Today’s Dietitian
Vol. 22, No. 4, P. 44
Suggested CDR Learning Codes: 3060, 4040, 5110, 5330
Suggested CDR Performance Indicators: 8.1.5, 8.3.6, 8.4.4, 10.2.1
CPE Level 2
Take this course and earn 2 CEUs on our Continuing Education Learning Library
Food allergies and asthma are both on the rise in the United States. Multiple health surveys from 1997 to 2007 concluded that there’s an increased prevalence of food allergies in children and heightened food allergy awareness by parents and health care professionals.1 Research has examined the relationship between food allergies and asthma to determine whether the former represent predisposition for the latter, and whether there’s a cause-and-effect relationship between them.
This continuing education course identifies the relationship between food allergies and asthma and provides counseling strategies dietitians can use when working with patients.
Asthma
The National Asthma Education and Prevention Program defines asthma as a chronic inflammatory disorder of the airways. In those with asthma, airway inflammation leads to coughing, wheezing, chest tightness, and loss of breath that can be reversed with treatment.2 According to a 2011 report from the Centers for Disease Control and Prevention (CDC), asthma affects 1 in 12, or about 25 million, people.3 The CDC states that women are more likely than men, and boys more likely than girls, to have asthma. The CDC also reports that multiracial adults and black adults and children are more likely than whites to have asthma. Other risk factors for asthma include being obese and smoking.4
There’s no gold standard tool used to diagnose asthma.5 The National Asthma Education and Prevention Program recommends doctors diagnose asthma by reviewing reported medical history and performing a physical examination that includes spirometry to determine whether there are recurrent episodes of airway obstruction. The physical exam will look for key symptoms indicating airway obstruction and a possible asthma diagnosis. These key symptoms include a history of a cough, recurrent wheezing, recurrent difficulty breathing, and recurrent chest tightness. These symptoms often occur or worsen due to outside stressors such as nighttime, exercise, infection, or inhalation of allergens or irritants. Doctors are encouraged to determine whether there are causes of airway obstruction other than asthma.2
Food Allergies
Food allergies are an abnormal immune response to the protein in certain foods. While it’s possible for any food to cause an allergic reaction, the most common food allergens are milk, wheat, peanuts, tree nuts, eggs, soy, fish, and shellfish. Food allergies can be mild or life threatening, and signs and symptoms include hives, eczema, congestion, vomiting, diarrhea, coughing, shortness of breath, wheezing, loss of consciousness, and a weak pulse.
According to Food Allergy Research & Education (FARE), 1 in 13 children has a food allergy, and food allergies affect as many as 15 million Americans.6 Risk factors for food allergies include family history or previous history of other allergy reactions such as asthma, hay fever, or eczema.6 If a child has a history of asthma, hay fever, or eczema, parents should be aware that the child is at risk of other allergic diseases such as food allergies. Because food allergies are dangerous, it’s important that families are aware of their children’s risk levels.
Food allergies are diagnosed through the use of skin prick testing, immunoglobulin E (IgE) blood tests, and oral food challenges. Clinical history showing signs and symptoms of an allergy are necessary along with skin prick tests and IgE blood tests for diagnosis. Oral food challenges are performed by the medical provider and most often by an allergist. The medical provider will feed measured amounts of the allergen to the patient and then watch them for any reactions. If there are no reactions, the measured doses provided are increased and the medical provider continues to watch the patient for any signs and symptoms. If no symptoms of the suspected food allergy are present at the end of the oral food challenge, the food allergy is ruled out.
