Today’s Dietitian
Vol. 21, No. 5, P. 44
Suggested CDR Learning Codes: 5000, 5150, 5400
Suggested CDR Performance Indicators: 8.1.5, 8.3.1, 8.3.6, 10.2.8
CPE Level 2
Take this course and earn 2 CEUs on our Continuing Education Learning Library
The number of people living after a diagnosis of cancer continues to grow in the United States. As of January 2016, more than 15.5 million Americans are living with a history of cancer, and that number is expected to increase to nearly 20 million in the next 10 years. Since the overall age-adjusted cancer incidence rate has declined over the past 10 years, this increase is due to the longer length of survival after diagnosis.1
The majority of cancer survivors (56%) were diagnosed 10 or more years ago, and 17% were diagnosed 20 or more years ago. Although there has been increased attention paid to young adults facing cancer, nearly one-half of cancer survivors (47%) are aged 70 or older, and only 5% are younger than 40. While the number of people living after a cancer diagnosis will increase in the next 10 years (mostly due to earlier detection), the distribution of cancer types and age is expected to stay the same.1
About 1.8 million new cancer cases are expected to be diagnosed in 2019 (not including noninvasive cancer or nonmelanoma skin cancers). The most common type of cancer diagnosis is breast cancer, followed by lung and prostate cancers.2
This continuing education course examines current research on nutrition for adults receiving radiation therapy and provides recommendations and strategies RDs can use when counseling clients and developing an oncology nutrition screening protocol.
Radiation Therapy
Radiation therapy uses high-energy radiation to shrink tumors and kill cancer cells. In the United States, approximately 50% to 60% of all individuals undergoing cancer treatment receive radiation therapy as part of their treatment.3 Radiation therapy for cancer treatment is used alone or in combination with other treatment, which could include surgery, chemotherapy, biotherapy, and hormonal therapy.
Radiation therapy kills cancer cells by damaging their DNA. Cancer cells whose DNA is damaged beyond repair stop dividing or die. When the damaged cells die, they’re broken down and eliminated by the body’s natural processes. This can be accomplished by damaging the DNA directly and/or by creating charged particles (free radicals) within the cells that can in turn damage the DNA.4
Radiation is targeted to the tumor via a variety of mechanisms. It may be delivered by a machine outside the body, which is called external-beam radiation, or it may come from radioactive material placed near cancer cells inside the body, known as internal radiation therapy or brachytherapy. Another method of delivering radiation is through a pill, eg, radioactive iodine, that travels in the blood to kill cancer cells.4
Radiation oncologists decide which type of radiation therapy to use and how to prescribe it based on several factors, including the type, size, and location of cancer in the body; the proximity of cancer to organs and normal tissues; how far the radiation must travel; the patient’s overall health and medical history; and whether other types of cancer treatment will be used.4
Radiation therapy is used for both curative intent and palliative care. When used with curative intentions, it’s typically given over the course of several weeks. Palliative radiation therapy may be given over a shorter period of time. The benefits of palliative radiation are improvement of quality of life, reduction of symptoms such as pain, slower disease progression, and reduction of the amount of obstruction the tumor is causing.5
Preventing and treating malnutrition in the oncology population is essential for best treatment outcomes and optimal quality of life. According to the Academy of Nutrition and Dietetics Evidence Analysis Library (EAL), “poor nutrition status is associated with higher rates of hospital admissions or readmissions, increased length of hospital stay, lower quality of life, and mortality in adult oncology patients.”6 The EAL also found poor nutrition status associated with decreased tolerance to chemotherapy and radiation treatment, meaning patients had worse side effects and were more likely to have to skip or delay a treatment.7 Significant loss of body weight is an indicator of poor prognosis and associated with decreased physical function and quality of life.8
MNT has been shown to be effective in improving multiple treatment outcomes for oncology patients,9 and RDs are uniquely trained to assist with screening, assessment, evaluation of nutrient needs, and management of nutrition impact symptoms—those that impede intake, digestion, or absorption.10 RDs’ nutrition interventions help patients adhere to their prescribed cancer treatment regimens, which is imperative for optimal outcomes including remission.
