Today’s Dietitian
Vol. 19, No. 11, P. 36
It’s an essential nutrient that’s underconsumed and underappreciated but so important to overall health.
In the world of nutrition, choline hardly is a household word. Having been identified as an essential nutrient by the US National Academies of Medicine Food and Nutrition Board only in 1998,1 choline remains under the radar of most consumers and many health care professionals. But with all of choline’s important roles, it may soon become the darling of the nutrition world.
Choline is important to development before birth and throughout the entire life cycle. Unfortunately, recent National Health and Nutrition Examination Survey data suggest that a mere 8% of adults meet or exceed the Adequate Intake (AI) for choline.2 Because few foods are good sources of this essential nutrient, supplements may be necessary.
Choline in the Body
Made by the body in small amounts, choline isn’t a true vitamin, as it doesn’t function as a coenzyme. Rather, it’s a vitaminlike compound that provides building material for several important compounds with diverse functions and interacts with folate and other nutrients. Along with endogenous sources, dietary choline is required to meet the long list of the body’s demands. Among its many roles, choline is needed for methyl donation, neurotransmitter synthesis, cell membrane signaling, and lipid transport.1,3 Most of the choline in the body exists as phosphatidylcholine, a phospholipid and essential structural component of cell membranes.
Moreover, choline is a precursor to acetylcholine, a neurotransmitter and nonneuronal cell signaling compound involved in muscle control, memory, mood, and other nervous system functions.3 As a major dietary source of methyl groups, choline plays a role in gene expression, cell membrane signaling, stabilization of DNA, homocysteine reduction, detoxification, and lipid transport and metabolism.1,2 Folate also is a major source of methyl groups, so folate status impacts choline requirements and vice versa. If one of these nutrients is low, the dietary requirement for the other is increased. Common genetic polymorphisms in folate and choline metabolizing genes alter the metabolic use of choline in ways that increase the demand for dietary choline.4
Requirements and Usual Intakes
Choline needs are influenced by stage of life, gender, ability to produce choline endogenously, and genetic variations, as well as the amount of folate and other nutrients in the diet.3 The Food and Nutrition Board found no research adequate to set an Estimated Average Requirement or Recommended Dietary Allowance. The AIs for choline for infants are based on the average intake from human breast milk.5 For other ages, the AI reflects the level necessary to prevent liver damage in adults (see Table 1 on page 39).
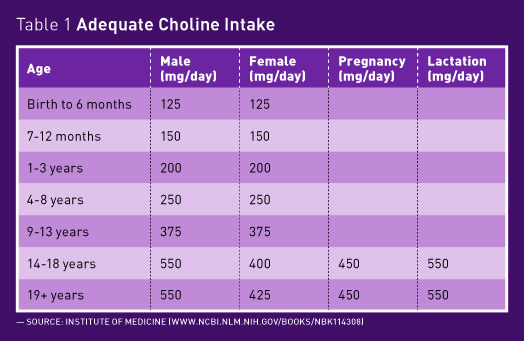
“Choline intakes are suboptimal,” says Taylor C. Wallace, PhD, CFS, FACN, a professor in the department of food and nutrition studies at George Mason University in Fairfax, Virginia, and principal at the Think Healthy Group, a consulting, advertising, and medical communications firm that serves the pharmaceutical, chemical, and agricultural industries across the Asian Pacific region in Sydney, Melbourne, Auckland, Singapore, Seoul, and Hong Kong. Research coconducted by Wallace finds that about 89% of Americans older than age 2 and almost 92% of pregnant women fail to consume adequate amounts of choline.2 In general, men are more likely to meet their age and gender-specific AI than women because they consume more food and calories. Children aged 9 and older are unlikely to consume enough choline, and teenagers between the ages of 14 and 18 are the least likely group to consume choline at or above the AI. The group most likely to meet their choline needs is children between the ages of 2 and 8, Wallace says, because this age group typically consumes considerable amounts of milk and eggs, which naturally supply choline, and they often consume choline-fortified processed foods while the other groups don’t.