The gold standard for the diagnosis of food allergies, however, is a double-blinded, placebo-controlled oral food challenge. In a double-blinded, placebo-controlled food challenge, the patient is given increasing doses of the suspected allergen and a placebo. The allergen and placebo are given at separate times, and neither the patient nor the medical provider are aware of which the patient is receiving. The patient is then watched to see whether symptoms develop. The double-blinded placebo controlled oral food challenge is done to avoid any bias.7 Some physicians choose not to perform oral food challenges due to the expense, time commitment, and potential for severe reactions.8
Anaphylaxis
It’s important to note that food allergies don’t usually present with chronic respiratory symptoms. Multiple studies have shown that concurrent diagnoses of food allergies and asthma lead to an increased risk of anaphylaxis.5 A 2010 study by Krogulska and colleagues showed that anaphylaxis risk was higher in those with both food allergies and asthma. It hypothesized that bronchial hyperreactivity is the link between food allergies and asthma and was found in 47% of nonasthmatic children with food allergies and 100% of children with both asthma and food allergies. Only 36% of the children with food allergies and asthma showed respiratory symptoms following oral food challenges, suggesting that although there’s an increase in bronchial hyperreactivity following ingestion of food allergens, those with asthma and food allergies may not experience a respiratory reaction.9
A 2016 study examined how food allergies affected respiratory symptoms and bronchial hyperreactivity in children with asthma. Participants were identified using double-blinded, placebo-controlled food challenges and had diagnosed asthma and food allergies. The findings were similar to those of the 2010 study, showing an increase in bronchial hyperreactivity in those with asthma and food allergies, even in those without respiratory symptoms. The study also showed that asthma control was improved following an eight-week elimination of allergens in 54.5% of children.10 These studies demonstrate that, although food allergies may not trigger asthma, there’s still an association between the two, and food allergies can trigger asthma exacerbations in those with existing asthma.
Food Sensitivities
Food sensitivities or intolerances (other than celiac disease) don’t involve the immune system. They take place in the digestive system and aren’t life threatening. People often confuse food intolerances with food allergies, which may result in an inaccurate diagnosis. This results from inaccurate self-diagnosis, and diagnosis from health care providers who don’t specialize in allergies. Many people will diagnose themselves with food allergies when they actually have food sensitivities or intolerances. This can cause them to excessively restrict their diets; as a result, they’re vulnerable to nutrient deficiencies.11,12
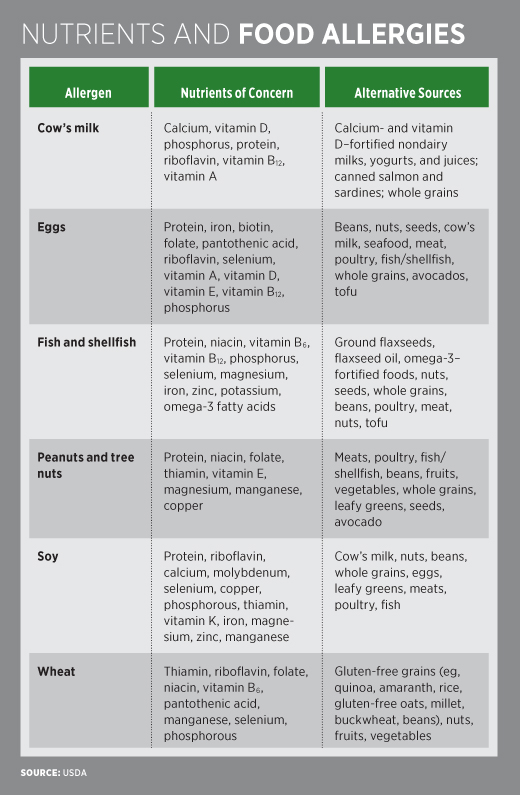
The accompanying table shows nutrients of concern in individuals who are avoiding each of the eight most common allergens. In addition to the deficiencies listed in the table, patients who eliminate multiple allergens without proper diet planning to replace these nutrients found in the allergenic foods put themselves at risk of macronutrient deficiencies including protein and fat. A patient who eliminates milk and all milk products from the diet without having a true allergy diagnosis may be at risk of calcium and vitamin D deficiencies if they don’t supplement their diet with other sources of calcium and vitamin D. Such a patient may be lactose intolerant and not milk allergic, and so may be able to consume some yogurts and cheeses to meet calcium and vitamin D needs. A 2013 article discusses a case review in which 11 children were diagnosed with failure to thrive due to parent-diagnosed food allergies. When these children were tested for the potential food allergens using double-blinded, placebo-controlled food challenges, only two reacted. This shows that these children likely were failing to thrive because their parents restricted their diets to eliminate perceived food allergens and not true food allergens.13 Some symptoms of food intolerances include bloating, gas, abdominal pain, and diarrhea.14 According to FARE, new research suggests that an increased number of adults in the United States are self-reporting food allergies without being diagnosed by a doctor.11 This is dangerous because without a proper medical diagnosis, adults who self-diagnose their food allergies won’t know how to handle true allergic reactions such as anaphylaxis. These adults also are at risk of nutrition deficiencies due to dietary restrictions. Consequently, research on the link between asthma and food allergies that relies on self-reported food allergies may be skewed.1
