Today’s Dietitian
Vol. 19, No. 3, P. 36
It’s a huge responsibility, but dietitians are most qualified to discuss ethics, tube feedings, and other tough issues with families of dying patients.
Everyone is going to die.
Death, as heartbreaking as it may be, comes whether we want it to or not. As a geriatric dietitian, I learned quickly that I’d probably outlive all of my patients. I work as a dietitian in a Home Based Primary Care (HBPC) program at the VA. HBPC comprises a multidisciplinary team providing longitudinal, primary care in the homes of veterans whose average age is 76.5.1 Veterans who are admitted into our program typically will live out the remainder of their lives and die while in the program—when, again, I’m reminded that everyone dies.
A letter I received from the wife of a patient who passed away reinforced that dietitians have an important role in end-of-life care. She wrote:
“I am finding it difficult to express in words my deep gratitude to the HBPC team for all that you did to help Taylor and I during the last year of his life. … You gave me so much encouragement in the darkest hours when that horrible scale continued to slide downwards and with it my hopes would slide, too. But you encouraged me to stay the course and assured me that I was doing everything that could possibly be done, and to continue to fight. I thank you for that badly needed boost of strength. … In closing, I guess I will have to use the very simple words ‘Thank You,’ but know that those words come from a place in my heart reserved for a very special few people in my life, and I will never forget how all of you touched mine and Taylor’s life.”
As this letter demonstrates, dietitians can have an influential role in end-of-life care. However, nutrition at end of life is a topic from which many dietitians shy away, either because they’re uncomfortable or lack training in this area, or both. Nonetheless, death is part of life, and it deserves as much dignity, respect, and support as any other aspect of life. RDs are uniquely qualified to support patients and their loved ones and caregivers in decision-making, eating, and dying.
This article will discuss the issues surrounding end-of-life care, such as the difference between hospice and palliative care, and review the risks and benefits of enteral percutaneous endoscopic gastrostomy (PEG) tube feeding in older adults with advanced dementia. It also will offer some tips on how to have those tough conversations with patients and their families about nutrition and end of life.
Defining End-of-Life Care
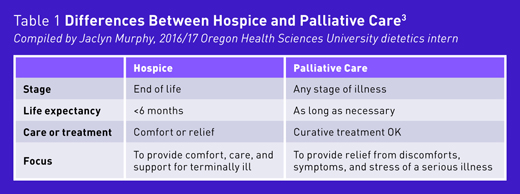
To set the stage for end-of-life discussions, dietitians must know the definition of end-of-life care. According to the National Institute on Aging, end-of-life care is the support and medical care given during the time surrounding death. It isn’t simply the moments before breathing ceases and the heart stops beating. It’s the days, weeks, and months leading up to death.2 To further explain, it’s best to define hospice and palliative care and consider the differences.
Hospice Care
According to the Centers for Medicare & Medicaid Services, hospice is a program of care and support for a dying patient whose doctor and a hospice medical director certify has less than six months to live. The focus of care is on comfort and not curative care.3 This means that a patient must be willing to give up curative treatments to receive hospice care. Some people may not be ready to give this up, and that’s OK. For them, palliative care may be an option.
Palliative Care
Unlike hospice care, patients don’t have to be dying or give up curative treatments to receive palliative care. Palliative care has a role in end of life, but it isn’t exclusively for end of life. Palliative care is a treatment available to anyone of any age who’s in need of relief from the discomforts, symptoms, and stress of a serious illness. Older persons living with chronic illnesses may benefit from palliative care long before the need for hospice.3
Important Documents
There are two important documents to consider at end of life: the advance directive and the Physician Orders for Life-Sustaining Treatment (POLST). The advance directive is a legal document meant to provide guidance in the types of treatment patients want to receive if they’re unable to make decisions for themselves—they either are unconscious or have developed a condition that renders them incompetent to make decisions (eg, advanced dementia).4 The term advance directive varies by state. It may be called a living will, health care power of attorney, or another name.