Nutrition Screening
Screening for malnutrition and malnutrition risk is essential for preventing poor outcomes. Rapidly dividing cells (eg, blood cells and gut mucosa) are the most susceptible to radiation damage; therefore, patients receiving radiation therapy are nutritionally at risk. Nutrition screening can help identify which patients require formal nutrition assessment, nutrition education, and a nutrition care plan.11,12
Oncology patients should be screened using one of five malnutrition screening tools validated for oncology patients: The Malnutrition Screening Tool for Cancer Patients, the Malnutrition Universal Screening Tool, the Malnutrition Screening Tool (MST), the Patient-Generated Subjective Global Assessment (PG-SGA), and the NUTRISCORE tool. Only the MST and the PG-SGA are validated for use in both inpatient and outpatient oncology settings.13,14
The MST is brief (three questions) and easily can be included in existing intake forms. In cases in which a tool can’t be used as designed, RDs should provide input regarding how to alter the tool to meet the needs of the institution and provide optimal patient care.
In January 2017, a study was published comparing the PG-SGA and MST with NUTRISCORE. The NUTRISCORE tool uses the MST as a base but has additional items, including tumor location and treatment, that helped improve sensitivity and specificity.15 This tool needs additional research and validation, but it’s something to follow, as it’s simple and accurate.
Factors that should be considered when developing a screening program in the radiation oncology setting include who’s going to do the screening (can the patient fill out the form independently or does it require a staff member), how much staff time is available to assist with the screening, and how the clients will be triaged once the screening has been completed (when referred to the RD vs receiving clinician-led education or no intervention).
Patient information included in most screenings include height/weight or BMI, weight change, presence/lack of appetite, disease severity, and presence of comorbidities.5
As part of the screening process, a protocol for referral needs to be identified. At minimum, it’s suggested that radiation oncology patients be referred to an RD when they score as high risk of malnutrition at baseline, develop malnutrition during treatment,12 and/or have certain diagnoses such as head and neck,16 esophageal, or pancreatic cancers.
Nutrition Assessment and Diagnosis
Once patients are referred to RDs for MNT, they’ll need to be evaluated. The in-depth assessment should address the following important areas of information9:
• nutrition intake (details regarding type of foods and beverages consumed, timing of consumption, and any changes in recent history of intake);
• anthropometric data (weight change over specific periods of time and current height, weight, and BMI);
• clinical data (such as relevant lab data, gastrointestinal function tests, inflammatory profile, and anemia profile);
• nutrition-focused physical status (age, body composition, changes in appetite, and changes in physical activity);
• client history (presence of comorbidities, depression, fatigue, pain, cancer treatment plan, and social factors); and
• stages of cancer cachexia, to be defined later.
In oncology, a diagnosis of malnutrition usually refers to undernutrition and changes in body composition. Malnutrition often is due to the cancer itself and/or to the impact of treatment. As previously mentioned, in ideal situations patients are screened and referred for assessment before they present with significant nutritional challenges and reassessed periodically throughout their treatment,12 but this isn’t always the case. Often, the RD receives a referral after significant malnutrition already is present.
A diagnosis of malnutrition is made when two or more of the following criteria are met17:
• insufficient energy intake;
• unintended weight loss;
• loss of subcutaneous fat;
• loss of muscle mass;
• localized or generalized fluid accumulation (this may mask weight loss); and
• reduced grip strength.
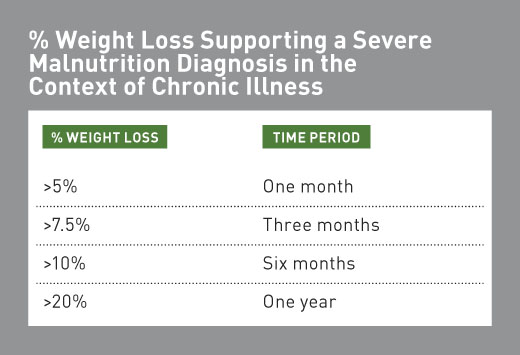
When evaluating unintended weight loss, it’s important to ask about weight loss before a diagnosis, as that’s sometimes what brings people to see their doctors. Unintended weight loss in the context of chronic illness should be interpreted as severe malnutrition if it meets the following conditions5:
Up to 80% of patients with advanced cancer may be diagnosed with cancer cachexia. Cancer cachexia, as stated in the EAL, is “a multifactorial syndrome characterized by an ongoing loss of skeletal muscle mass (with or without loss of fat mass) that can’t be fully reversed by conventional nutritional support and that leads to progressive functional impairment.” There are three stages of cancer cachexia: precachexia, cachexia, and refractory cachexia.18
Patients at high risk of weight loss or who have experienced unintended weight loss, in addition to patients with lung, pancreatic, head and neck, or gastrointestinal cancers, must be assessed for cancer cachexia. This can be achieved by identifying markers of inflammation, signs of wasting, and the presence of nutrition impact symptoms.19 If the patient is diagnosed with cancer cachexia, calorie and protein needs will increase.