Food Sensitization as a Predictor for Asthma
Food sensitization describes the existence of evidence of an allergen-specific IgE to a food in the absence of symptoms when one is exposed to the food.15 For example, if someone is sensitized to a food, an IgE blood test or skin prick test will show positive results, but eating the food won’t necessarily lead to clinical symptoms. Food sensitization early in life has been shown to increase the risk of asthma later in life. A 2011 article in the Journal of the American Dietetic Association states that a positive skin test for allergies and increased IgE raises the risk of developing asthma in children aged 3 to 14.16 Another study found that high IgE levels at 6 months of age leads to early-onset asthma and the development of asthma in the school-age years.17 A review study looking at data from two cohorts showed that when infants were sensitized to common food allergens by age 2, they had an increased risk of asthma and allergic rhinitis later in life. The two cohorts reviewed in the study were the Australian-based Melbourne Atopy Cohort study (MACS) cohort and the German-based LISAplus cohort. The MACS cohort used skin prick testing for egg whites, cow’s milk, and peanut. The LISAplus cohort used IgE blood samples that tested a mix of hen’s egg, cow’s milk, peanut, wheat flour, soybean, and codfish. If the IgE level was high, egg whites, cow’s milk, and peanut were then tested on their own. This study also showed that sensitization to both food and aeroallergens (eg, inhalant allergens such as cat dander, mold, and pollen) early in life was a stronger predictor of asthma and allergic rhinitis later in life than was food sensitization alone.18
Sensitization to foods is more common in asthmatics than in the general population.19 A 2015 Polish study showed that more than one-half of the children with asthma studied had food-related complaints including respiratory symptoms, skin lesions, and gastrointestinal symptoms. Of these children, approximately 20% were sensitized to food allergens and 6.6% had confirmed food allergies. These statistics show that being sensitized to food without having a confirmed food allergy is associated with having asthma.20
Multiple Food Allergies as a Risk Factor for Asthma
Food allergies, eczema, allergic rhinitis, and asthma all are considered allergic diseases and often coexist. As mentioned, research has explored the relationship between food allergies and asthma to determine whether food allergies predispose individuals to asthma. Studies have concluded that multiple food allergies have a strong association with the diagnosis of asthma, but it’s unclear whether there’s a cause-and-effect relationship between them. Studies continue to explore whether there’s merely an association or a cause-and-effect relationship.
It’s possible that the interrelationship between food allergies and asthma differs among age groups. Young children with food allergies might outgrow their food allergies before they develop asthma symptoms. This is important to consider when reviewing research because studies can be affected when young children outgrow their food allergies before developing asthma symptoms. Young children also may have transient wheezing rather than true asthma. According to the National Asthma Council Australia, wheezing is common in the first few years of life and children usually outgrow transient wheezing by age 3.21
A study by Schroeder and colleagues accounted for the impact of age on the interrelationship between food allergies and asthma. This study looked at children aged 6 and older and those younger than 6. The researchers concluded that food allergies are associated with a higher risk of asthma, and those with multiple food allergies are at a greater likelihood of an asthma diagnosis.22 A stronger association between food allergies and asthma was shown in the older children, but there was also an association in the younger children studied. Both the older and younger children with food allergies and asthma were diagnosed with asthma at a younger age than were those who didn’t have food allergies. Egg, milk, peanut, and tree nut allergies all were associated with an increased risk of asthma, and food allergies developed before asthma across all age groups. Researchers also observed an association between severe food allergies and asthma. This study concluded that having severe food allergies with symptoms such as anaphylaxis to at least one food led to an increased risk of asthma in both older and younger children. However, a cause-and-effect relationship between food allergies and asthma couldn’t be determined.
