foods, such as meat, poultry, and seafood, is more readily absorbed than nonheme iron found in plant foods, such as beans and leafy greens. Nonheme iron absorption can be increased by consuming these foods with a source of vitamin C. During lactation, iron needs drop considerably to 10 mg for women aged 14 to 18 and 9 mg for those aged 19 to 50 due to the lack of menstruation.2 Since prenatal vitamins often are formulated to meet the higher needs of iron during pregnancy, the DGAs recommend lactating women discuss appropriate levels of iron supplementation with their health care providers.2 Currently, the tolerable upper limit level of iron for pregnant and lactating women is 45 mg, which is based on the amount associated with gastrointestinal effects.11
Iodine supports neurocognitive development of the baby, so the needs of the mother increase during pregnancy and lactation. While most women consume adequate iodine, those who limit dairy, eggs, seafood, or iodized table salt may not be able to meet the increased demands of pregnancy. Many prenatal vitamins don’t contain iodine, so it’s important to check the label to confirm whether it’s included, especially with patients who may be at risk of deficiency.2
Similarly, choline needs are increased during pregnancy and lactation to support brain and spinal cord development. Good sources of choline include eggs, meat, seafood, beans, and lentils. Many prenatal vitamins don’t contain iodine or choline, so it’s important to ensure pregnant women consume sufficient amounts through dietary sources and/or find a prenatal supplement that includes these nutrients.2
The science of nutrition is always changing and expanding. There are several different nutrients that may benefit from a review in future DGA editions. Protein needs during pregnancy aren’t well-defined in the current version of the DGAs. At present, the range is set at 10% to 35% of total calories from protein, which would be 50 to 175 g of protein for a person consuming 2,000 kcal per day.2 The Cleveland Clinic suggests taking prepregnancy weight in pounds and dividing by two to determine protein needs (75 g for a 150 lb person),12 while the Mayo Clinic recommends 71 g per day.13 These recommendations are inconsistent and don’t differentiate between trimesters. One study suggests pregnant women require 1.2 g/kg of body weight during early pregnancy (16 weeks) and 1.52 g/kg during late pregnancy based on current body weight (36 weeks), suggesting protein requirements are higher than previously thought and vary at different stages of pregnancy.14
Vitamin D supplementation is another area that may benefit from further review. Presently, the RDA for pregnant and lactating women is set at 600 international units (IU)2; however, there’s evidence that higher doses may be needed to maintain serum vitamin D concentrations and provide optimal outcomes for mother and baby. Considering vitamin D is found naturally in only a few foods and many factors including skin tone, season, and location influence the body’s ability to make and absorb vitamin D, supplementation often is necessary.15 The American Pregnancy Association suggests that 4,000 IU of vitamin D daily may be necessary based on a recent study that found this dose to be most effective at preventing preterm labor and infections. The American College of Obstetricians and Gynecologists states that 1,000 to 2,000 IU of vitamin D generally is considered safe when deficiency is identified, and that even with limited data, most experts agree that up to 4,000 IU per day isn’t harmful. For routine pregnancies, they suggest awaiting the results of further clinical trials to determine dosage.16 Other experts suggest treating vitamin D deficiency with 4,000 IU per day and recommend routine supplementation with 1,000 to 2,000 IU daily; however, note that research is limited in first trimester use.17 One of the reasons determining optimal dosage has been difficult is the lack of consensus on what “optimal” serum levels of vitamin D are in pregnant women. While most agree on a minimum level of 20 ng/mL, some experts believe a circulating level of >40 ng/mL may be necessary.17
Seafood