Choline in the Diet
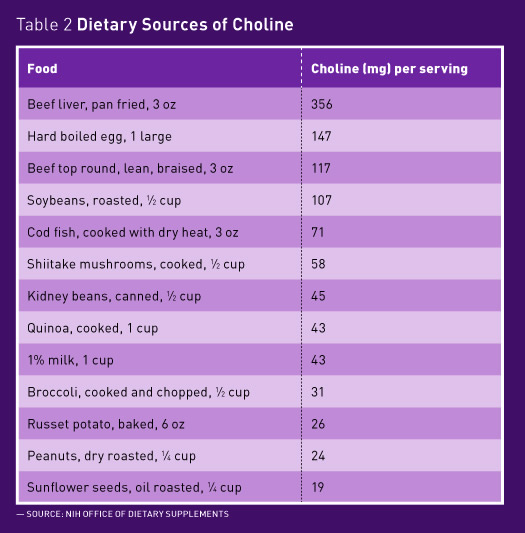
Though tiny amounts of choline are found in many foods, this nutrient is relatively scarce in the diet but is primarily found in eggs, liver, meats, seafood, and dairy. “If you’re vegetarian, you have a big problem. It’s almost completely impossible to get enough choline from plant foods alone,” Wallace says. The best vegetarian sources of naturally occurring choline are quinoa, nuts, potatoes, and some vegetables such as broccoli (see Table 2 on page 39).
Even a well-crafted diet likely is low in choline. The 2015–2020 Dietary Guidelines for Americans identify choline as an underconsumed nutrient.6 The USDA Food Patterns, as outlined in the Dietary Guidelines, offer dietary recommendations. An analysis found that the recommended amounts of each food group in the USDA Food Patterns met or came close to meeting almost all nutrient goals. However, adequacy goals weren’t met for choline, nor were they met for potassium, vitamin D, and vitamin E.6 This underscores the scarcity of choline in the food supply, Wallace says.
Choline and Health
Choline is essential for good health at all ages and stages of life, and it’s being studied for its association with desirable health outcomes.
Pregnancy and Lactation
In June, the American Medical Association announced its support for the addition of choline in all prenatal vitamins to ensure proper development of a baby’s brain and spinal cord.7 Currently, prenatal vitamins routinely provide 0 to 55 mg choline, though the AI during pregnancy is 450 mg per day.
“I was very pleased to learn of this recommendation,” says Marie Caudill, PhD, RD, a professor in the division of nutritional sciences at Cornell University in Ithaca, New York. “Like folate, choline is required for cellular division and methylation reactions, both of which are accelerated during human pregnancy. And choline is needed to make acetylcholine, phosphatidylcholine, and sphingomyelin, all of which play a critical role in brain development and function,” she adds. Though the mechanism is unclear, choline appears to be important for the prevention of neural tube defects.
Animal studies and some human studies support that prenatal choline supplementation improves brain development. According to Caudill, rodents born to mothers supplemented with choline show improved memory and learning compared with rodents of mothers that didn’t consume additional choline. In other animal studies, choline was associated with greater emotional regulation. Human infants born to supplemented moms showed better attention by blocking out unnecessary information. In Caudill’s own research, babies born to moms who consumed additional choline could more quickly process information, which was measured by tracking the infants’ eye movements toward visual stimuli in their peripheral vision.
Studies also have shown beneficial effects on biomarkers of placental development. Among women supplemented with choline in the last trimester of pregnancy, there was decreased production of a biomarker linked to poor placental health, Caudill says.
Even stress reactivity is reduced in neonates when their moms receive additional choline during the final trimester of pregnancy. Caudill explains that choline’s role as a methyl donor leads to decreased cortisol at birth. This demonstrates an important epigenetic effect, she adds.
Additional research in Caudill’s lab found that giving women of childbearing age supplemental choline along with DHA supplements enhanced red blood cell DHA content compared with women receiving DHA supplements alone. Theoretically, this would lead to greater incorporation of DHA in fetal neuronal tissue.
For lactation, the AI for choline is even higher than it is for pregnancy. Breast milk is rich in choline, underscoring the importance of this nutrient to the infant and the likelihood of depleted stores for the mom.
Muscle Function
Because choline is a precursor to acetylcholine and phosphatidylcholine, it plays a role in muscle cell communication and function, Wallace says. Thus, athletes likely have greater performance when choline stores are adequate, he adds.