A 2011 study looked at a cohort of 799 children with physician-diagnosed food allergies and found an association between multiple food allergies and asthma. This study relied on skin prick tests, IgE tests, and parental reports, rather than oral food challenges, to diagnose food allergy. The parents in this study were given questionnaires about their child’s food allergy history. Foods on the questionnaire included eggs, dairy/milk products, seafood, tree nuts, peanuts/peanut butter, and sesame seeds. Response options for the questionnaire included “yes,” “no,” and “never tried.” Food allergies in this study were defined as report of the allergy and evidence by skin prick and IgE tests, conducted for the same foods discussed in the questionnaire. Children who had never tried these foods were excluded from the study. The prevalence of asthma in children with food allergies in the cohort was 45.6%, and allergies to eggs and tree nuts were more strongly associated with asthma than were other food allergens.23
A cohort study that looked at the medical records of children with diagnoses of asthma, rhinitis, and food allergies by health care professionals concluded that those with a food allergy had a higher risk of developing asthma and rhinitis. Participants with multiple food allergies were at an increased risk of asthma and rhinitis than were those with just one food allergy; those with milk, peanut, and egg allergies were shown to be at an increased risk of asthma development compared with individuals who didn’t have these particular allergies.24
Do Food Allergies Trigger Asthma Symptoms?
Asthma symptoms are shown to be worse in those with food allergies, and research has explored whether food allergies trigger asthma symptoms.19 It’s unknown whether asthma symptoms directly correlate with ingestion of food allergens, but studies suggest an association between food allergies and asthma exacerbations.5 While food sensitization also may worsen asthma, this exacerbation may occur because severe asthma is associated with greater atopy,25 ie, “the genetic tendency to develop allergic diseases such as rhinitis, asthma, and atopic dermatitis.”26 Therefore, someone diagnosed with asthma has a greater risk of also having a food allergy diagnosis because food allergies are another allergic disease. Those with both food allergies and asthma are at an increased risk of severe asthma reactions, so it’s important for patients to obtain a proper diagnosis of and appropriate treatment for food allergies and asthma.
Food Diversity in the First Year of Life
Research has shown that food diversity introduced in the first year of life has a protective effect against allergic diseases including asthma and food allergies. While in the past parents were told to wait until their children were 1 year old to introduce the top eight food allergens, it’s now recommended that these foods are introduced between 4 and 6 months of age along with other foods and formula and/or breast milk. The American Academy of Allergy, Asthma and Immunology recommends waiting three to five days between new foods and introducing allergens one at a time after babies accept and tolerate other single-ingredient foods.27 Research on early introduction of food allergens has shown a decreased incidence in food allergies.
Important research pertaining to food diversity in the first year of life was done in the Learning Early About Peanut Allergy (LEAP) study, which explored whether avoidance or consumption of peanuts during infancy led to peanut allergies. This study looked at 640 infants between the ages of 4 and 11 months who were at high risk of developing food allergies due to a diagnosis of severe eczema and/or an egg allergy. Infants were given skin prick tests for peanut allergy and assigned to two cohorts based on whether their skin tests were positive. Cohort participants were then randomly assigned to a group in which peanuts were consumed or a group in which they were avoided until 60 months (5 years) of age. Of the 542 infants with negative skin prick tests, 13.7% of the infants who avoided peanuts were allergic to peanuts at 60 months, and only 1.9% of the infants who consumed peanuts were allergic to peanuts at 60 months. Of the 98 infants in the group whose skin tested positive to peanuts, 35.3% of those who avoided peanuts had peanut allergies at 60 months, while only 10.6% of those who consumed peanuts did. In sum, those at high risk of peanut allergies who consumed peanuts during infancy were less likely to develop peanut allergies as toddlers and preschool-age children.28
In the Enquiring About Tolerance (EAT) study, 1,303 3-month-old exclusively breast-fed infants in the United Kingdom were randomly assigned to two groups. One was introduced early to peanuts, cooked egg, cow’s milk, sesame, whitefish, and wheat, and the other was exclusively breast-fed until 6 months of age and then introduced to foods at the discretion of parents. Unlike the LEAP study, EAT looked at the general population rather than those at high risk. While this study didn’t conclude that early introduction of allergenic foods prevents food allergies, it did show that early introduction of potential allergens at specific doses for a specific time frame could protect against the development of food allergies.29
More research is needed regarding the early introduction of allergens, however, these studies both show that early introduction to allergens doesn’t increase risk of developing food allergies and is more beneficial than it is harmful. It’s important for dietitians to be knowledgeable about this new research and educate patients about food diversity whenever possible.30 Current recommendations also state that women shouldn’t avoid potential allergens during pregnancy.