Consuming 8 to 12 oz of seafood on a weekly basis is recommended in the DGAs during pregnancy and lactation.2 Seafood is a nutritious addition to the diet due to its content of omega-3 fatty acids, high-quality protein, and several vitamins and minerals, including vitamin D, calcium, selenium, zinc, and iodine.18 The omega-3 fatty acids found in fish and seafood are DHA and EPA, which are essential for the development of the brain, nervous system, and the baby’s vision. Mothers also benefit from adequate omega-3 intake as it reduces the risk of preeclampsia and depression. The best sources of EPA and DHA are cold-water fish, such as salmon, tuna, herring, sardines, and mackerel.19 Women should avoid seafood high in mercury because overconsumption can harm their own brain and nervous system, as well as adversely affect their fetus. King mackerel, marlin, orange roughy, shark, swordfish, tilefish (Gulf of Mexico), and bigeye tuna have the highest mercury levels and should be avoided. Ideally, women should choose from fish and seafood lowest in mercury, including clams, cod, haddock, salmon, shrimp, tilapia, and freshwater trout, among others.20
Vegetarian or Vegan Diets
Women who follow a vegetarian or vegan diet during pregnancy should pay special attention to certain nutrients that tend to be lacking in these dietary patterns. As previously discussed, iron deficiency is common during pregnancy among vegetarians and omnivores. Vegetarians or vegans may be at higher risk of deficiency because nonheme iron, found in plant foods, isn’t as readily absorbed as heme iron. Zinc, which is vital for normal growth and development, is similarly not as well absorbed when found in plant foods compared with animal foods due to the presence of phytates, which bind zinc and inhibit its absorption.21 Vegetarians can optimize the absorption of iron and zinc by consuming them alongside a vitamin C source and by using food preparation methods such as soaking, heating, sprouting, fermenting, and leavening.22
Vitamin B12 is found only in animal products, making it another nutrient of concern for vegetarians and vegans. Unborn children are at risk of neural tube defects, developmental delays, anemia, or failure to thrive if their mothers are vitamin B12 deficient during the pregnancy. Breast-feeding mothers who have inadequate B12 stores may cause deficiency in their infants.23 Vegetarians can get vitamin B12 from eggs and dairy; however, vegans will need supplemental B12 from either fortified foods or supplements.
As discussed, iodine and choline are nutrients of concern for pregnant and lactating women. However, the risk of deficiency is higher in vegetarian and vegans, as the highest source of these nutrients are animal products. Good sources of iodine include fish, seafood, and eggs, although seaweed is an excellent source of iodine that vegetarians and vegans may want to consume.24 The main dietary sources of choline are meat, poultry, fish, dairy, and eggs. Nuts, seeds, and whole grains also contain choline at lower levels.25
Finally, vegetarians and vegans need to consider where to obtain the omega-3 fatty acids DHA and EPA. Walnuts and flaxseeds contain a type of omega-3 called ALA, which isn’t linked to brain development and not well converted to DHA and EPA in the body.19 Vegetarians and vegans should consider taking an algae-based omega-3 supplement to meet their needs.
Foods to Limit and Avoid
Alcohol isn’t recommended in any amount for women who are pregnant or planning to become pregnant. For breastfeeding women, the safest option is to abstain from drinking; however, moderate consumption of one standard drink per day isn’t thought to be harmful, especially if consumed at least two hours before feeding or expressing milk.26
Caffeine can pass from mother to infant in breast milk; however, moderate amounts of caffeine shouldn’t negatively impact the baby. Consumption of less than 300 mg per day, the amount in approximately two to three cups of coffee, is considered safe.27
The DGAs advise pregnant women to discuss caffeine consumption with their health care providers. Per the American Pregnancy Association, there’s limited and/or mixed research on the safety of caffeine regarding miscarriage, birth defects, preterm delivery, reduced fertility, and other complications. Until there’s further research, pregnant women should consume no more than 200 mg caffeine per day.28
There are certain precautions pregnant women should take to prevent foodborne illness. They should cook seafood, meat, poultry, and eggs to the recommended minimum internal temperature. And pregnant women should avoid raw juice, raw milk products, and sprouts. Deli, luncheon meats, and hot dogs need to be reheated until steaming to kill Listeria. Moreover, they should follow general hygiene and food safety practices when storing, preparing, and consuming any foods.
Infants and Toddlers
The first two years of life are vitally important to the growth and development of children, which is why it’s notable that the 2020–2025 DGAs are the first to include this age range.
