Today’s Dietitian
Vol. 17 No. 5 P. 38
Lactose intolerance isn’t a new malady, but it may be one of the most discussed. As any practicing dietitian knows, lactose intolerance affects a significant number of people, causing gas, bloating, cramps, nausea, and diarrhea within 30 minutes to two hours after eating lactose-containing products. Because dairy products are the primary source of lactose, eating a dairy-free diet may seem like the easiest way for your clients and patients to avoid symptoms, but it may not be the healthiest.
What Is Lactose Intolerance?
Milk sugar (lactose) is a disaccharide that must be broken down into the simple sugars glucose and galactose by the intestinal enzyme lactase in order to be absorbed in the intestinal tract. When the enzyme—which is active in the small intestine in those who can tolerate lactose—is lacking, lactose remains undigested. Few bacteria reside in the small intestine, but when the undigested lactose moves into the large intestine, the millions of bacteria that call the large intestine home ferment it. The bacteria give off hydrogen and methane gases and symptoms result.
The condition, referred to as lactose intolerance or “lactase nonpersistence” is quite common among many populations. Estimates vary, but generally it’s believed that as much as 80% of the black population is affected, 53% of the Mexican-American population, and about 15% of the white population. In Europe, it varies widely from about 2% in Scandinavia to about 70% in Sicily.1 The prevalence is almost 100% in some Asian countries.1 Most people are born with the ability to digest lactose, but for many, that ability lessens significantly after about age 2. It’s possible, however, to experience some degree of lactose malabsorption without ever experiencing symptoms of lactose intolerance.1
There are four types of lactase deficiency that can result in lactose intolerance:2
- Primary lactase deficiency is the most common type of lactase deficiency, in which lactase production declines over time, beginning at about age 2. However, symptoms may not begin until adolescence or adulthood. In some people, it may be hereditary.
- Secondary lactase deficiency is the result of infection or disease in the small intestine. This is most common in infants and young children, when lactase is temporarily lost as a result of a rotavirus infection, which causes severe watery diarrhea, often with vomiting, fever, and abdominal pain, or due to childhood diarrhea caused by E coli. A lactose-free diet is best prescribed during recovery,3 but treating the underlying condition usually improves the lactose intolerance.
- Developmental lactase deficiency may occur in infants born prematurely, but it usually lasts for only a short period of time after birth.
- Congenital lactase deficiency is a rare hereditary disorder in which the small intestine produces no lactase enzyme from birth.
Reliable Diagnosis
Lactose intolerance often is diagnosed on the basis of symptoms and an elimination test in which dairy foods are avoided, then reintroduced, and symptoms monitored.1 However, this is not the most reliable way to detect and diagnose the condition. It’s common for people to misdiagnose themselves after consuming milk or some other dairy food and then experiencing symptoms. “Many people have digestive discomfort after eating and then assume it’s related to lactose intolerance,” says Sonya Angelone, MS, RDN, CLT, spokesperson for the Academy of Nutrition and Dietetics (the Academy). It can be more definitively diagnosed after consuming a specified amount of lactose and having the breath analyzed for hydrogen and methane gases, both of which are byproducts of bacteria digesting the lactose. The gases are diffused into the blood then expired through the lungs. A recent review found, however, that even breath testing can produce inaccurate results, with an estimated 5% to 15% false negatives found with hydrogen breath testing—that is, reporting no lactose intolerance when, in fact, it exists.4 According to the report, about 80% of methane is excreted by flatus and about 20% in the breath. Elevated levels of either hydrogen or methane suggest lactose intolerance.
Because of cost issues associated with testing, Angelone says she suggests people try to cut back and gradually reintroduce dairy foods in small amounts to determine if it helps relieve symptoms. If it doesn’t, then she recommends they see their physicians. Angela Lemond, RDN, CSP, LD, a dietitian in private practice in the Dallas area, echoes that sentiment. “Breath analysis tests are expensive and depending on where someone lives, it may be difficult to find a physician who will do a breath analysis.”
Misconceptions About Lactose Intolerance
“One of the most common misconceptions about lactose intolerance,” Angelone says, “is that people with the condition are unable to consume any dairy products without experiencing symptoms. The other common misconception is that lactose intolerance is the same thing as a milk allergy.” However, an important distinction exists between lactose intolerance and a milk allergy. While lactose intolerance results from undigested milk sugars, a milk allergy is an immune reaction to milk proteins. For those suffering from a milk allergy, all food containing milk and milk products must be eliminated from the diet.