The POLST is an important document stating what patients want at the end of life. There’s a section on artificially administered nutrition that gives patients three options: 1) no artificial nutrition by tube, 2) a defined trial period of artificial nutrition by tube, or 3) full-term artificial nutrition by tube.4 If a patient doesn’t have this document, it may be a good idea to recommend they get a POLST so they can ensure their wishes are known. When a patient is unable to make decisions and doesn’t have either of these documents in place, the laws dictating what happens regarding consent will vary by state. However, in these cases, a family member (eg, spouse, parent, or adult child) usually ends up making these decisions. Knowing a patient’s wishes for artificial nutrition is important, particularly because there’s controversy regarding whether tube feedings are beneficial for older adults with advanced dementia at the end of life.
Ethics of Tube Feedings in Advanced Dementia Cases
While tube feeding has been commonplace in nursing homes and leads to increased nutrition and calories in the older adult with advanced dementia, it remains unclear whether it confers other benefits. According to a review of randomized controlled trials, there’s insufficient evidence showing that tube feedings increase quality of life or survival.5 Side effects of tube feeding may include aspiration, infection, increased oral secretions, tube malfunction, and discomfort.
A 2014 study of nursing home residents found a small but significant increase in annual inpatient health care costs post-PEG tube insertion along with an increase in hospital and ICU days.6 However, overall rates of feeding tube insertion among US nursing home residents with advanced dementia have declined over the years from 11.7% in 2000 to 5.7% in 2014.7 Fewer patients with advanced dementia are getting tube feedings.
Expert opinion and position statements from national organizations increasingly advocate against the routine practice of placing feeding tubes in patients with advanced dementia but promote honoring patients’ wishes. The American Geriatrics Society’s position on feeding tubes in advanced dementia states: When eating difficulties arise, feeding tubes aren’t recommended for older adults with advanced dementia. However, health care providers should promote choice, endorse shared and informed decision-making, and honor preferences regarding tube feeding.8
According to a 2014 article in Nutrition in Clinical Practice, based on current scientific literature, long-term enteral access devices should be withheld in patients with advanced dementia or other near end-of-life conditions. However, the authors do note that a patient’s autonomy and cultural, religious, social, and emotional value systems should be respected.9 There’s more behind this topic than just the science; there are people and their beliefs.
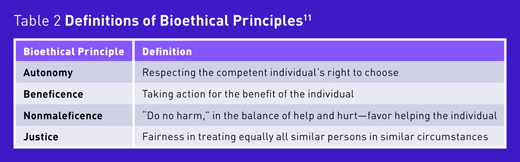
In 2016, the European Society for Clinical Nutrition and Metabolism published a guideline on ethical aspects of artificial nutrition and hydration. The guideline offers 36 statements with level of consensus on a variety of ethical topics in this area. In regard to ethical principles, it emphasizes: The ethical principles “autonomy, beneficence, nonmaleficence, and justice” are internationally recognized. They are interrelated and have to be applied in the act of medical decision-making [Strong Consensus].10 (See Table 2 for definitions of these bioethical principles.)
Dietetics organizations also recognize the growing importance of ethics in all areas of health care. The Commission on Dietetic Registration (CDR) code of ethics applies to all CDR-credentialed practitioners. The code of ethics guides dietetics practitioners in their professional practice and conduct. It includes the fundamental principles and responsibilities to the public, clients, the profession, colleges, and other professionals.11
The Academy of Nutrition and Dietetics position paper “Ethical and Legal Issues in Feeding and Hydration,” has a wealth of information.12 It summarizes dietitians’ responsibilities and the active role they have in ethical deliberations. RDs are responsible for providing sound, technical judgment, knowing what patients want, and supporting them as appropriate.13 Dietitians must support patients in whatever decisions they make, even if they aren’t decisions they’d make for themselves.
With regard to some of the legal aspects of ethics and end of life, no single event in the past has occurred that now guides professional organizations and medical references surrounding biology and life or bioethics. Many court cases have set the landscape for bioethics in health care. One landmark case in particular helped pave the way for ethics in nutrition and dietetics: Cruzan v. Director, Missouri Department of Health.