It’s important to note that not all oncology patients struggle with unintentional weight loss or undernutrition. Many patients, specifically early-stage breast cancer and prostate cancer patients, gain weight during treatment, which has been proven to adversely affect outcomes. However, these patients aren’t typically referred to RDs because they aren’t at highest risk of undernutrition. When RDs see patients at risk of weight gain during treatment, they should encourage a healthful lifestyle. Modest weight loss, with approval from the patients’ oncologists, isn’t contraindicated.20,21
Protein and Calorie Needs
When estimating calorie and protein needs for patients undergoing radiation therapy, RDs must pay close attention to weight and adjust recommendations accordingly, as cancer itself and radiation therapy can alter patients’ metabolism.
Energy requirements are patient specific.22 Estimates of energy needs made by direct calorimetry, indirect calorimetry, and prediction equations attempt to mirror actual expenditures and account for changes in metabolic state.5 The recommended predictive equations will depend on the clinical status of the patient. RDs will need to use the appropriate equation depending on whether the individual is considered healthy, acutely ill, critically ill, or obese.5
Oncology dietitians use estimation of energy needs based on body weight often as an alternative to predictive equations. While kcal/kg equations lack scientific validation and aren’t accurate for critically ill patients, they’re a quick way to determine a baseline. Recommendations would then be adjusted based on outcomes.5 The 2002 American Society for Parenteral and Enteral Nutrition (ASPEN) guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients suggest energy need estimates should fall in the range of 20 to 35 kcal/kg.22 A 2017 European Society for Clinical Nutrition and Metabolism expert group for action against cancer-related malnutrition recommended that if resting energy expenditure (REE) and/or total energy expenditure can’t be measured directly, 25 to 30 kcal/kg/day is an appropriate target.12
Macronutrient needs for those receiving radiation therapy generally are the same as those for the general public: 20% to 35% of calories from fat; 45% to 65% of calories from carbohydrate; and 10% to 35% of calories from protein.23 Protein needs in the oncology population are 0.8 g/kg/day for healthy individuals; 1.2 to 2 g/kg/day for catabolic individuals; 1.5 g/kg/day for those who are metabolically stressed; and, for cancer patients in general, 1 to 1.5 g/kg/day of actual weight (1.2 to 1.5 g/kg/day serves as a target range to maintain or restore lean body mass).5,12
Among patients undergoing radiation therapy, some populations may have alterations in their metabolism that affect calorie and/or protein needs. For example, calorie needs may vary in head and neck cancer patients. One neutral-quality prospective, time series study found that the Harris-Benedict Equation (HBE), as compared with indirect calorimetry, underestimated the REE of head and neck cancer patients receiving radiation therapy. The researchers concluded that the HBE is unsuitable for use in determining the REE of advanced head and neck cancer patients receiving radiation therapy.24
Lung cancer patients also may represent a unique population. In one study, the estimated energy needs (using HBE) were within 5% of the measured energy needs, except for in male patients, who measured at higher than the estimated amount (113% HBE). Another study of males with lung cancer found that average measured REE was 112% HBE. Therefore, the calculated calorie needs may underestimate the actual energy needs of lung cancer patients.25
More research is needed to better define recommendations for actual grams of protein required as well, especially in patients undergoing pelvic or head and neck radiation.
One study presented in two reports assessed the protein intake of 15 patients undergoing radiation for pelvic malignancies. To prevent loss of fat-free mass, protein intake higher than the Recommended Dietary Allowance (RDA) is needed.26
Another study assessed the impact of protein intake on weight and body composition in 38 head and neck cancer patients receiving radiation. Patients’ protein intake decreased along with their weight and lean body mass. It appears that intake higher than the RDA is needed.27
Unless otherwise indicated by results of a nutrition assessment, cancer patients should aim for an intake of 100% of the RDAs for micronutrients. It’s safest to achieve recommended intake of micronutrients, especially antioxidants, via food, if possible.28
It’s imperative that RDs discuss with the medical team the need for enteral nutrition for patients with head and neck cancers. According to recent research, oral nutrition alone may not be adequate to maintain nutritional status during radiation therapy; enteral nutrition may be required. In one study, outpatient enteral nutrition resulted in improvement or maintenance of weight status and increased mean calorie and protein intake when compared with controls.29
Common Nutrition Impact Symptoms
Radiation therapy targets cancer cells and can damage normal cells, leading to side effects that usually appear during or immediately after completion of treatment. Late side effects of treatment, however, can happen months or years after radiation has been given. Side effects depend on the type of radiation, the total dose, the dose per treatment, how many treatments a patient receives, and whether radiation is combined with other cancer therapies.