Lactose Threshold
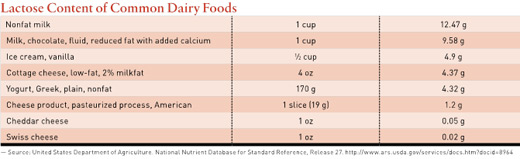
In the past, doctors diagnosed lactose intolerance by having individuals ingest a large amount of lactose (the amount in about one quart of milk) before undergoing testing, resulting in overdiagnosis. However, lactose loads of less than 6 g, equivalent to a one-half serving of milk, are unlikely to trigger symptoms, even among intolerant individuals.5 Even 12 g of lactose generally is considered to be well tolerated.6 However, according to Vandana Sheth, RDN, CDE, a dietitian in private practice in the Los Angeles area and a spokesperson for the Academy, “The threshold for lactose intolerance and symptoms varies widely among individuals.”
Consequences of Lactose Intolerance
The majority of blacks and Hispanic Americans suffer from lactose intolerance and consume less than the recommended level of three servings of low-fat and fat-free dairy foods per day.6,7 In fact, lactose intolerance is cited by black adults as the primary reason for cutting back or avoiding dairy foods.7 The main health consequence of lactose intolerance is a reduction in calcium intake.5 Dairy products, such as low-fat milk, provide calcium, as well as several other important nutrients, including high-quality protein, both essential for building and maintaining bone health.5
According to a recent study, a calcium-equivalent serving of cow’s milk requires 1.1 servings of fortified soy beverage; 0.6 servings of fortified orange juice; 1.2 servings of boney fish, such as sardines; or 2.2 servings of leafy greens. However, the intake of other nutrients found in dairy foods, such as potassium, riboflavin, and vitamin B12 are unlikely to be replaced equally.8 Milk and some yogurts are fortified with vitamin D, another nutrient in short supply in the diet and one that has few food sources. If adults avoid dairy foods, it’s important they achieve calcium intake levels of 1,000 mg to 1,300 mg per day through diet and supplementation, and meet vitamin D requirements of 600 IU to 800 IU through supplementation.
“Since dairy is such an important source of essential nutrients, like calcium and vitamin D, it’s important to continue reintroducing dairy products as long as they are tolerated,” Lemond says. She advises eating low-lactose products, spaced throughout the day, and combining them with other foods.
Lactose intolerance also may affect absorption of some medications, such as levothyroxine for the treatment of hypothyroidism,9 so it’s important to know what medications a patient or client is taking and whether absorption and effectiveness are being affected.
Lactose-Free Options
Several lactose-free dairy products are available that may make it easy for people to meet their calcium and various other nutrient needs; these include Lactaid, Horizon Organic, and Dairy Ease lactose-free milks, in which the lactose is “predigested” (hydrolyzed). Lactaid also makes lactose-free ice cream, yogurt, cottage cheese, and eggnog, and Yoplait makes a lactose-free yogurt. These products typically contain between 0 g to 2 g of lactose per serving, well under the typical threshold for symptoms. Some products also claim to be lactose-free, when they’re virtually lactose-free to begin with, such as lactose-free cream cheese (regular cream cheese contains less than 1 g of lactose per oz).
Also available are lactase enzyme tablets, such as Lactaid, Lactodigest, Source Naturals, Nature’s Way, and Walgreens brand, designed to help digest the lactose in dairy once it’s consumed. However, the National Institutes of Health concluded in 2010 that there’s a lack of evidence suggesting that these products reduce symptoms.
Gradually introducing small amounts of milk or milk products may help some people adapt with fewer symptoms. Hard cheeses, such as cheddar or Swiss, may be better tolerated than a glass of milk. A 1.5 oz serving of low-fat hard cheese has less than 1 g of lactose, while a 1-cup serving of low-fat milk has about 11 g to 13 g of lactose.2 However, people with lactose intolerance also may tolerate yogurt better than milk, even though yogurt and milk have similar amounts of lactose.2 Yogurt made from milk contains lactose, but it also contains bacteria that digest much of the lactose, making it less likely to cause symptoms. Soy yogurt is made with soy rather than milk, so it’s naturally lactose-free. Chocolate milk also may be better tolerated than unflavored milk. According to Lemond, who suffers from lactose intolerance, “Eating a slice of cheddar cheese might be tolerable, but consuming a cheese pizza, with several ounces of mozzarella, could cause symptoms. Everyone is different, so the form and the amount of food that’s tolerable can vary among individuals.”