Nancy Cruzan was in a persistent vegetative state (ie, no sign of brain function) and was receiving artificial nutrition and hydration. In 1990, the US Supreme Court ruled that receiving food and water through tubes administered by nurses and doctors constituted medical treatment, and that if there were clear and convincing evidence (ie, statements/directives made when a patient is still competent) that the patient wanted to discontinue artificial feeding, then the feeding tubes could have been withdrawn. Because of this case, a guardian may honor the wishes of a patient in a persistent vegetative state to discontinue artificial nutrition and hydration. This case also made clear that the Constitution gives a competent person a protected right to refuse lifesaving hydration and nutrition.14
More recently, a 2016 case involved a patient that had been diagnosed with early-onset Alzheimer’s. She completed an advance directive and let her family members know she didn’t want them to take measures to prolong her life. Later, as the disease progressed, her husband filed a civil case to stop spoon-feeding provided by her nursing home. He lost the case. The judge who made the decision said they couldn’t stop the spoon-feeding because not helping the patient eat would be a violation of state law. This ruling brings up a few thoughts: End-of-life documents often deal with artificial nutrition/hydration but not necessarily spoon-feeding. Rules and laws vary by state, and nutrition at end of life continues to be an evolving ethical issue.15
Nutrition at Very End of Life
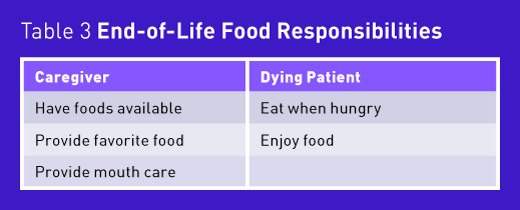
Reduced food intake that occurs in the weeks, days, and hours before death can be extremely difficult on caregivers and their families. People usually associate food with nourishment and love. They don’t want their loved ones to suffer. Often, a loved one tries to push or force foods on the patient. However, forcing foods and fluids on a patient at end of life won’t enhance or prolong life. It may be a burden or cause uncomfortable symptoms such as bloating, nausea, vomiting, diarrhea, constipation, edema, and/or gastric reflux leading to aspiration.16
When end of life nears, there are few precious moments to be had between dying patients and their loved ones. Issues around nutrition can affect those precious moments. Caregivers often feel guilty because they think they’re causing a loved one to starve to death, and dying patients who want to please loved ones force themselves to eat and feel miserable. This is where dietitians can make an impact on the lives of dying patients and their families. They can provide education and support in what this process looks like and guide them through each step.
Decreased appetite and the loss of thirst are natural processes that enable the body to prepare itself for death. Here’s an explanation of what takes place: A healthy individual has an anabolic metabolism, which can use nutrients to build and repair tissue. However, during the dying process, the body shifts from an anabolic to a catabolic state, which refers to breaking down organic molecules. It’s this catabolic condition that leads to starvation and dehydration. This shift is a natural part of the dying process, which slows down bodily functions such as gastric emptying, leading to increased satiety and therefore a decreased sense of hunger.17 When the body doesn’t get the glucose it needs for energy, it begins to use fat for energy, which in turn produces ketones. As ketones build up, the resulting ketonemia further reduces hunger and may be associated with euphoria and a sense of well-being.16
Moreover, water deprivation and dehydration at end of life has been shown to decrease the perception of suffering.17 Many studies show that when steps are taken to moisturize the patient’s mouth with ice chips, lip balm, or moistened swabs, they can alleviate uncomfortable dry mouth without the use of artificial hydration.18,19
Bottom Line
Due to these issues surrounding nutrition at end of life, conversations with patients and loved ones can be difficult, but developing the skills to have them is important for all dietitians. If it feels appropriate to broach these discussions, ask the patient and caregiver for permission to discuss what nutrition looks like at very end of life. Emphasize that no one knows exactly when the end will come, and discuss the importance of honoring the patient’s wishes, as outlined in Table 3. In addition, try to encourage loved ones to find nonfood ways of demonstrating love and care.
Nutrition at end of life is a challenging but important topic for dietitians to embrace, but they have an active role in end-of-life care. They’re knowledgeable about ethics, they can provide education on the risks and benefits of tube feeding in older adults with advanced dementia, and they understand how starvation relates to the dying process; therefore, they’re most qualified to have these tough conversations with patients and caregivers. Everyone dies, but we can become comfortable in talking about it. Tackling this subject the right way will enable dietitians to truly help those at end of life enjoy the precious moments they have left.