Since rapidly dividing cells are the most susceptible to radiation damage and cells in the head and neck and gastrointestinal tract turn over more quickly than do those in other areas of the body, radiotherapy to the head and neck or the gastrointestinal tract is likely to lead to nutritional problems.8 A recent study showed that many head and neck cancer patients experience oral complications six months after radiation, affecting oral function and quality of life.30
Following are among the possible nutrition-related side effects of site-specific radiation therapy for patients treated with external-beam radiation5:
• Brain radiation: fatigue, nausea, and vomiting;
• Breast radiation: fatigue;
• Chest radiation (lung or esophageal cancers): fatigue, nausea, vomiting, and throat burn or pain;
• Head and neck radiation: fatigue, nausea, vomiting, throat burn, or pain, thick saliva, oral infections, and stiffness of the jaw;
• Pelvic radiation: diarrhea, fatigue, and urinary and bladder changes;
• Rectum radiation: diarrhea, fatigue, and urinary and bladder changes; and
• Stomach and abdomen radiation: diarrhea, fatigue, nausea, vomiting, and urinary and bladder changes.
Long-term nutrition impact symptoms are found mostly in patients treated for cancers of the head, neck, esophagus, colon, and rectum. These side effects include the following5:
• Esophageal radiation: esophageal stenosis, fibrosis, or necrosis;
• Gastrointestinal tract radiation: diarrhea, malabsorption, chronic colitis, and intestinal changes; and
• Head and neck radiation: trismus, permanent xerostoma, alterations in taste and smell, and dental problems.
Managing Radiation Therapy Side Effects
The range of side effects that can result from radiation therapy also have the potential to impede oral intake. This article highlights the most common and provides resources for finding information on less common side effects.
Diarrhea
Diarrhea is defined as an increase of three or more stools per day compared with the patient’s usual number or an increase in liquidity of bowel movements.
The following tips are helpful for clients experiencing diarrhea. RDs should advise patients to partake in the following practices5,14:
• Consume small, frequent meals.
• Consume a low-fat, low-fiber diet.
• Keep a detailed diet and symptom history to help identify problem foods or eating habits that contribute to the issue.
• Avoid gas-producing foods, caffeine, and alcohol.
• Consider using bulking agents, pectin, or high–soluble fiber foods to control diarrhea.
• Avoid sorbitol and other sugar alcohol–containing products.
In addition to offering these tips, RDs should consider advising patients to take a multivitamin and mineral supplement to make up for potential losses and malabsorption. Close monitoring of symptoms and communication with the medical team about any medication adjustments that must be made also are necessary.
Fatigue
Fatigue is a common side effect for many undergoing cancer treatment.
Cancer-related fatigue is defined as a “distressing, persistent, subjective sense of physical, emotional, and/or cognitive tiredness or exhaustion related to cancer or cancer treatment that’s not proportional to recent activity and interferes with usual functioning.” It’s one of the most common side effects in cancer patients.31
There are many possible causes, including anemia, inadequate energy and/or protein intake, weight loss, pain, medications, anticancer treatment, dehydration, and/or sleep disturbances.5 As there are so many potential influencing factors, it’s recommended that a qualified professional complete a full nutrition assessment that includes weight gain and loss, caloric intake changes, impediments to nutrient intake, anemia, and fluid and electrolyte imbalances.31
In addition to addressing any nutritional deficiencies and making sure the client is getting adequate calories and protein, it can be helpful to counsel patients on energy conservation.31 This strategy would involve getting adequate nutrition without spending too much energy on preparation.
Advise patients to do the following32:
• Use easy-to-prepare meals and snacks, prepared foods, and energy-dense foods.
• Keep nonperishable snacks at their bedside.
• Consume soft, easy-to-chew foods.
• Eat small, frequent meals.
• Eat well when appetite is best (usually first thing in the morning).
• Limit duties or chores to save energy.
• Encourage light activity to maintain muscle mass.
