Today’s Dietitian
Vol. 19, No. 12, P. 28
Here’s what we know and what’s still unclear about the health benefits of this nutrient that Americans aren’t getting enough of.
The 2015–2020 Dietary Guidelines for Americans identified vitamin E (specifically, the form known as α-tocopherol) as a “shortfall nutrient”; in a general sense, more than 90% of Americans don’t meet the estimated average requirement. Still, clinical deficiencies in the United States are rare but are believed to be more common in other countries.
Despite decades of research and an official Recommended Dietary Allowance (RDA) of 15 mg per day, it’s difficult to confidently identify the role vitamin E plays in disease prevention and health.1 Further complicating the vitamin E story is the fact that it isn’t a single entity but a collective term given to a group of fat-soluble vitamins, of which α-tocopherol (alpha-tocopherol) and γ-tocopherol (gamma-tocopherol) are two major forms used by the body, and another branch of the vitamin E family, tocotrienols.2
What We Know
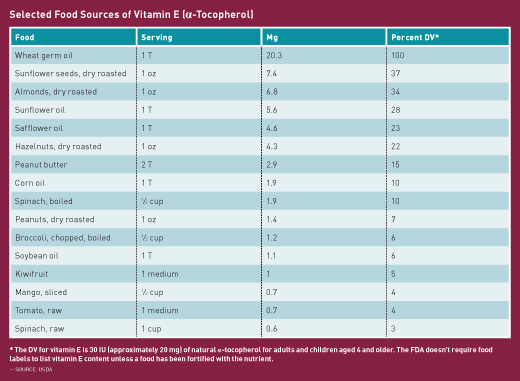
Vitamin E was discovered in 1922, but it wasn’t until the 1980s that vitamin E deficiency was identified as a condition in humans. It took almost another decade before deficiency symptoms were recognized. Vitamin E is found naturally in several foods, including wheat germ, acai berries, avocados, almond milk, sunflower seeds, almonds, peanut butter, and safflower oil. Other sources include tomatoes, spinach, asparagus, Swiss chard, and broccoli. Naturally occurring vitamin E (tocopherol) exists in eight chemical forms (alpha-, beta-, gamma-, and delta-tocopherol, and alpha-, beta-, gamma-, and delta-tocotrienol). Natural vitamin E (d-α-tocopherol) and synthetic vitamin E (dl-α-tocopherol) are both found in some supplements. Alpha-tocopherol is believed to be the only form that meets the requirement for vitamin E, though tocotrienols and γ-tocopherol are thought to be better scavengers of free radicals than α-tocopherol.3 In the body, α-tocopherol is preferentially retained in the liver, which incorporates the vitamin into lipoproteins for delivery to body tissues. However, other forms of vitamin E also are actively metabolized and excreted.
Alpha-tocopherol functions as an antioxidant, preventing the formation of tissue-damaging free radicals in cell membranes and plasma lipoproteins. In fact, it’s the first line of defense against oxidation of cell membranes. Gamma-tocopherol traps and neutralizes existing free radicals.2 It’s likely also involved in strengthening cell-mediated immunity.4
Causes of Deficiency
While vitamin E deficiency is rare in the US population, it can be caused by fat malabsorption disorders, malnutrition, or genetic abnormalities that affect vitamin E metabolism. Severe deficiency symptoms include muscle weakness, neuropathy, and damage to the retina. If deficiency goes untreated, it can lead to muscle deterioration, including the heart muscle. Deficiency is more likely to be found in children, as they have limited vitamin E stores and are growing rapidly, which increases demand.5 Cigarette smoking is thought to increase the utilization of α-tocopherol, possibly putting smokers at increased risk of deficiency compared with nonsmokers.6
Consequences of Large Doses and Contraindications
Large doses of vitamin E may inhibit vitamin K and thus interfere with blood coagulation.7 Specifically, the use of vitamin E supplements may increase the risk of bleeding in individuals taking blood thinners, such as heparin and warfarin (Coumadin); antiplatelet drugs, such as clopidogrel (Plavix), ticlopidine (Ticlid), tirofiban (Aggrastat), and aspirin/dipyridamole (Aggrenox); and NSAIDs, including aspirin, ibuprofen, and naproxen sodium (Aleve). In addition, individuals who may be vitamin K deficient as a result of liver failure, those with a propensity to bleed (eg, bleeding peptic ulcers), and those with inherited bleeding disorders (eg, hemophilia) or a history of hemorrhagic stroke shouldn’t take α-tocopherol supplements without close medical supervision because of the increased risk of hemorrhage.8 Vitamin E also could exacerbate the antithrombotic activity of fish oils and herbal products, such as garlic, curcumin, and Ginkgo biloba.9
Conversions Made Easy
Quantifying vitamin E can be confusing, as it’s expressed in either IU or mg. The conversions are calculated as follows:
• To convert from mg to IU: 1 mg of α-tocopherol is equivalent to 1.49 IU of the natural form or 2.22 IU of the synthetic form.