The First Six Months
Exclusive breast-feeding is regarded as the ideal form of nutrition for the first six months of life. The nutrients in breast milk are easily absorbed and meet the complete needs of an infant during this time frame, with the exception of vitamin D. Breast milk also provides antioxidants, enzymes, immunologic properties, antibodies, and substances that help soothe infants. Benefits for exclusively breast-fed babies include stronger immune systems, fewer respiratory illnesses and ear infections, lower rates of SIDS and infant mortality, and decreased risk of obesity in childhood, among many others.29
Infants who are exclusively or partially breast-fed require a vitamin D supplement of 400 IU daily due to low levels of vitamin D typically found in breast milk. Maternal vitamin D supplementation may be another option that isn’t as routinely recommended. Lactating women can increase vitamin D in their breast milk through oral vitamin D supplementation and/or increased sun exposure. Current research suggests that supplementing lactating mothers with 6,400 IU of vitamin D daily ensures adequate vitamin D in breast milk with the added benefit of stabilizing vitamin D stores in the mother.30 Vitamin B12 supplementation should be considered for breast-fed infants whose mothers are deficient or when intake is inadequate, such as with vegan diets.2
There are several reasons why infants may not be breast-fed, including the mother choosing not to breast-feed, adoption, poor maternal milk supply, difficulty latching, unsupportive work environment, lack of family support, pain with feedings, and concerns about infant weight gain or nutrition.31 Infants who aren’t receiving breast milk should be fed a commercially prepared, iron-fortified infant formula through the first year of life.2
When preparing breast milk or formula, mothers should take special care to ensure proper handling and storage. Instructions include washing hands before expressing or feeding milk, cleaning all pump and bottle parts before use, and sanitizing feeding items for premature or immunocompromised infants and infants under 3 months. Mothers should prepare powdered infant formula using a safe water source and follow instructions on the label. Once prepared, they can refrigerate the formula up to 24 hours.2 Freshly expressed breast milk should be refrigerated within four hours for up to four days. Previously frozen and thawed milk must be used within 24 hours. When preparing formula or breast milk, mothers should put it in a sealed container and place it in a bowl of warm water or under running tap water. They should use leftover milk from bottles within two hours for breast milk or one hour for formula.2
Complementary Foods
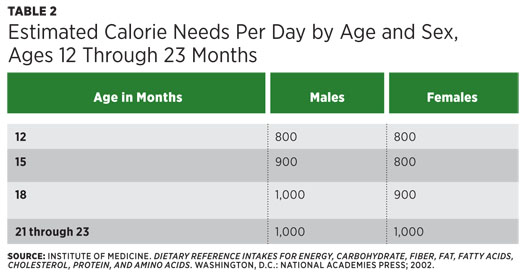
Complementary foods should be introduced between 4 and 6 months of age and when infants start to show signs of readiness, including the ability to control their head and neck, sit up independently or with support, put objects in or around their mouth, and grasp small objects. Around this age, complementary foods are critical for appropriate nutrient intake and to introduce the baby to a variety of foods and textures. For infants aged 6 through 11 months, nutrients of public concern include iron, zinc, protein, vitamin D, choline, and potassium. Iron and zinc are of particular concern for the breast-fed infant. Babies typically are born with adequate iron stores to last for the first six months; however, the iron content in breast milk is low and not impacted by maternal intake. Similarly, zinc content of breast milk is high and well-absorbed for the first six months, then declines and isn’t impacted by maternal intake. Therefore, complementary sources and/or supplementation of these nutrients as deemed appropriate by the child’s pediatrician is necessary. For children aged 1 year to 23 months, vitamin D, calcium, fiber, and potassium are underconsumed, while added sugars and sodium are overconsumed.2
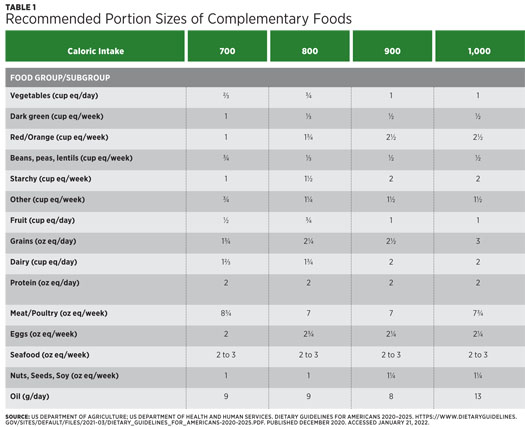
Introducing infants and young children to a variety of foods to provide a large array of nutrients and expand their palate is important. Infants are genetically predisposed to prefer sweet and salty foods and dislike bitter foods.32 It may take eight to 10 exposures to a new food before a child accepts it, especially bitter foods like cruciferous vegetables, so caregivers should be encouraged to continuously offer foods to children even if they initially don’t accept them. Children under age 2 should be offered food from across all food groups. Meats, poultry, eggs, seafood, nut butters, and soy products offer protein, iron, zinc, choline, and other nutrients. To minimize the risk of mercury exposure, seafood should be limited to two to three servings (one serving being equal to 1 oz for children aged 1 to 3) of low mercury fish per week. There’s no current recommendation for seafood consumption for children under age 1. Fruits and vegetables offer a wide variety of vitamins, minerals, and fiber with beans, peas, and lentils also providing a good source of protein. Grains, especially whole grains and grains/cereals fortified with iron, also are important for young children. Finally, dairy helps meet calcium, protein,
and vitamin D requirements of infants and toddlers. Whenever solids are started,
parents can introduce yogurt and cheese. Recommended portion sizes for children
aged 12 through 23 months based on caloric intake can be found in Table 1.