People who find they have symptoms after consuming only small amounts of lactose should scout food labels for ingredients such as milk, lactose, whey, curds, milk by-products, dry milk solids, or nonfat dry milk powder, and avoid those products. These ingredients can be found in everything from bread and waffles to salad dressings and processed meats.2 Some common medications also use lactose as a filler. Check with a pharmacist or the pharmaceutical manufacturer on whether your clients’ medications contain lactose and how much.
Raw Milk or Goat’s Milk Solutions
Both raw milk and goat’s milk have been touted as being better tolerated than pasteurized cow’s milk. However, neither offers a symptom-free alternative for people with lactose intolerance. A recent study published in the Annals of Family Medicine disproved the idea that raw milk is less likely to trigger symptoms.10 In this small study, conducted at the Stanford Prevention Research Center, 16 lactose-intolerant participants were given three types of milk—raw, pasteurized, and soy—over multiple eight-day periods. Their breath was measured for hydrogen, and they reported their symptoms. The researchers found no difference in the hydrogen breath test or the severity of symptoms reported when the different types of milk were consumed. While goat’s milk has slightly less lactose than cow’s milk, it still can cause discomfort in people with low lactose thresholds.
The National Dairy Council offers the following simple tips for dealing with lactose intolerance:
- try it: opt for lactose-free products;
- sip it: introduce dairy slowly;
- stir it: mix milk with food;
- slice it: choose natural cheeses;
- shred it: add hard, natural cheeses to salads, pastas, and veggies; and
- spoon it: try easy-to-digest yogurt.
Recommendations
Lactose intolerance is a common, but benign, condition that can cause incredibly distressing gastrointestinal symptoms. While the condition itself is benign, the potential nutrition consequences are not. Self-diagnosis and elimination of all dairy can lead to nutrient shortfalls, such as lack of both calcium and vitamin D. It’s important to educate clients and patients on how best to determine if the symptoms they are experiencing are indeed the result of lactose intolerance. If they are a manifestation of lactose intolerance, dietitians can suggest they consume low-lactose or lactose-free dairy options, and/or counsel them on how to introduce small amounts of nutrient-rich dairy into their diets, while keeping symptoms at bay.
— Densie Webb, PhD, RD, is a freelance writer, editor, and industry consultant based in Austin, Texas.
References
1. Lember M. Hypolactasia: a common enzyme deficiency leading to lactose malabsorption and intolerance. Pol Arch Med Wewn. 2012;122(Suppl 1):60–64.
2. Lactose intolerance. National Institute of Diabetes and Digestive and Kidney Diseases website. www.niddk.nih.gov/health-information/health-topics/digestive-diseases/lactose-intolerance/pages/facts.aspx. Updated June 4, 2014. Accessed March 2, 2015.
3. Brüssow H. Nutrition, population growth and disease: a short history of lactose. Environ Microbiol. 2013;15(8):2154-2161.
4. de Lacy Costello BP, Ledochowski M, Ratcliffe NM. The importance of methane breath testing: a review. J Breath Res. 2013;7(2):024001.
5. Heaney RP. Dairy intake, dietary adequacy, and lactose intolerance. Adv Nutr. 2013;4(2):151-156.
6. Suchy FJ, Brannon PM, Carpenter TO, et al. National Institutes of Health Consensus Development Conference: lactose intolerance and health. Ann Intern Med. 2010;152(12):792-796.
7. Keith JN, Nicholls J, Reed A, Kafer K, Miller GD. The prevalence of self-reported lactose intolerance and the consumption of dairy foods among African American adults are less than expected. J Natl Med Assoc. 2011;103(1):36-45.
8. Fulgoni VL 3rd, Keast DR, Auestad N, Quann EE. Nutrients from dairy foods are difficult to replace in diets of Americans: food pattern modeling and an analyses of the National Health and Nutrition Examination Survey 2003-2006. Nutr Res. 2011;31(10):759-765.
9. Ruchala M, Szczepanek-Parulska E, Zybek A. The influence of lactose intolerance and other gastro-intestinal tract disorders on L-thyroxine absorption. Endokrynol Pol. 2012;63(4):318-323.
10. Mummah S, Oelrich B, Hope J, Vu Q, Gardner CD. Effect of raw milk on lactose intolerance: a randomized controlled pilot study. Ann Fam Med. 2014;12(2):134-141.


