Today’s Dietitian
Vol. 19, No. 11, P. 46
Research shows it’s the most effective eating pattern for lowering blood pressure, so how can dietitians get clients more excited about its virtues?
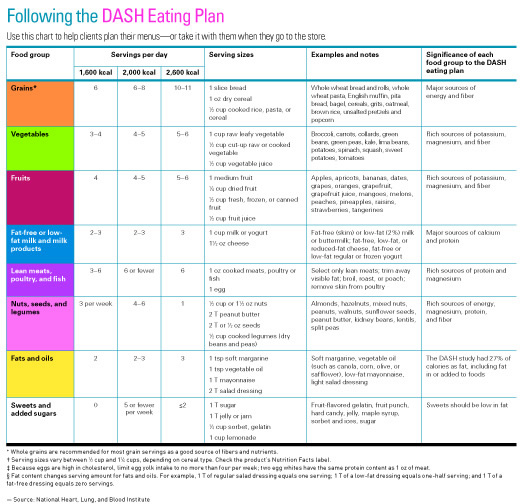
This year marks the 20th anniversary of the DASH (Dietary Approaches to Stop Hypertension) diet. The diet, which emphasizes foods rich in protein, fiber, potassium, magnesium, and calcium (fruits and vegetables, beans, nuts, whole grains, and low-fat dairy), has been shown time and again to be effective in lowering elevated blood pressure. More recent research has suggested it also can be effective in reducing inflammation markers, lowering the risk of developing kidney disease (a common complication of hypertension), and decreasing levels of low-density lipoproteins (an established risk factor for CVD) and several types of cancer.
Each year, US News & World Report ranks the best diets based on expert advice in areas such as ease of compliance, weight loss results, and effectiveness against CVD and diabetes. The DASH diet has come in at number one for seven years in a row. So why isn’t DASH the dietary darling, with thousands of consumers clamoring to get the latest information as they do for the likes of Paleo, Atkins, the Alkaline Diet, or Whole30?
That’s a good question.
Hypertension
Blood pressure is the measure of the force of blood flowing through blood vessels. Almost 86 million people in the United States have high blood pressure, and only one-half have it under control. About 13 million US adults with hypertension aren’t even aware they have it and are going untreated.1 There are many causes of hypertension, but whatever the cause, the harmful repercussions include damaged arteries, aneurysms, enlarged heart, transient ischemic attack, stroke, dementia, kidney failure, retinopathy, sexual dysfunction in men, sleep apnea, and bone loss. That makes controlling blood pressure critical for disease prevention.2 High blood pressure can be defined as a reading higher than 140/90 mm Hg. Prehypertension is between 120/80 mm Hg and 139/89 mm Hg. Prehypertension is likely to become hypertension unless lifestyle changes, including diet, are made.2 The DASH diet is rich in several nutrients known to play important roles in regulating blood pressure, including potassium, magnesium, and calcium, and is lower in sodium and saturated fat than the typical American diet.
DASH Research
While sodium reduction alone often is a physician’s go-to recommendation for lowering blood pressure, the DASH diet shows that reducing blood pressure through diet is the result of combining a team of nutrients—and sodium isn’t the standout. It’s the symbiosis of the DASH nutrients working together that makes the difference. The DASH dietary pattern consistently has proven to be effective for lowering blood pressure in diverse populations, including men, women, white individuals, and in those of various races and ethnicities who have either prehypertension or hypertension.3
The original study to examine the efficacy of the DASH diet was conducted at four sites as a randomized controlled feeding study. While the diet provided 3,600 mg of sodium per day—significantly more than the current recommendation of 2,300 mg—it showed significant reductions in blood pressure as quickly as two weeks after the start of the diet, suggesting that the combination of foods and nutrients is what provides the greatest blood pressure-lowering effects.4
Since then, several studies have shown the DASH dietary pattern to have a wide range of benefits. A recent examination of National Health and Nutrition Examination Survey (NHANES) data found that following a DASH-style diet was associated with metabolic health (eg, fasting glucose, insulin resistance, C-reactive protein, and high-density lipoproteins) in young, healthy overweight, and obese individuals.5
As part of the Atherosclerosis Risk in Communities Study, it was found that participants with the lowest DASH scores were 16% more likely to develop kidney disease than those with the highest scores, even after taking into account several factors, such as smoking status, physical activity, and hypertension. DASH scores (there are more than one) are a way to compare an individual’s diet with the DASH dietary pattern. Of the individual components of the DASH diet score, high intakes of nuts, legumes, and low-fat dairy products were associated with reduced risk of kidney disease.6
A systematic review and meta-analysis of observational prospective studies found that a DASH-style diet decreases the risk of heart failure by 29%, coronary heart disease by 21%, and stroke by 19%.7
Data from the Multiethnic Cohort study, which included black, Native Hawaiian, Japanese American, Latino, and white individuals, found that following a DASH-style diet significantly reduced the risk for colorectal cancer. The overall effect was greater in men than in women and was less strong among blacks compared with the other racial/ethnic groups.5
Recommended by the 2015–2020 Dietary Guidelines for Americans as a healthful dietary pattern,8 the DASH diet is an amalgam of every healthful eating recommendation that health and nutrition experts have been making for decades, eg, eat more fruits and vegetables, low-fat dairy, nuts and seeds, beans, and whole grains, and lower intake of sodium and sugar.