With regard to beverages, cow’s milk and fortified soy beverages shouldn’t be consumed before the age of 1 as they’re not suitable substitutes for breast milk or formula, and cow’s milk is difficult to digest for infants younger than 12 months. Whole milk or fortified, unsweetened soy beverages can be given after age 1. Other plant-based milk, such as almond, coconut, or oat milk, also are OK to include in small amounts after age 1 as long as they’re unsweetened. Caregivers should be advised that these drinks don’t have a similar amount of protein as cow or soy milk and may not be fortified. Therefore, they shouldn’t be considered a dairy equivalent. Parents should give up to 4 to 8 oz per day of water when they introduce complementary foods. After age 1, they can increase water intake gradually to ensure adequate hydration. Fruit juices should be avoided in the first year of life. After this, parents can include up to 4 oz of 100% fruit juice in a healthful diet plan, although fruit intake primarily should comprise whole fruit. They also should avoid all sugar-sweetened beverages. Lastly, toddler drinks aren’t needed as they include added sugars, and children can meet their nutrient needs through a balanced diet.2
Allergenic Foods
Introducing potentially allergenic food (eg, peanuts, eggs, dairy products, tree nuts, wheat, fish and shellfish, and soy) to infants can be scary for caregivers. The DGAs recommend introducing these foods when other complementary foods are initiated, as delaying their incorporation into the diet hasn’t been shown to prevent food allergies. Infants with an increased risk of peanut allergy may benefit from early introduction of age-appropriate peanut-containing foods at 4 to 6 months. It’s recommended that infants with moderate-to-low risk, including infants with mild-to-moderate eczema, introduce peanuts after 6 months.33
Foods to Avoid
Certain precautions should be taken to prevent choking. Babies should be sitting in a high chair or other safe place with adult supervision at all times, and food provided should be appropriate for children’s age and developmental level. The USDA recommends cooking hard foods until they’re soft enough to pierce with a fork, removing seeds and tough skins and peels from fruits and vegetables, and grinding up tough meats and poultry. Parents should chop food into thin strips or pieces no larger than a ½ inch or mashed or pureed. They also should cut in half round foods such as grapes, as they can easily block a child’s windpipe. Small (marble-sized), sticky, or hard foods are choking hazards, including dried fruits, fruit snacks, hard candies, hard pretzels, ice cubes, marshmallows, nuts and seeds, popcorn, spoonfuls of peanut butter, and round or tube-shaped foods like hot dogs.34
Choking concerns aside, parents should avoid feeding toddlers foods with added sugars and those high in sodium. Nutrient needs are high during this time frame and foods with added sugars take up space that should be reserved for more nutrient-dense foods. Exposure to very sweet or salty foods also is thought to increase preference for these foods later in life. Honey, which can contain the bacteria that causes botulism, and unpasteurized foods should be avoided due to the risk of developing foodborne illness. Finally, caffeine should be avoided because of potential negative health effects including insomnia, anxiety, headache, and lack of appetite.35 There’s currently no safe limit for caffeine for children aged 2 and under.