• To convert from IU to mg: 1 IU of the natural form is equivalent to 0.67 mg of α-tocopherol. 1 IU of the synthetic form is equivalent to 0.45 mg of α-tocopherol.
While natural vitamin E often is viewed as being the better option, according to Tod Cooperman, MD, president and founder of ConsumerLab.com, a company that provides independent test results, reviews, ratings, and comparisons of vitamins, supplements, and herbal and nutrition products for consumers, “Both natural and synthetic vitamin E in the proper doses can be equally effective.” However, he says, “It takes more IUs of synthetic vitamin E than natural vitamin E to get an equivalent amount of the active vitamin, but it also takes fewer IUs of synthetic vitamin E to cause potential bleeding problems when high doses are used.”
While γ-tocopherol is the most common form of vitamin E in the American diet,10 its plasma and tissue concentrations generally are much lower than those of α-tocopherol, and because more γ-tocopherol is excreted in urine than α-tocopherol, it’s believed the body needs less γ-tocopherol for its use.4
Vitamin E in Metabolic Syndrome, Chronic Disease Prevention
According to Maret Traber, PhD, a professor with the Linus Pauling Institute at Oregon State University and a vitamin E researcher, “People with metabolic syndrome are more likely to have impaired absorption and transport of vitamin E, so their requirements may be higher than the current RDA.” Metabolic syndrome generally is defined as a collection of factors, including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels, which together increase a person’s risk of heart attack and stroke. A study in which Traber was involved cited inflammation and oxidative stress of metabolic syndrome as possible causes for limited absorption of α-tocopherol in the small intestine and impairment of liver metabolism of the vitamin.11
Numerous studies have suggested that tocotrienols might be beneficial in the prevention of chronic diseases.12 Tocotrienols (especially δ-tocotrienol) have shown greater anticancer effects than tocopherols in malignant cells in laboratory studies.13 However, in a clinical study, dose, formulation, and study population would affect the bioavailability of tocotrienols and alter findings.14 Currently, there are no clinical studies on the efficacy of supplemental tocotrienols in humans.12
“Throughout my practice, I have yet to find a patient that needed vitamin E supplementation,” says Kristen Smith, MS, RDN, LD, a spokesperson for the Academy of Nutrition and Dietetics. “Typically, if a patient is suspected of being deficient in vitamin E, other micronutrient deficiencies are present and a multivitamin is best suited for them.” The patient’s primary care physician can order blood tests to determine vitamin E levels, but this isn’t a blood test that’s routinely administered. If cost or lack of insurance is a factor, a food journal should reveal whether vitamin E intake is inadequate.
What We Think We Know
Randomized controlled trials investigating prevention of chronic diseases, such as CVD, cancer, and cataracts, don’t support a preventive effect of supplemental α-tocopherol.4 However, limited clinical evidence suggests vitamin E supplementation may be beneficial for age-related macular degeneration and fatty liver diseases resulting from type 2 diabetes. Supplementation with α-tocopherol was found to slow cognitive decline in some, but not all, clinical studies.4
Results of several large prospective observational studies in men and women have suggested an inverse relationship between dietary vitamin E consumption and risk of myocardial infarction or death from heart disease. In two of the studies, individuals who consumed more than 7 mg per day of dietary α-tocopherol were 35% less likely to die from heart disease than those who consumed less than 3 to 5 mg per day.15,16 Two other large studies found that the risk of heart disease was significantly reduced in men who consumed at least 100 IU (67 mg) per day of supplemental natural tocopherol.17,18
Effects on Cancer Risk, Pregnancy, Mild Cognitive Impairment
Because of its ability to neutralize free radicals, vitamin E has been suggested to possess anticancer properties by virtue of its ability to protect cells against oxidative damage. However, large prospective cohort studies have failed to show significant associations between dietary and supplemental vitamin E intake and the incidence of lung or breast cancer.19 More recently, the prospective VITamins And Lifestyle (VITAL) study evaluated the association between the use of supplemental vitamins over 10 years and the risk of lung cancer in more than 77,000 men and women.20 No relationships were reported between intake of multivitamins, vitamin C, vitamin E, or folate and the risk of lung cancer. However, the use of supplemental vitamin E in current smokers, but not in former smokers, was associated with an 11% increased risk of lung cancer for every 100 mg per day increase in vitamin E intake, and intakes greater than 215 mg per day were specifically linked to a 29% increase in risk of nonsmall-cell lung cancer.