Few DASH Followers
Despite the overwhelming evidence that the DASH diet can reduce high blood pressure, and the growing number of studies suggesting that it can lower the risk of several other chronic diseases, few people adopt the DASH as their primary eating pattern. Data from the 1988–2004 NHANES found that only 20% of those surveyed met even one-half of the recommended levels of nutrients found in the DASH diet.9 An analysis of the data from 2007–2012 NHANES found that the average DASH score was 2.6 out of a possible nine. The score was based on nine nutrients: sodium, cholesterol, saturated fat, total fat, protein, calcium, magnesium, potassium, and fiber.10
One of the possible reasons DASH hasn’t gained a foothold in the American obsession with diet is that it isn’t a diet for weight loss; it’s a dietary pattern designed for disease prevention and improved health. It’s not the easiest diet to follow for life, and the name isn’t as catchy as, say, Whole30.
“DASH may need a rebranding,” says Dori Steinberg, PhD, RD, an assistant professor at the Duke Global Institute, Durham, North Carolina. Steinberg agrees that it’s not the most appealing name, and few consumers know what DASH stands for.
Marla Heller, MS, RDN, author of four books on the DASH diet, including The DASH Diet Action Plan and The Everyday DASH Diet Cookbook, says that in her experience, people think that DASH refers to the seasoning of the same name.
Any diet that’s low in saturated fat is tough to follow, even with intensive dietary counseling.11 To address that issue, a study by Chiu and colleagues published in 2016 examined the effectiveness of a DASH dietary pattern that was much higher in both total fat (40% of calories vs 27% of calories) and saturated fat (14% of calories vs 8% of calories) and found that when the rest of the diet is followed, the benefits on blood pressure and blood lipids were the same. While the higher-fat diet was higher in total fat and saturated fat, and provided more full-fat dairy than the original DASH diet, it provided more vegetables, more nuts and legumes, less sugar, and less fruit and fruit juice. The higher-fat version might make it easier to follow and stick with over the long term. However, Heller says the study sample size was small and the study was of a short duration.
DASH Apps
Mobile apps are being developed to increase compliance with the DASH plan. The DASH Cloud is one such app in development at the Duke Global Health Institute. “We’re trying to see how we can leverage technology to promote DASH,” Steinberg says. There are thousands of diet and fitness apps to track calories and activity, she says, but few focus on diet quality. It’s currently in the testing stage. Steinberg works with one of the original developers of the DASH diet, and she says they want people to be aware of all the nutrients that lower blood pressure. The goal is to pair the DASH Cloud with a good diet tracker app and offer messaging to users that provides ways to increase their DASH score throughout the day.
However, not everyone agrees that apps are the way to go. “I think that too much reliance on outside factors, such as an app, doesn’t create habits that make it easy to follow a healthful eating plan for a lifetime,” Heller says.