Responsive Feeding
The DGAs recommend responsive feeding from infants and young children. Responsive feeding is the practice of recognizing and responding to hunger and satiety signals from the child during feeding. This practice can help children learn how to self-regulate their intake, which can improve eating habits and promote weight management. Responsive feeding is a tool that can be used during breast- and bottle feeding as well as when parents introduce complementary foods. Signs a child is hungry include putting hands to mouth, turning towards the breast or bottle, smacking or licking lips, reaching for or pointing to food, opening the mouth when being offered food, becoming excited at the sight of food, and using sounds or hand motions to indicate hunger. Signs that a child is full include closing the mouth, turning the head away from the breast or bottle when offered, pushing food away, and using sounds or hand motions to indicate fullness.2
Supporting Healthful Eating (Pregnancy and Children)
There’s no denying the importance of healthful eating during pregnancy and throughout the first two years of life; however, there often are real or perceived barriers that prevent women and children from receiving optimal nutrition. Lower income families may benefit from the support of government programs such as WIC. According to the website, WIC serves “low-income pregnant, postpartum, and breast-feeding women, infants, and children up to age 5 who are at nutritional risk by providing nutritious foods to supplement diets, information on healthy eating, including breast-feeding promotion and support, and referrals to health care.”36 SNAP is the largest food assistance program in the country and helps by providing monthly benefits participants can use to purchase food. The Child and Adult Care Food Program reimburses meals and snacks served at participating child care centers including the Head Start program. Breast-feeding mothers can take advantage of the free information on the USDA’s WIC Breastfeeding Support website, the US Department of Health and Human Services Office of Women’s Health Breastfeeding Guide, and the Your Guide National Breastfeeding Helpline (800-994-9662). The best way to support breastfeeding, however, is by advocating for workplace policies and quality childcare that allow women the time and freedom to pump breast milk when away from their child. A referral to a local breastfeeding support group, such as La Leche League, is another way to support breastfeeding mothers.37
Putting It Into Practice
The first 1,000 days, spanning from conception through the first two years of life, are known to be a critical period in the neurodevelopment, mental health, and overall physical health of a child, with consequences that can last into adulthood.38 The 2020–2025 version of the DGAs is the first to include recommendations for pregnant and lactating women as well as children from birth to age 2. It’s vitally important that this information is conveyed to pregnant women and parents/caregivers to support food nutrition and promote healthful outcomes. With nutrition science always expanding, staying on top of these recommendations and continuing to revise these guidelines to reflect best practices in the editions moving forward will help ensure healthier futures for generations to come.
— Kristin Sementelli, MS, RD, LDN, is a prenatal and women’s health dietitian based in Chicago.
Learning Objectives
After completing this continuing education course, nutrition professionals should be better able to:
1. Differentiate nutrients of concern for pregnant and lactating women and babies aged 0–24 months.
2. Counsel patients on foods that should be avoided or limited during pregnancy and lactation and for babies aged 0–24 months.
3. Evaluate signs of readiness for infants to start complementary foods.
4. Recommend programs to support healthful eating for pregnant women and children aged 0–24 months.
Examination
1. It’s recommended that pregnant women with a prepregnancy BMI of 18.5 to 24.9 (normal range) gain how much weight?
a. 11 to 20 lbs
b. 15 to 25 lbs
c. 25 to 35 lbs
d. 30 to 40 lbs
2. How many additional calories does a pregnant woman with a prepregnancy BMI of 18.5 to 24.9 (normal range) need during the third trimester?
a. +0 kcal
b. +342 kcal
c. +452 kcal
d. +500 kcal
3. Pregnant women should limit caffeine to how many milligrams per day?
a. 200 mg
b. 300 mg
c. 400 mg
d. No amount of caffeine is considered safe during pregnancy.