Food Allergies and Asthma in Adults
The majority of the studies on the association between asthma and food allergies have been done in children. One small study used a cohort of 203 adults, primarily Hispanic and black women with diagnosed asthma. It looked at the symptoms of self-reported food allergies in adults and found that those with asthma and self-reported food allergies had an increased risk of hospitalization, emergency department visits, and oral steroid use due to asthma exacerbations.31 This study further suggests that there might be an association between food allergies and asthma in the adult population. However, due to its small sample size and demographic, more research is needed.
Role of Dietitians and Allergists
Not enough evidence is available to show a causal relationship between food allergies and asthma or determine whether food allergies can directly affect asthma control.19 However, research has shown an association between the two conditions and that a diagnosis of both food allergies and asthma can lead to worse food-induced allergic reactions and increase risk of anaphylaxis in children.16
Despite the lack of conclusive evidence, there are ways dietitians and allergists can work together to help patients with food allergies. Allergists are responsible for diagnosing food allergies and asthma and providing medication and education about the medications used to treat asthma. Dietitians should review patients’ histories and refer those whom they suspect to have food allergies to allergists for diagnosis. Dietitians should counsel patients about food allergies and help them understand which foods to include in their diets and which to exclude. Avoidance of the allergen is the only way to prevent an allergic reaction, and dietitians are skilled in teaching patients what to look for on Nutrition Facts labels and how to avoid allergens at school, restaurants, and when cooking at home. After taking a diet history from patients and/or their parents, dietitians should identify any nutrient gaps in the diet that result from avoiding food allergens and recommend alternative foods to fill these gaps to avoid nutrition deficiencies (refer to table).
Dietitians should be aware that, if a patient has an asthma diagnosis, they might have food allergies, too. Using nutrition interventions, dietitians can help these patients prevent exacerbations. It’s necessary for dietitians to frequently follow up with their patients to ensure they understand how to avoid allergens and choose alternative foods, as well as to evaluate their patient’s diet to ensure they’re continuing to meet their estimated nutrition needs while avoiding allergens. Without the guidance of a dietitian, patients often overrestrict their diets, which may result in nutrition deficiencies and decreased quality of life. Education of both patients and caregivers about allergen avoidance is important for reducing fear and anxiety. Caregivers also should make sure patients’ schools are aware of their food allergies and know how to handle an emergency.8
— Linzy Ziegelbaum, MS, RD, CDN, is a New York–based dietitian in private practice specializing in food allergies, weight management, and sports nutrition for children and teens.
Learning Objectives
After completing this continuing education course, nutrition professionals should be better able to:
1. Distinguish the relationship between food allergies and asthma.
2. Discuss with clients how to manage food allergies with diet.
3. Assess the prevalence of asthma in patients with food allergies.
4. Explain how food diversity in the first year of life influences allergic diseases.
CPE Monthly Examination
1. What is the gold standard for food allergy diagnosis?
a. Immunoglobulin E (IgE) blood test
b. Skin prick test
c. Double-blinded, placebo-controlled oral food challenge
d. 24-hour dietary recall
2. According to the Centers for Disease Control and Prevention, how many people does asthma affect each year?
a. 1,200
b. 25,000
c. 12,000,000
d. 25,000,000
3. What happens if someone is sensitized to a food allergen?
a. Skin prick and IgE tests will be positive, but the patient won’t show signs or symptoms upon eating the food.
b. Skin prick and IgE tests will be positive, and the patient will have an allergic reaction when they eat the food.
c. Skin prick and IgE tests will be negative, but the patient will have an allergic reaction when they eat the food.
d. The patient will show signs and symptoms similar to food intolerances upon eating the food.