Affordability and Environmental Impact
Previous research has found that dietary costs are strongly associated with diet quality.12 Following the DASH dietary pattern is no exception. The study, which was conducted in the United Kingdom (UK), found that the closer the adherence to the DASH dietary pattern, the greater the dietary costs. Those with the highest DASH scores had 18% greater food costs than those with the lowest DASH scores. Fast food is cheap; foods in the DASH diet, such as fresh fruits and vegetables and nuts, tend to be more expensive. In fact, a recent study suggested that the likelihood of consuming a DASH-like diet was dependent on both geographic and economic access.13 The study was conducted in the UK, but there’s no reason the findings wouldn’t apply to the United States. The researchers found that the likelihood of consuming a DASH-like diet was 58% lower in households with the lowest dietary costs. And those living the farthest from any supermarket were 15% less likely to consume DASH-like diets.
In addition to being a diet for good health, DASH is also good for the planet. The UK study found that the more closely the dietary pattern resembled the DASH diet, the lower the associated greenhouse gas production.12
Recommendations
Heller says offering practical advice can make following the DASH plan easier and longer lasting. The DASH dietary pattern isn’t for the short term, she says; it’s for life. “If a plan can’t be sustained,” she says, “why go to the trouble of trying to follow it in the first place?” She offers the following suggestions to help clients and patients follow the DASH diet:
• Use frozen fruits and vegetables; it’s a more economical way to increase fruit and vegetable intake, which is a major component of the DASH diet.
• Fill half the plate with nonstarchy vegetables, and include a lean protein-rich food.
• Add a salad, preferably with an olive oil-based dressing, and fruit for dessert.
• Eat fruit, raw veggies, yogurt, cheese, nuts, or hard-boiled eggs for snacks.
• At breakfast, choose a whole grain such as toast or cereal that’s low in added sugars.
• Have milk as hot chocolate or a latte to make it more appealing.
• Always balance snacks and meals with something protein-rich (eg, cheese, eggs, nuts, yogurt) and something bulky and filling (eg, fruits or veggies).
• Remember that DASH isn’t a diet; it’s a lifestyle change to reduce the risk of chronic disease.
— Densie Webb, PhD, RD, is a freelance writer, editor, and consultant based in Austin, Texas.
References
1. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics — 2017 Update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603.
2. High blood pressure (hypertension). Mayo Clinic website. http://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/high-blood-pressure/art-20045868?pg=2. Updated November 23, 2016. Accessed September 9, 2017.
3. Steinberg D, Bennett GG, Svetkey L. The DASH diet, 20 years later. JAMA. 2017;317(15):1529-1530.
4. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117-1124.
5. Park YM, Steck SE, Fung TT, et al. Mediterranean diet, Dietary Approaches to Stop Hypertension (DASH) style diet, and metabolic health in U.S. adults. Clin Nutr. 2017;36(5):1301-1309.
6. Rebholz CM, Crews DC, Grams ME, et al. DASH (Dietary Approaches to Stop Hypertension) diet and risk of subsequent kidney disease. Am J Kidney Dis. 2016;68(6):853-861.
7. Salehi-Abargouei A, Maghsoudi Z, Shirani F, Azadbakht L. Effects of Dietary Approaches to Stop Hypertension (DASH)-style diet on fatal or nonfatal cardiovascular diseases — incidence: a systematic review and meta-analysis on observational prospective studies. Nutrition. 2013;29(4):611-618.
8. US Department of Health & Human Services. Dietary Guidelines for Americans 2015–2020: Eighth Edition. http://health.gov/dietaryguidelines/2015/guidelines/. Published January 7, 2016.
9. Mellen PB, Gao SK, Vitolins MZ, Goff DC, Jr. Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Arch Intern Med. 2008;168(3):308-314.
10. Kim H, Andrade FC. Diagnostic status of hypertension on the adherence to the Dietary Approaches to Stop Hypertension (DASH) diet. Prev Med Rep. 2016;4:525-531.
11. Henkin Y, Garber DW, Osterlund LC, Darnell BE. Saturated fats, cholesterol, and dietary compliance. Arch Intern Med. 1992;152(6):1167-1174.
12. Monsivais P, Scarborough P, Lloyd T, et al. Greater accordance with the Dietary Approaches to Stop Hypertension dietary pattern is associated with lower diet-related greenhouse gas production but higher dietary costs in the United Kingdom. Am J Clin Nutr. 2015;102(1):138-145.
13. Mackenbach JD, Burgoine T, Lakerveld J, et al. Accessibility and affordability of supermarkets: associations with the DASH diet. Am J Prev Med. 2017;53(1):55-62.