Cardiovascular Health
Some population studies find that individuals with the highest dietary choline intakes are the most likely to have low levels of inflammation markers such as C-reactive protein.1 In theory, this could suggest a role of choline in the prevention of some chronic diseases related to inflammation, such as heart disease and some types of cancer.
In its role as a methyl donor, choline is involved in the conversion of the amino acid homocysteine to methionine. Though not known to be a causative factor, elevated levels of homocysteine are linked to a greater risk of CVD and other chronic conditions.
Recently, questions were raised about a potential role of choline in the development of CVD. For example, a small human study found that choline supplementation increased plasma levels of a metabolite studied as a possible atherogenic compound and led to increased platelet aggregation.8 Caudill explains that instead of being absorbed, some choline travels to the large intestine, where microbes can convert it to trimethylamine (TMA). TMA then travels to the liver where it becomes TMA N-oxide (TMAO). “In mouse models, TMAO exacerbates atherosclerosis,” Caudill explains. “And individuals at high risk of CVD tend to have higher levels of TMAO and greater risk of subsequent cardiovascular events.” This doesn’t prove that TMAO is a causative agent, she says. Instead, sicker individuals may have a different makeup of intestinal microbes resulting in higher TMAO levels. And they may have some renal impairment, which reduces the renal excretion of TMAO, leaving higher concentrations within the body. In addition, Caudill notes that fish, which is widely considered heart healthy, is one of the greatest sources of dietary TMAO.
A recent systematic review and meta-analysis found no association between dietary choline and incident CVD. One of two studies looking at phosphatidylcholine and CVD mortality found a positive association.9 Caudill suggests more studies are needed before recommendations are made to limit choline-containing foods, especially since intakes are already below AI levels. “Whether these risks are causal and for whom they are relevant requires further evidence from randomized controlled trials.”
Cognition in Adults
As the precursor to acetylcholine, choline is connected with cholinergic neural networks associated with memory. This relationship has scientists wondering whether choline plays a role in slowing cognitive decline in aging. Though research is limited, data from the Framingham Heart Study Offspring cohort find that higher choline intake is related to better memory performance.10
When Intakes Are Inadequate
Choline deficiency manifests as nonalcoholic fatty liver disease because choline is required for the synthesis of very low-density lipoprotein particles, which transport fat from the liver. Without adequate choline, liver fat accumulates, leading to steatosis and potentially to liver damage. Adults fed total parenteral nutrition devoid of choline but adequate in other nutrients developed fatty liver, which resolved when choline was administered.1 In a separate study, when adults were deprived of dietary choline, 80% of men and 77% of postmenopausal women developed fatty liver or muscle damage. Fewer premenopausal women developed signs of organ dysfunction, presumably because estrogen upregulates de novo synthesis of choline. Again, choline intake reversed signs of damage.11
Choline deficiency is rare among healthy nonpregnant individuals likely because of endogenous choline synthesis and because small amounts of choline are present in a variety of foods.3 When levels are suboptimal, choline from the kidneys, lungs, and intestines is redistributed to the liver and brain.1
While deficiency is rare, insufficiency is the norm, as Wallace’s data make clear. With all of choline’s roles, it makes sense that people will have better long-term outcomes if they consume adequate choline throughout their lives. Low intakes of choline may predispose an individual to early cognitive decline and other health problems, Wallace explains.
Improving choline status will require a multipronged approach. Since most people fail to meet the AI for choline and no subpopulation has exceeded the Upper Limit, Wallace supports a greater public health effort to encourage increased intake of choline from foods and supplements. Particularly, pregnant and lactating women will benefit from supplementation, he says. He also calls for additional research and review of the research by the National Academies of Medicine to set an Estimated Average Requirement and Recommended Dietary Allowance. Furthermore, educating dietitians, physicians, and other health care providers could spur a trickle-down effect to improve consumer awareness of choline and the nutrient’s vital roles in human health. In addition, Wallace sees a role for voluntary fortification of staple food products such as cereals and grains.