4. Which of the following is a sign that a child is developmentally ready to begin complementary foods?
a. Grasping small objects
b. Crawling
c. Rolling over
d. Babbling
5. Which nutrient is routinely supplemented in breast-fed babies?
a. Vitamin B12
b. Iron
c. Choline
d. Vitamin D
6. The RDA for which of the following nutrients decreases during lactation compared with pregnancy?
a. Iron
b. Calcium
c. Vitamin A
d. Vitamin B6
7. Which source of fish/seafood should be avoided during pregnancy and breast-feeding?
a. Shrimp
b. Swordfish
c. Salmon
d. Anchovies
8. When should peanut-containing foods be introduced to infants with high risk of allergy?
a. 4 to 6 months
b. After 6 months
c. After 1 year
d. Peanuts should not be given to children with high risk of allergies.
9. Which feeding method is recommended in the Dietary Guidelines for Americans for babies and toddlers?
a. Baby-led weaning
b. Spoon feeding
c. Scheduled feeding
d. Responsive feeding
10. How long can prepared formula be stored in the refrigerator?
a. 12 hours
b. 24 hours
c. 48 hours
d. It must be used immediately.
References
1. Agricultural Act of 2014: highlights and implications. United States Department of Agriculture website. https://www.ers.usda.gov/agricultural-act-of-2014-highlights-and-implications/. Updated August 20, 2019. Accessed February 23, 2022.
2. US Department of Agriculture; US Department of Health and Human Services. Dietary Guidelines for Americans 2020–2025. https://www.dietaryguidelines.gov/sites/default/files/2021-03/Dietary_Guidelines_for_Americans-2020-2025.pdf. Published December 2020. Accessed January 21, 2022.
3. Oribhaber G, Nelson M, Buchanan-Peart K, Cancarevic I. A mother’s cry: a race to eliminate the influence of racial disparities on maternal morbidity and mortality rates among black women in America. Cureus. 2020;12(7):e9207.
4. US Department of Agriculture, Economic Research Service. Are healthy foods really more expensive? It depends on how you measure the price. https://www.ers.usda.gov/webdocs/publications/44678/19980_eib96.pdf?v=5977.1. Published May 2012.
5. Weight gain during pregnancy. American College of Obstetricians and Gynecologists website. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2013/01/weight-gain-during-pregnancy. Published January 2013. Accessed January 21, 2022.
6. Goldstein R, Abell S, Ranasinha S. Association of gestational weight gain with maternal and infant outcomes. JAMA. 2017;317(21):2207-2225.
7. Most J, St Amant M, Hsia D, et al. Evidence-based recommendations for energy intake in pregnant women with obesity. Clin Invest. 2019;129(11):4682-4690.
8. Toro-Ramos T, Heaner M, Yang Q, et al. Postpartum weight retention: a retrospective data analysis measuring weight loss and program engagement with a mobile health program. J Womens Health. 2021;30(11):1645-1652.
9. Folic acid. Center for Disease Control and Prevention website. https://www.cdc.gov/ncbddd/folicacid/about.html. Updated April 19, 2021. Accessed January 24, 2022.
10. Iron deficiency anemia during pregnancy: prevention tips. Mayo Clinic website. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/anemia-during-pregnancy/art-20114455. Updated October 25, 2019. Accessed January 24, 2022.
11. Iron fact sheet for health professionals. National Institutes of Health website. https://ods.od.nih.gov/factsheets/Zinc-HealthProfessional/. Updated March 30, 2021. Accessed February 28, 2022.
12. Pregnancy: nutrition. Cleveland Clinic website. https://my.clevelandclinic.org/health/articles/12593-pregnancy-nutrition. Reviewed January 1, 2018. Accessed February 28, 2022.
13. Pregnancy week by week. Mayo Clinic website. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/pregnancy-nutrition/art-20045082. Reviewed February 18, 2022. Accessed February 28, 2022.
14. Elango R, Ball R. Protein and amino acid requirements during pregnancy. Adv Nutr. 2016;7(4): 839S-844S.
15. Vitamin D and pregnancy. American Pregnancy Association website. https://americanpregnancy.org/healthy-pregnancy/pregnancy-health-wellness/vitamin-d-and-pregnancy/. Accessed March 2, 2022.
16. American College of Obstetricians and Gynecologists. Vitamin D: screening and supplementation during pregnancy. https://www.acog.org/-/media/project/acog/acogorg/clinical/files/committee-opinion/articles/2011/07/vitamin-d-screening-and-supplementation-during-pregnancy.pdf. Published July 2011. Accessed March 2, 2022.