— Katie M. Dodd, MS, RD, CSG, LD, FAND, is a home-based primary care dietitian for the Veterans Health Administration in White City, Oregon. She’s a board-certified specialist in gerontological nutrition and the current president of the Oregon Academy of Nutrition and Dietetics.
References
1. Beales JL, Edes T. Veteran’s Affairs Home Based Primary Care. Clin Geriatr Med. 2009;25(1):149-154, viii-ix.
2. End of life: helping with comfort and care. NIH National Institute on Aging website. https://www.nia.nih.gov/health/publication/end-life-helping-comfort-and-care/introduction. Updated August 10, 2016. Accessed December 3, 2016.
3. Preparing for the end of life. National Institutes for Health (NIH) Senior Health website. https://nihseniorhealth.gov/endoflife/preparingfortheendoflife/01.html. Updated March 2014. Accessed December 3, 2016.
4. National POLST Paradigm website. http://polst.org. Accessed December 3, 2016.
5. Candy B, Sampson EL, Jones L. Enteral tube feeding in older people with advanced dementia: findings from a Cochrane systematic review. Int J Palliat Nurs. 2009:15(8):396-404.
6. Hwang D, Teno JM, Gozalo P, Mitchell S. Feeding tubes and health costs postinsertion in nursing home residents with advanced dementia. J Pain Symptom Manage. 2014;47(6):1116-1120.
7. Mitchell SL, Mor V, Gozalo PL, Servadio JL, Teno JM. Tube feeding in US nursing home residents with advanced dementia, 2000-2014. JAMA. 2016;316(7):769-770.
8. American Geriatrics Society Ethics Committee and Clinical Practice and Models of Care Committee. American Geriatrics Society feeding tubes in advanced dementia position statement. J Am Geriatr Soc. 2014;62(8):1590-1593.
9. Schwartz DB, Barrocas A, Wesley JR, et al. Gastrostomy tube placement in patients with advanced dementia or near end of life. Nutr Clin Pract. 2014;29(6):829-840.
10. Druml C, Ballmer PE, Druml W, et al. ESPEN guideline on ethical aspects of artificial nutrition and hydration. Clin Nutr. 2016;35(3):545-556.
11. American Dietetic Association. American Dietetic Association/Commission on Dietetic Registration code of ethics for the profession of dietetics and process for consideration of ethics issues. J Am Diet Assoc. 2009;109(8):1461-1467.
12. O’Sullivan Maillet J, Baird Schwartz D, Posthauer ME; Academy of Nutrition and Dietetics. Position of the Academy of Nutrition and Dietetics: ethical and legal issues in feeding and hydration. J Acad Nutr Diet. 2013;113(6):828-833.
13. Schwartz DB, Posthauer ME, O’Sullivan Maillet J. Practice paper of the Academy of Nutrition and Dietetics abstract: ethical and legal issues of feeding and hydration. J Acad Nutr Diet. 2013;113(7):981.
14. U.S. Supreme Court. Cruzan v. Director, Missouri Department of Health. Wests Supreme Court Report. 1990;110:2841-2892.
15. Aldous V. Ashland woman didn’t want life prolonged, but state says she must be spoon-fed. Mail Tribune. September 18, 2016. http://www.mailtribune.com/news/20160918/ashland-woman-didnt-want-life-prolonged-but-state-says-she-must-be-spoon-fed. Updated September 18, 2016. Accessed December 3, 2016.
16. Winter SM. Terminal nutrition: framing the debate for the withdrawal of nutrition support in terminally ill patients. Am J Med. 200;109(9):723-726.
17. Niedert K, Carlson M. Nutrition Care of the Older Adult: A Handbook for Nutrition Throughout the Continuum of Care. Chicago, IL: Academy of Nutrition and Dietetics; 2016.
18. Bennett J. Dehydration: hazards and benefits. Geriatr Nurs. 2000;21(2):84-88.
19. Pasman HR, Onwuteaka-Philipsen BD, Kriegsman DM, Ooms ME, Ribbe MW, van der Wal G. Discomfort in nursing home patients with severe dementia in whom artificial nutrition and hydration is forgone. Arch Intern Med. 2005;165(15):1729-1735.