4. What were the findings of a 2010 study by Krogulska and colleagues that examined the relationship between asthma and food allergies and anaphylaxis?
a. Those with a diagnosis of both asthma and food allergies are at an increased risk of anaphylaxis.
b. Those with just one food allergy are at an increased risk of anaphylaxis.
c. Those with a diagnosis of both eczema and food allergies are at an increased risk of anaphylaxis.
d. Those with a diagnosis of both asthma and food allergies are more likely to outgrow their diagnoses.
5. Research has shown that food diversity introduced within the first year of life will result in which of the following?
a. An increased risk of asthma
b. An increased risk of food allergies
c. A protective effect on allergic diseases including asthma and food allergies
d. No effect on allergic diseases including asthma and food allergies
6. Why is self-diagnosing food allergies a problem?
a. It can lead to additional food allergies.
b. It can lead to nutrient deficiencies.
c. It can increase risk of asthma.
d. It can lead to additional food sensitivities.
7. The American Academy of Allergy, Asthma & Immunology defines atopy as which of the following?
a. An increased risk of the development of food allergies
b. The predisposition to develop asthma and atopic dermatitis
c. The genetic tendency to develop allergic diseases such as rhinitis, asthma, and atopic dermatitis
d. The genetic tendency to develop food allergies
8. How can dietitians help patients with food allergies?
a. By providing them with meal plans
b. By teaching them how to follow an elimination diet to diagnose food allergies
c. By diagnosing food sensitivities
d. By showing them how to avoid overrestricting their diet to prevent deficiencies and decreased quality of life
9. According to Food Allergy Research & Education, what proportion of children has a food allergy?
a. 1 in 5
b. 1 in 11
c. 1 in 13
d. 1 in 33
10. When should potential food allergens be introduced to infants?
a. Any time during the first year of life
b. Before 4 months of age
c. Between 4 to 6 months of age
d. After 1 year of age
References
1. Branum AM, Lukacs SL. Food allergy among children in the United States. Pediatrics. 2009;124(6):1549-1555.
2. National Institutes of Health; National Heart Lung and Blood Institute. National Asthma Education and Prevention Program expert panel number 3: guidelines for the diagnosis and management of asthma. https://www.nhlbi.nih.gov/files/docs/guidelines/asthsumm.pdf. Published October 2007. Accessed April 2, 2018.
3. Vital signs: asthma in the US. Centers for Disease Control and Prevention website. https://www.cdc.gov/vitalsigns/asthma/index.html. Updated May 3, 2011. Accessed April 2, 2018.
4. Centers for Disease Control and Prevention, National Center for Environmental Health, Division of Environmental Hazards and Health Effects. Asthma’s impact on the nation: data from the CDC National Asthma Control Program. https://www.cdc.gov/asthma/impacts_nation/asthmafactsheet.pdf. Accessed April 2, 2018.
5. Wang J, Liu AH. Food allergies and asthma. Curr Opin Allergy Clin Immunol. 2011;11(3):249-254.
6. What is a food allergy? Food Allergy Research & Education website. https://www.foodallergy.org/life-with-food-allergies/food-allergy-101/what-is-a-food-allergy. Accessed April 2, 2018.
7. Oral food challenge. Food Allergy Research & Education website. https://www.foodallergy.org/life-with-food-allergies/food-allergy-101/diagnosis-testing/oral-food-challenge. Accessed April 2, 2018.
8. Collins SC. Practice paper of the Academy of Nutrition and Dietetics: role of the registered dietitian nutritionist in the diagnosis and management of food allergies. J Am Nutr Diet. 2016;116(10):1621-1631.
9. Krogulska A, Dynowski J, Wasowska-Królikowska K. Bronchial reactivity in schoolchildren allergic to food. Ann Allergy Asthma Immunol. 2010;105(1):31-38.
10. Krogulska A, Dynowski J, Jedrzejczyk M, Sardecka I, Małachowska B, Wasowska-Królikowska K. The impact of food allergens on airway responsiveness in schoolchildren with asthma: a DBPCFC study. Pediatr Pulmonol. 2016;51(8):787-795.