17. Mithal A, Kalra S. Vitamin D supplementation in pregnancy. Indian J Endocrinol Metab. 2014;8(5):593-596.
18. Fish and shellfish. National Health Service UK website. https://www.nhs.uk/live-well/eat-well/fish-and-shellfish-nutrition/. Updated December 4, 2018. Accessed January 31, 2022.
19. Omega-3 fish oil and pregnancy. American Pregnancy Association website. https://americanpregnancy.org/healthy-pregnancy/pregnancy-health-wellness/omega-3-fish-oil-and-pregnancy/. Accessed January 31, 2022.
20. EPA-FDA advice about eating fish and shellfish. United States Environmental Protection Agency website. https://www.epa.gov/fish-tech/epa-fda-advice-about-eating-fish-and-shellfish. Accessed January 31, 2022.
21. Zinc fact sheet for health professionals. National Institutes of Health website. https://ods.od.nih.gov/factsheets/Zinc-HealthProfessional/. Updated December 7, 2021. Accessed January 24, 2022.
22. Saunders A, Craig W, Baines S. Zinc and vegetarian diets. Med J Aust. 2013;199(S4):S17-S21.
23. Vitamin B12 fact sheet for Health professionals. National Institutes of Health website. https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/. Updated April 6, 2021. Accessed January 24, 2022.
24. Iodine fact sheet for Health professionals. National Institutes of Health website. https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/. Updated March 29, 2021. Accessed January 31, 2022.
25. Choline fact sheet for health professionals. National Institutes of Health website. https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/. Updated March 29, 2021. Accessed January 31, 2022.
26. Alcohol. Centers for Disease Control and Prevention website. https://www.cdc.gov/breastfeeding/breastfeeding-special-circumstances/vaccinations-medications-drugs/alcohol.html. Updated February 9, 2021. Accessed February 28, 2022.
27. Maternal diet. Centers for Disease Control and Prevention website. https://www.cdc.gov/breastfeeding/breastfeeding-special-circumstances/diet-and-micronutrients/maternal-diet.html. Updated September 2, 2021. Accessed February 28, 2022.
28. Caffeine during pregnancy. American Pregnancy Association website. https://americanpregnancy.org/healthy-pregnancy/pregnancy-health-wellness/caffeine-intake-during-pregnancy/. Accessed January 31, 2022.
29. The benefits of breastfeeding for baby and for mom. Cleveland Clinic website. https://my.clevelandclinic.org/health/articles/15274-the-benefits-of-breastfeeding-for-baby–for-mom. Updated January 1, 2018. Accessed January 31, 2022.
30. Hollis B, Wagner C, Howard C, et al. Maternal versus infant vitamin D supplementation during lactation: a randomized controlled trial. Pediatrics. 2015;136(4):625-634.
31. Breastfeeding. Centers for Disease Control and Prevention website. https://www.cdc.gov/breastfeeding/data/facts.html. Reviewed August 24, 2021. Accessed March 4, 2022.
32. Forestell C. Flavor perception and preference development in human infants. Ann Nutr Metab. 2017;70(suppl 3):17-25.
33. National Institute of Allergy and Infectious Disease. Addendum guidelines for the prevention of peanut allergy in the United States. https://www.niaid.nih.gov/sites/default/files/addendum-peanut-allergy-prevention-guidelines.pdf. Accessed January 31, 2022.
34. United States Department of Agriculture. Reducing the risk of choking in young children at mealtimes. https://wicworks.fns.usda.gov/sites/default/files/media/document/English_ReducingRiskofChokinginYoungChildren.pdf. Accessed January 31, 2022.
35. Caffeine and children. American Academy of Child and Adolescent Psychiatry website. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Caffeine_and_Children-131.aspx. Published July 2020. Accessed January 31, 2022.
36. About WIC. US Department of Agriculture website. https://www.fns.usda.gov/wic/about-wic. Updated July 9, 2022. Accessed January 31, 2022.
37. La Leche League International website. https://www.llli.org. Accessed January 31, 2022.
38. Schwarzenberg S, Georgieff M. Advocacy for improving nutrition in the first 1,000 days to support childhood development and adult health. Pediatrics. 2018;141(2):e20173716.