In addition to helping clients identify strategies for managing fatigue, RDs should monitor weight and modify intake plans as needed to stabilize patients’ weight. Since physical activity has been proven to help mitigate cancer-related fatigue, consider requesting a physical therapy consult for improving patients’ strength.33 In addition, RDs should consider advising the use of a multivitamin and mineral supplement if food intake doesn’t meet the patients’ needs.
Nausea and Vomiting
Nausea and vomiting can have a significant impact on nutrition intake. The nutrition professional should work with the medical team to use antinausea medications as appropriate. The timing of the antinausea medication is as important as the medication itself for improving food intake. RDs should encourage clients to take antinausea medication 30 minutes before eating so it’s fully in the client’s system when food is introduced.
To help mitigate nausea and vomiting, advise patients to do the following32:
• Eat five to six small meals per day.
• Limit exposure to food smells by avoiding food prep areas.
• Eat cool foods with little odor.
• Avoid greasy, high-fat foods.
• Consume fluids between meals, rather than with meals.
• Avoid strong smelling lotions, soaps, perfumes, and air fresheners.
• Rest with head elevated for 30 minutes after eating.
• Take nausea medicine as prescribed, focusing on 30 minutes before meals or timing meals when medications are working at their best.
• Take pain medicines with crackers or light food.
Mouth Changes
Patients with taste and smell changes have little or no sense of taste and smell or heightened sense of metallic, bitter, salty, or sweet tastes. Following treatment, normal taste may take up to a year to return.5
The following tips are helpful for clients facing taste and smell changes5,14:
• Have patients rinse their mouths or brush their teeth before eating.
• If foods have little or no taste, choose fruit marinades for meats or use lemon, herbs and spices, pickles, or hot sauce to season foods.
• If foods have an “off” taste, choose fruity and salty flavors and suggest sugar-free lemon drops, gum, or mints to improve mouth taste.
• For bitter or metallic tastes, eat using bamboo or plastic silverware or chopsticks and flavor water with lemon juice or other fruit flavors.
• For too salty, bitter, or acidic tastes, choose foods that are naturally sweet rather than salty or acidic and use low-sodium products.
• When meats taste bitter or strange, add fruit-based marinades or sweet and sour sauce or choose alternative protein sources such as eggs, tofu, dairy, or beans.
• If smells are bothersome, eat cool foods and avoid microwave ovens and food prep areas; use cups with lids and straws to mask odors.
RDs should encourage clients with damage to their taste buds to practice good oral hygiene, and periodically they’ll need to have a nurse or doctor evaluate their mouths for thrush. A good recipe for oral hygiene calls for mixing 3/4 tsp salt and 1 tsp baking soda in 4 cups water. Rinse mouth with 1 cup three to four times per day or as directed by a physician.5
Mucositis and esophagitis are inflammations of the mouth or esophagus usually described as a painful, irritated throat, or the feeling of a lump in the throat. Other symptoms may include indigestion, esophageal reflux, belching, feeling of fullness, and early satiety. Almost all patients receiving radiation for head and neck cancer will develop mucositis.34
For those with throat burn or pain, getting enough calories and fluids can be especially difficult. Many will require tube feedings to meet their needs. However, they should continue swallowing as much as possible to avoid atrophy of the swallowing muscles.
Clients may benefit from some of the following strategies5,14,35:
• Choose foods lower in acidity and avoid tomato products, citrus juices, and pickled foods.
• Choose foods that are less spicy and avoid chili, chili powder, curry, cloves, black pepper, and hot sauces.
• Choose foods softer in texture, with added moisture, sauce, or gravy.
• Choose cream soups, mashed potatoes, yogurt, eggs, tofu, and pudding.
• Serve foods that are cool or at room temperature.
• Prepare smoothies with low-acid fruits such as melons, bananas, or peaches, and add yogurt, milk, or silken tofu.
• Avoid alcohol, mouthwashes containing alcohol, and tobacco.
To encourage good oral hygiene, RDs can suggest patients use lidocaine gels and rinses to help combat mucositis.35 In addition, a sore throat gargle may help. Patients can mix 3/4 tsp salt and 1 tsp baking soda in 4 cups water. Gargle with 1 cup three to four times per day.5
In the past, glutamine rinses were thought to help with sore mouth. According to the EAL, there’s no evidence that directly supports or refutes that the use of oral glutamine can improve and support recovery from radiation therapy or reduce mucositis associated with radiation therapy.36
Patients with xerostomia will have abnormal dryness of the mouth that causes difficulty eating and talking, taste alterations, and/or thick saliva. Saliva stimulants or sialagogues, such as sugarless candies and chewing gum, may be used to stimulate saliva flow when functional salivary glands remain. However, in many patients receiving radiation therapy, salivary glands aren’t functioning. Pilocarpine is a pharmaceutical intervention indicated for the treatment of dry mouth symptoms from salivary gland hypofunction caused by radiation.37
Some nutrition strategies RDs can suggest for their patients include the following5,37:
• Eat frequent, small meals.