It also has been suggested that vitamin E supplements might reduce colon cancer risk. However a meta-analysis of four placebo-controlled trials found no evidence that vitamin E supplementation reduces colorectal cancer risk.21 To date, most clinical trials have failed to find any beneficial effects of vitamin E supplementation on the risk of various cancers.4 Overall, observational studies haven’t found vitamin E, either from food or supplements, to offer protection against cancer.
Some studies have suggested that vitamin E supplements during pregnancy may improve outcomes for babies and mothers. However, a recent review concluded that supplementation of vitamin E in combination with other supplements had no effect on pregnancy outcomes.22
A few studies suggest that α-tocopherol supplements have no effect on mild cognitive impairment, but there’s evidence, though limited, that it may slow functional decline associated with Alzheimer’s disease.23 Guidelines published in the journal Neurobiology of Aging recommend lifestyle changes to reduce dementia risk. Among them: “Vitamin E should come from foods, rather than supplements. Healthful food sources of vitamin E include seeds, nuts, green leafy vegetables, and whole grains.”24
There appear to be few side effects in adults taking supplements containing less than 2,000 mg per day of either natural or synthetic α-tocopherol. However, most studies have lasted only a few weeks to a few months. A meta-analysis of randomized controlled trials found that daily vitamin E supplementation—equivalent to 25 to 536 mg per day of d-α-tocopherol—for several years resulted in a 10% reduction in ischemic stroke risk and a trend toward an increased risk of hemorrhagic stroke, the opposite effect of large doses.25
The Food and Nutrition Board of the Institute of Medicine established the Tolerable Upper Intake Level (UL) for supplemental α-tocopherol to avoid the potential risk of bleeding. The UL of 1,000 mg per day of α-tocopherol in any supplemental form (equivalent to 1,500 IU per day of d-α-tocopherol or 1,100 IU per day of dl-α-tocopherol) is the highest dose unlikely to result in hemorrhage in adults.19 Although only certain forms of α-tocopherol are used by the body, all forms are absorbed and metabolized by the liver, so the UL is based on the fact that any form of α-tocopherol can be absorbed and thus be potentially harmful.4
Recommendations
Little evidence is conclusive about the effects of vitamin E on health, other than that a clinical deficiency can result in illness and eventually death. Experts agree that more research is needed to determine whether supplemental vitamin E is beneficial and in which form and at what dose. Most multivitamins provide adequate amounts of vitamin E that equal or exceed the RDA. Traber says that until additional findings are evaluated, “A multivitamin will provide the RDA not only for vitamin E but other vitamins as well; that is my preference over a single vitamin E pill.”
— Densie Webb, PhD, RD, is a freelance writer, editor, and consultant based in Austin, Texas.
References
1. Niki E, Traber MG. A history of vitamin E. Ann Nutr Metab. 2012;61(3):207-212.
2. Rizvi S, Raza ST, Ahmed F, Ahmad A, Abbas S, Mahdi F. The role of vitamin E in human health and some diseases. Sultan Qaboos Univ Med J. 2014;14(2):e157-e165.
3. Brown KM, Morrice PC, Duthie GG. Erythrocyte vitamin E and plasma ascorbate concentrations in relation to erythrocyte peroxidation in smokers and nonsmokers: dose response to vitamin E supplementation. Am J Clin Nutr. 1997;65(2):496-502.
4. Vitamin E. Oregon State University, Linus Pauling Institute, Micronutrient Information Center website. http://lpi.oregonstate.edu/mic/vitamins/vitamin-E. Accessed October 11, 2017.