Counseling Clients
To help clients meet their choline needs, it’s important to carefully assess their eating patterns and unique situations, says Elizabeth Ward, MS, RD, author of Expect the Best: Your Guide to Healthy Eating, Before, During and After Pregnancy. With the critical need for choline during fetal development and infancy, choline-containing vitamins are important for pregnant and breast-feeding moms. “Right now, the choline levels in prenatal vitamins and other vitamins are variable,” Ward says. That may soon change because of the American Medical Association recommendation. Infant formula, too, should contain choline. The FDA requires that it be present in infant formulas, but the levels also may vary, Ward says. She advises parents to discuss their choice of formula with their infant’s pediatrician.
Consumers may soon find it easier to identify foods containing choline. The FDA recently set a DV of 550 mg for choline for anyone aged 4 and older. This opens the door for manufacturers to voluntarily label choline on the Nutrition Facts panel. Foods with at least 55 mg of choline per serving are considered good sources, and those with at least 110 mg of choline may be called excellent sources. Both consumers and dietitians will find the choline content of various foods in the USDA Food Composition Databases.
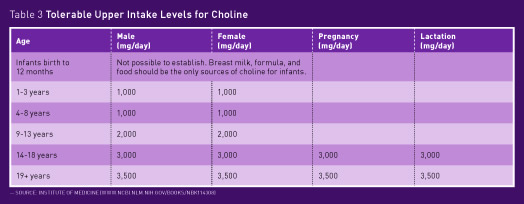
Excessive intakes of choline are associated with a fishy body odor, low blood pressure, liver toxicity, vomiting, and excessive sweating and salivation (see Table 3 on page XX).3
When discussing supplements with older clients and patients, Caudill encourages caution. It’s best to be conservative with older individuals since choline is involved in cellular division and could possibly accelerate an undiagnosed cancer. For now, aim to reach the AI with food, adding supplements only if necessary and only to the AI level, she says.
— Jill Weisenberger, MS, RDN, CDE, CHWC, FAND, is a freelance writer and a nutrition and diabetes consultant to the food industry, including Egg Nutrition Center, Omega-9 Oils, and Balchem Corporation, a supplier of choline and other nutritional ingredients. She has a private practice in Newport News, Virginia, and is the author of the bestselling Diabetes Weight Loss — Week by Week.
References
1. Zeisel SH, da Costa KA. Choline: an essential nutrient for public health. Nutr Rev. 2009;67(11):615-623.
2. Wallace TC, Fulgoni VL. Usual choline intakes are associated with egg and protein food consumption in the United States. Nutrients. 2017;9(8):839.
3. Choline: fact sheet for professionals. National Institutes of Health, Office of Dietary Supplements website. https://ods.od.nih.gov/factsheets/Choline-HealthProfessional/. Updated January 25, 2017. Accessed July 28, 2017.
4. Ganz AB, Cohen VV, Swersky CC, et al. Genetic variation in choline-metabolizing enzymes alters choline metabolism in young women consuming choline intakes meeting current recommendations. Int J Mol Sci. 2017;18(2):252.
5. Wallace TC, Fulgoni VL. Assessment of total choline intakes in the United States. J Am Coll Nutr. 2016;35(2):108-112.
6. US Department of Health & Human Services. Dietary Guidelines for Americans 2015–2020: Eighth Edition. http://health.gov/dietaryguidelines/2015/guidelines/. Published January 7, 2016.
7. Berg S. AMA backs global health experts in calling infertility a disease. AMA Wire website. https://wire.ama-assn.org/ama-news/ama-backs-global-health-experts-calling-infertility-disease. Published June 13, 2017. Accessed July 31, 2017.
8. Zhu W, Wang Z, Tang WHW, Hazen SL. Gut microbe-generated trimethylamine N-Oxide from dietary choline is prothrombotic in subjects. Circulation. 2017;135(17):1671-1673.
9. Meyer KA, Shea JW. Dietary choline and betaine and risk of CVD: a systematic review and meta-analysis of prospective studies. Nutrients. 2017;9(7):711.
10. Poly C, Massaro JM, Seshadri S, et al. The relation of dietary choline to cognitive performance and white-matter hyperintensity in the Framingham Offspring Cohort. Am J Clin Nutr. 2011;94(6):1584-1591.
11. Fischer LM, daCosta KA, Kwock L, et al. Sex and menopausal status influence human dietary requirements for the nutrient choline. Am J Clin Nutr. 2007;85(5):1275-1285.