• Add broth, gravies, and sauces to meals and dunk dry foods in liquids.
• Sip liquids often throughout the day; aim for 8 to 10 cups per day.
• Chew on carrots or celery.
• Swish and spit with club soda or carbonated water.
• Use a humidifier at home to moisten air.
• Practice good oral hygiene (see previous suggestions for mouth rinses).
• Suck on hard candy, frozen grapes, or melon balls.
• Avoid alcohol and alcohol-containing mouthwashes.
Resources for information and tips on other cancer-related nutrition impact symptoms can be found in the National Cancer Institute’s publication “Eating Hints: Before, During, and After Cancer Treatment” (www.cancer.gov/publications/patient-education/eatinghints.pdf) and the American Institute for Cancer Research’s page “Dealing With Treatment Side Effects” (www.aicr.org/patients-survivors/during-treatment/cancerresource-side-effects.html). In addition, “Oncology Nutrition for Clinical Practice,” a comprehensive guide from the Oncology Nutrition Dietetic Practice Group, is available for purchase at www.eatrightstore.org/product-type/books/oncology-nutrition-for-clinical-practice.
Conclusion
RDs play an important role in caring for patients undergoing radiation therapy. Adult patients should be screened for malnutrition upon entry into oncology services. Early identification and management of malnutrition improves nutrition status and quality of life, which leads to improved outcomes. Furthermore, RDs should estimate and monitor patients’ nutrition needs depending on diagnosis, treatment effects, and clinical status. Managing the side effects of radiation therapy such as diarrhea, nausea, and taste changes is integral in maintaining quality of life and nutrition status.9
— Julie Lanford, MPH, RDN, CSO, LDN, is wellness director for Cancer Services in Winston-Salem, North Carolina. Lanford develops and manages survivorship and prevention programs and also writes the organization’s prevention and survivorship blog at CancerDietitian.com.
Learning Objectives
After completing this continuing education course, nutrition professionals should be better able to:
1. Demonstrate the need for nutrition interventions in the usual care of adult oncology patients undergoing radiation therapy.
2. Assess three common nutrition-related side effects that adults receiving radiation therapy may experience.
3. Employ nutrition strategies to address the common side effects that adults undergoing radiation therapy may experience.
CPE Monthly Examination
1. Which of the following cancers is not one of the most common cancer diagnoses (other than nonmelanoma and noninvasive cancers)?
a. Lung
b. Prostate
c. Leukemia
d. Breast
2. Which of the following factors do oncologists consider when determining a radiation therapy prescription?
a. The patient’s family history
b. How far radiation must travel to reach the cancer
c. The patient’s body composition
d. Percent of usual body weight
3. Poor nutrition status is associated with which of the following?
a. Decreased admissions and readmissions
b. Increased length of hospital stay
c. Decreased mortality
d. Low RD referral rates
4. Which tool has been validated for screening inpatient and outpatient oncology patients?
a. Malnutrition Screening Tool
b. Oncology Nurse Screening
c. Percentage of weight loss
d. NUTRISCORE
5. All oncology screenings should include which of the following characteristics of the patient?
a. Education level
b. History of diet adherence
c. Appetite
d. Amount of social support
6. Which of the following is a stage of cancer cachexia?
a. Multifactorial cachexia
b. Refractory cachexia
c. Protein loss cachexia
d. Oncocachexia
7. An RD is assessing a lung cancer patient for weight loss. The patient was diagnosed one month before meeting with the RD. To determine percentage of weight loss, how far in the past should the RD consider weight?
a. One week
b. Two weeks
c. One month before last stable weight
d. Date of last stable weight
8. Which equation is most appropriate for determining energy needs of oncology patients?
a. Harris-Benedict Equation
b. It depends on clinical status of the patient.
c. 25 to 30 kcal/kg/day
d. Mifflin-St Jeor Equation
9. Which of the following is an appropriate meal suggestion for an elderly patient who lives alone and has fatigue?
a. Peanut butter and banana sandwich with milk
b. Grilled steak and baked potato with tossed salad and vinaigrette
c. Homemade juice from locally sourced produce
d. Baked salmon, roasted broccoli, and fruit salad
10. For patients with radiation-induced mucositis, which of the following would be an appropriate strategy to suggest?
a. Enhance flavor of food by adding spices.
b. Gargle with a salt and baking soda solution.
c. Use Listerine or Scope mouthwash.
d. Consume acidic foods.