5. Traber MG. Vitamin E inadequacy in humans: causes and consequences. Adv Nutr. 2014;5(5):503-514.
6. Leonard SW, Bruno RS, Ramakrishnan R, Bray T, Traber MG. Cigarette smoking increases human vitamin E requirements as estimated by plasma deuterium-labeled CEHC. Ann N Y Acad Sci. 2004;1031:357-360.
7. Booth SL, Golly I, Sacheck JM, et al. Effect of vitamin E supplementation on vitamin K status in adults with normal coagulation status. Am J Clin Nutr. 2004;80(1):143-148.
8. Pastori D, Carnevale R, Cangemi R, et al. Vitamin E serum levels and bleeding risk in patients receiving oral anticoagulant therapy: a retrospective cohort study. J Am Heart Assoc. 2013;2(6):e000364.
9. Hendler SS, Rorvik DM. PDR for Nutritional Supplements. 2nd ed. Montvale, NJ: Thomson Reuters; 2008.
10. Jiang Q, Christen S, Shigenaga MK, Ames BN. gamma-tocopherol, the major form of vitamin E in the US diet, deserves more attention. Am J Clin Nutr. 2001;74(6):714-722.
11. Mah E, Sapper TN, Chitchumroonchokchai C, et al. α-Tocopherol bioavailability is lower in adults with metabolic syndrome regardless of dairy fat co-ingestion: a randomized, double-blind, crossover trial. Am J Clin Nutr. 2015;102(5):1070-1080.
12. Ahsan H, Ahad A, Iqbal J, Siddiqui WA. Pharmacological potential of tocotrienols: a review. Nutr Metab (Lond). 2014;11(1):52.
13. Constantinou C, Papas A, Constantinou AI. Vitamin E and cancer: an insight into the anticancer activities of vitamin E isomers and analogs. Int J Cancer. 2008;123(4):739-752.
14. Fu JY, Che HL, Tan DM, Teng KT. Bioavailability of tocotrienols: evidence in human studies. Nutr Metab (Lond). 2014;11(1):5.
15. Knekt P, Reunanen A, Järvinen R, Seppänen R, Heliövaara M, Aromaa A. Antioxidant vitamin intake and coronary mortality in a longitudinal population study. Am J Epidemiol. 1994;139(12):1180-1189.
16. Kushi LH, Folsom AR, Prineas RJ, Mink PJ, Wu Y, Bostick RM. Dietary antioxidant vitamins and death from coronary heart disease in postmenopausal women. N Engl J Med. 1996;334(18):1156-1162.
17. Rimm EB, Stampfer MJ, Ascherio A, Giovannucci E, Colditz GA, Willett WC. Vitamin E consumption and the risk of coronary heart disease in men. N Engl J Med. 1993;328(20):1450-1456.
18. Stampfer MJ, Hennekens CH, Manson JE, Colditz GA, Rosner B, Willett WC. Vitamin E consumption and the risk of coronary disease in women. N Engl J Med. 1993;328(20):1444-1449.
19. Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. Washington, D.C.: National Academy Press; 2000.
20. Slatore CG, Littman AJ, Au DH, Satia JA, White E. Long-term use of supplemental multivitamins, vitamin C, vitamin E, and folate does not reduce the risk of lung cancer. Am J Respir Crit Care Med. 2008;177(5):524-530.
21. Arain MA, Abdul Qadeer A. Systematic review on “vitamin E and prevention of colorectal cancer.” Pak J Pharm Sci. 2010;23(2):125-130.
22. Rumbold A, Ota E, Hori H, Miyazaki C, Crowther CA. Vitamin E supplementation in pregnancy. Cochrane Database Syst Rev. 2015;9:CD004069.
23. Farina N, Llewellyn D, Issac MG, Tabet N. Vitamin E for Alzheimer’s dementia and mild cognitive impairment. Cochrane Database Syst Rev. 2017;1:CD002854.
24. Barnard ND, Bush AI, Ceccarelli A, et al. Dietary and lifestyle guidelines for the prevention of Alzheimer’s disease. Neurobiol Aging. 2014;35(Suppl 2):S74-S78.
25. Schürks M, Glynn RJ, Rist PM, Tzourio C, Kurth T. Effects of vitamin E on stroke subtypes: meta-analysis of randomised controlled trials. BMJ. 2010;341:c5702.