11. FDA finds more and more adults are self-diagnosing food allergies. Food Allergy Research & Education website. https://www.foodallergy.org/about-fare/blog/fda-finds-more-and-more-adults-are-self-diagnosing-food-allergies. Published February 29, 2016. Accessed February 21, 2019.
12. Diagnosis & testing. Food Allergy Research & Education website. https://www.foodallergy.org/life-with-food-allergies/food-allergy-101/diagnosis-testing. Accessed February 21, 2019.
13. Mehta H, Groetch M, Wang J. Growth and nutritional concerns in children with food allergy. Curr Opin Allergy Clin Immunol. 2013;13(3):275-279.
14. Food intolerance definition. American Academy of Allergy, Asthma & Immunology website. https://www.aaaai.org/conditions-and-treatments/conditions-dictionary/food-intolerance. Accessed April 2, 2018.
15. Liu AH, Jaramillo R, Sicherer SH, et al. National prevalence and risk factors for food allergy and relationship to asthma: results from the National Health and Nutrition Examination Survey 2005-2006. J Allergy Clin Immunol. 2010;126(4):798-806.e13.
16. McCloud E, Papoutsakis C. A medical nutrition therapy primer for childhood asthma: current and emerging perspectives. J Am Diet Assoc. 2011;111(7):1052-1064.
17. Foong RX, du Toit G, Fox AT. Asthma, food allergy, and how they relate to each other. Front Pediatr. 2017;5:89.
18. Alduraywish SA, Standi M, Lodge CJ, et al. Is there a march from early food sensitization to later childhood allergic airway disease? Results from two prospective birth cohort studies. Pediatr Allergy Immunol. 2017;28(1):30-37.
19. Caffarelli C, Garrubba M, Gerco C, Mastrorilli C, Povesi Dascola C. Asthma and food allergy in children: is there a connection or interaction? Front Pediatr. 2016;4:34.
20. Krogulska A, Dynowski J, Funkowicz M, Małachowska B, Wąsowska-Królikowska K. Prevalence and clinical impact of IgE-mediated food allergy in school children with asthma: a double-blind placebo-controlled study. Allergy Asthma Immunol Res. 2015;7(6):547-556.
21. Resources — patients & carers. National Asthma Council Australia website. https://www.nationalasthma.org.au/living-with-asthma/resources/patients-carers. Updated October 2017.
22. Schroeder A, Kumar R, Pongracic JA, et al. Food allergy is associated with an increased risk of asthma. Clin Exp Allergy. 2009;39(2):261-270.
23. Gaffin JM, Sheehan WJ, Morrill J, et al. Tree nut allergy, egg allergy, and asthma in children. Clin Pediatr (Phila). 2011;50(2):133-139.
24. Hill DA, Grundmeier RW, Ram G, Spergel JM. The epidemiologic characteristics of healthcare provider-diagnosed asthma, allergic rhinitis, and food allergy in children: a retrospective cohort study. BMC Pediatr. 2016;16:133.
25. Boyce JA, Assa’ad A, Burks AW, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010:126(6):1105-1108.
26. Atopy definition. American Academy of Allergy, Asthma & Immunology website. https://www.aaaai.org/conditions-and-treatments/conditions-dictionary/atopy. Accessed April 2, 2018.
27. Prevention of allergies and asthma in children. American Academy of Allergy, Asthma & Immunology website. https://www.aaaai.org/conditions-and-treatments/library/allergy-library/prevention-of-allergies-and-asthma-in-children. Accessed October 4, 2018.
28. Du Toit G, Roberts G, Sayre PH, et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372(9):803-812.
29. Perkin MR, Logan K, Tseng A, et al. Randomized trial of introduction of allergenic foods in breast-fed infants. N Engl J Med. 2016;374(18):1733-1743.
30. Mazzocchi A, Venter C, Maslin K, Agostoni C. The role of nutritional aspects in food allergy: prevention and management. Nutrients. 2017;9(8):E850.
31. Berns SH, Halm EA, Sampson HA, Sicherer SH, Busse PJ, Wisnivesky JP. Food allergy as a risk factor for asthma morbidity in adults. J Asthma. 2007;44(5):377-381.