References
1. Miller KD, Siegel R, Lin CC, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66(4):271-289.
2. American Cancer Society. Cancer statistics, 2019. https://onlinelibrary.wiley.com/doi/full/10.3322/caac.21551. Published January 2019.
3. Halpern MT, Yabroff KR. Prevalence of outpatient cancer treatment in the United States: estimates from the Medical Panel Expenditures Survey (MEPS). Cancer Invest. 2008;26(6):647-651.
4. Radiation therapy to treat cancer. National Cancer Institute website. http://www.cancer.gov/about-cancer/treatment/types/radiation-therapy/radiation-fact-sheet. Updated July 19, 2017. Accessed January 31, 2018.
5. Leser M, Ledesma N, Bergerson S, Trujillo E. Oncology Nutrition for Clinical Practice. Chicago, IL: Oncology Nutrition Dietetic Practice Group; 2013.
6. Recommendations summary: ONC: nutrition status and outcomes in adult oncology patients 2013. Academy of Nutrition and Dietetics Evidence Analysis Library website. http://www.andeal.org/template.cfm?template=guide_summary&key=4155. Accessed January 31, 2018.
7. What is the relationship between nutrition status and radiation treatment tolerance in oncology patients? Academy of Nutrition and Dietetics Evidence Analysis Library website. https://www.andeal.org/topic.cfm?menu=5291&cat=4957. Accessed January 17, 2018.
8. Isenring E. Nutrition intervention improves nutritional status and quality of life outcomes in patients undergoing radiotherapy. In: Kataria T, ed. Frontiers in Radiation Oncology. InTechOpen; 2013:205-216.
9. ONC: executive summary of recommendations (2013). Academy of Nutrition and Dietetics Evidence Analysis Library website. http://www.andeal.org/topic.cfm?menu=5291&cat=5067. Accessed January 31, 2018.
10. ONC: nutrition assessment for adult oncology patients (2013). Academy of Nutrition and Dietetics Evidence Analysis Library website. https://adaevidencelibrary.com/topic.cfm?menu=5291&pcat=5068&cat=5164. Accessed January 23, 2018.
11. August DA, Huhmann MB; American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Board of Directors. A.S.P.E.N. clinical guidelines: nutrition support therapy during adult anticancer treatment and in hematopoietic cell transplantation. JPEN J Parenter Enteral Nutr. 2009;33(5):472-500.
12. Arends J, Baracos V, Bertz H, et al. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin Nutr. 2017;36(5):1187-1196.
13. Which malnutrition screening tools have been found to be valid and reliable for identifying malnutrition risk in adult oncology patients in ambulatory and acute care settings? Academy of Nutrition and Dietetics Evidence Analysis Library website. https://www.andeal.org/topic.cfm?cat=4873&conclusion_statement_id=251796. Accessed January 17, 2018.
14. Nutrition in cancer care (PDQ®)–health professional version. National Cancer Institute website. https://www.cancer.gov/about-cancer/treatment/side-effects/appetite-loss/nutrition-hp-pdq. Updated November 17, 2017. Accessed January 30, 2018.
15. Arribas L, Hurtós L, Sendrós MJ, et al. NUTRISCORE: a new nutritional screening tool for oncological outpatients. Nutrition. 2017;33:297-303.
16. Findlay M, Bauer J, Brown T; Head and Neck Guideline Steering Committee. Evidence-based practice guidelines for the nutritional management of adult patients with head and neck cancer. https://wiki.cancer.org.au/australia/COSA:Head_and_neck_cancer_nutrition_guidelines. Updated June 6, 2014. Accessed January 18, 2018.
17. Recommendations summary: ONC: nutrition diagnosis of malnutrition in adult oncology patients. Academy of Nutrition and Dietetics Evidence Analysis Library website. http://www.andeal.org/template.cfm?template=guide_summary&key=4179. Accessed January 31, 2018.
18. Fearon K, Strasser F, Anker SD, et. al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12(5):489-495.
19. Recommendations summary: ONC: nutrition assessment for the stages of cancer cachexia in adult oncology patients 2013. Academy of Nutrition and Dietetics Evidence Analysis Library website. https://www.andeal.org/template.cfm?template=guide_summary&key=4160. Accessed January 31, 2018.
20. Rock CL, Doyle C, Demark-Wahnefried W, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62(4):243-274.
21. Food, nutrition, physical activity and the prevention of cancer: a global perspective: the third expert report. World Cancer Research Fund website. https://www.wcrf.org/dietandcancer. Accessed January 31, 2018.
22. ASPEN Board of Directors and the Clinical Guidelines Task Force. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enteral Nutr. 2002;26(1 Suppl):1SA-138SA.
23. Institute of Medicine of the National Academies, Food and Nutrition Board. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. https://www.nap.edu/read/10490/chapter/1. Published 2005. Accessed January 18, 2018.
24. Are the measured energy needs of head and neck cancer patients receiving radiation therapy different from estimated needs? Academy of Nutrition and Dietetics Evidence Analysis Library website. https://www.andeal.org/topic.cfm?menu=5291&pcat=3198&cat=3237. Accessed January 31, 2018.
25. Are the measured energy needs of non-small cell lung cancer patients undergoing chemotherapy different from estimated needs? Academy of Nutrition and Dietetics Evidence Analysis Library website. https://www.andeal.org/topic.cfm?menu=5291&cat=3200. Accessed January 31, 2018.
26. Are the protein needs of cancer patients treated by pelvic radiation therapy different from the RDA? Academy of Nutrition and Dietetics Evidence Analysis Library website. https://www.andeal.org/topic.cfm?menu=5291&pcat=3073&cat=3115. Accessed January 31, 2018.
27. Are the protein needs of head and neck cancer patients undergoing radiation therapy different than the RDA? Academy of Nutrition and Dietetics Evidence Analysis Library website. https://www.andeal.org/topic.cfm?menu=5291&pcat=3198&cat=3237. Accessed January 31, 2018.
28. Is it safe to take antioxidant supplements during chemotherapy and radiation therapy? Oncology Nutrition Dietetic Practice Group website. https://www.oncologynutrition.org/erfc/eating-well-when-unwell/is-it-safe-to-take-antioxidant-supplements-during-chemotherapy-and-radiation-therapy/. Updated April 2013. Accessed January 31, 2018.
29. Is there a relationship between enteral nutrition to improve nutrition intake (protein and kcals) and the reduction of side effects associated with outpatient radiation therapy for head and neck cancer patients? Academy of Nutrition and Dietetics Evidence Analysis Library website. http://www.andeal.org/topic.cfm?cat=3237. Accessed January 31, 2018.
30. Lalla RV, Treister N, Sollecito T, et al. Oral complications at 6 months after radiation therapy for head and neck cancer. Oral Dis. 2017;23(8):1134-1143.
31. Berger AM, Mooney K, Alvarez-Perez A, et al. Cancer-related fatigue, version 2.2015. J Natl Compr Canc Netw. 2015;13(8):1012-1039.
32. Elliott L, Levin R, McIver J. The Complete Resource Kit for Oncology Nutrition. Chicago, IL: Academy of Nutrition and Dietetics; 2013.
33. van Waart H, Stuiver MM, van Harten WH, et al. Effect of low-intensity physical activity and moderate- to high-intensity physical exercise during adjuvant chemotherapy on physical fitness, fatigue, and chemotherapy completion rates: results of the PACES randomized clinical trial. J Clin Oncol. 2015;33(17):1918-1927.
34. Lalla RV, Saunders DP, Peterson DE. Chemotherapy or radiation-induced oral mucositis. Dent Clin North Am. 2014;58(2):341-349.
35. Mucositis. The Oral Cancer Foundation website. https://oralcancerfoundation.org/complications/mucositis/. Accessed January 17, 2018.
36. Is there a relationship between the intake of oral glutamine to improve and support recovery from radiation therapy and the reduction of mucositis associated with treatment of cancer patients? Academy of Nutrition and Dietetics Evidence Analysis Library website. https://www.andeal.org/topic.cfm?menu=5291&pcat=3577&cat=3616. Accessed January 31, 2018.
37. Bartels CL. Xerostomia. The Oral Cancer Foundation website. https://oralcancerfoundation.org/complications/xerostomia/. Accessed February 6, 2018.


