Today’s Dietitian
Vol. 19, No. 11, P. 32
As more children are diagnosed with type 2 diabetes, RDs and diabetes educators need to know how to effectively counsel them.
Over the past 10 years, the face of diabetes has changed dramatically. Type 2 diabetes—once thought of as an obese adult disease, is emerging rapidly in children and adolescents. According to a 2016 consensus report published in Diabetes Care, there are 5,000 new cases each year in the United States, and the prevalence increases with age, tripling from age 10 to 14 years to 15 to 18 years. Although diabetes rates in adult men and women are similar, adolescent girls have a 60% higher prevalence rate than boys.1
Even more troubling, the majority of new cases are among youth of minority racial and ethnic groups. Ethnic disparities also are apparent in death rates. Mortality rates of African American children with diabetes are more than twice as high as those for their white peers and more than three times higher than those for Hispanic children.2,3 It’s projected that by 2050 the prevalence of type 2 diabetes in youth will increase four-fold to more than 80,000.4 This article will describe the pathophysiology, risk factors, signs and symptoms, complications, and management of type 2 diabetes in youth and will provide strategies for diabetes educators counseling children with type 2 diabetes and their parents.
Obesity a Major Risk Factor
It’s been said that the 21st century is an unprecedented diabetogenic era in human history, and the number of children diagnosed with type 2 diabetes continues to soar exponentially.5
Compared with their normal-weight counterparts, children who are obese have a quadrupled risk of developing type 2 diabetes.6 Although childhood obesity, a major risk factor for type 2 diabetes, isn’t increasing in the United States, the prevalence of type 2 diabetes in children has increased three-fold. This prevalence is due in large part to the fact that the degree of obesity in affected children is increasing.7 Obese children are hyperinsulinemic; they have approximately 40% lower insulin-stimulated glucose metabolism than nonobese children.8
Childhood obesity rates are higher among minorities, and there’s evidence that African American children may have a genetic predisposition to insulin resistance, putting them at increased risk of type 2 diabetes. African American children aged 7 to 11 have significantly higher insulin levels than age-matched white children.8
Signs and Symptoms
Most children with type 2 diabetes are obese or extremely obese at diagnosis and present with glucose in the urine without ketones, no or mild polyuria and polydipsia, and little or no weight loss. Children with type 2 diabetes usually are diagnosed over the age of 10 in middle to late puberty. Increased growth hormone secretion during puberty contributes to insulin resistance and resulting high insulin levels.8
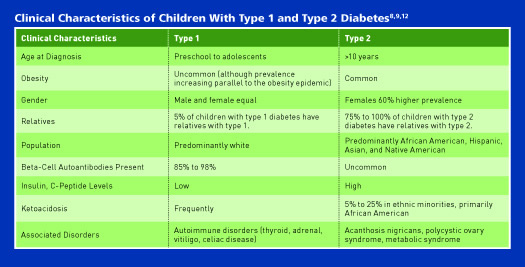
Distinguishing between type 1 and type 2 diabetes at diagnosis is important—although not always easy, because treatment regimens, educational approaches, dietary advice, and outcomes differ markedly between patients with the two diagnoses.9 Overweight and obesity are common in children with type 1 and type 2 diabetes. “Today, the challenge with determining type 1 and type 2 diabetes is that children with type 2 are generally very overweight or obese and have such severe insulin resistance. Some children present with a hemoglobin A1c of greater than 10% and the three P’s (polyuria, polydipsia, polyphagia), resulting in the need for insulin. These are the classic signs and symptoms of type 1 diabetes; however, after further testing with blood work, type 1 diabetes is ruled out,” says Kimberly Philbin, RD, CDN, a practice dietitian in the division of pediatric endocrinology at Cohen Children’s Medical Center in Lake Success, New York. Further testing may include fasting insulin levels, C-peptide, and insulin autoantibodies.8
Up to 33% of children in particular ethnic groups—primarily African Americans—have ketones in their urine at diagnosis, and 5% to 25% have ketoacidosis at diagnosis. It’s very rare for children with type 2 diabetes to present with a hyperglycemic hyperosmolar coma. These clinical features often delay the confirmation of the type of diabetes for months.8 Marina Chaparro, MPH, RDN, CDE, a clinical dietitian and national spokesperson for the Academy of Nutrition and Dietetics, says, “It is possible to see overweight kids with newly diagnosed type 1 diabetes and even with some clinical signs of insulin resistance, all due to the excess weight. Insulin antibodies should be assessed in all children upon diagnosis to determine the correct pathogenesis and provide appropriate treatment.”
Typical characteristics of type 2 diabetes include the following:8
• slow onset;
• overweight or obese patients from a minority group (Native Americans, African Americans, and Pacific Islanders);
• signs of insulin resistance (eg, acanthosis nigricans, hypertension, polycystic ovary syndrome [PCOS], dyslipidemia);
• retinopathy; and
• strong family history of type 2 diabetes.
Screening
The American Diabetes Association 2017 Standards of Medical Care in Diabetes recommend screening for prediabetes and type 2 diabetes in children who are overweight or obese and who have two or more of the following risk factors for diabetes:
• family history of type 2 diabetes in a first-degree or second-degree relative;
• minority race or ethnicity (eg, Native American, African American, Latino, Asian, or Pacific Islander);
• signs of insulin resistance or conditions associated with insulin resistance (eg, acanthosis nigricans, hypertension, dyslipidemia, PCOS, or small-for-gestational-age birth weight); and
• maternal history of diabetes or gestational diabetes during the child’s gestation.9
Screening should start at age 10 or at the onset of puberty, whichever is earlier. Subsequent screening should be performed every three years. A fasting plasma glucose test is the preferred screening study; if clinical suspicion is high but fasting blood glucose is normal (<100 mg/dL), an oral glucose tolerance test should be considered.9
Pathophysiology and Complications
Insulin resistance and nonautoimmune beta-cell failure are the hallmarks of type 2 diabetes in children and adults. However, children exhibit a rapidly progressive beta-cell decline and accelerated development of diabetes complications.1 “Children with type 2 diabetes are affected differently than adults with diabetes. Studies in children with type 2 diabetes point to a faster and more severe progression of diabetes-related complications,” Chaparro says.
The TODAY (Treatment Options for type 2 Diabetes in Adolescents and Youth) study showed the loss of glycemic control was three- to four-fold higher in adolescents and youth than rates observed in adults.1
Moreover, youth with type 2 diabetes experience diabetes complications at a greater rate than children with type 1 diabetes. “The earlier the onset, the earlier the complications. Some studies estimate that children with type 2 diabetes may develop some type of diabetes complication as early as age 21,” Chaparro says. In a study published in the February 2017 issue of the Journal of the American Medical Association, researchers examined how quickly and often youth developed signs of kidney, nerve, and eye diseases, which are among the most common diabetes complications. They also measured several risk factors for heart disease. Surprisingly, after having diabetes for less than eight years, at age 21 one in three patients with type 1 diabetes and almost three in four patients with type 2 diabetes had at least one of the following complications or comorbidities: diabetic kidney disease, retinopathy, peripheral neuropathy, arterial stiffness, or hypertension.10,11 (See table for more information about type 1 vs type 2 diabetes.)
It should be noted, most of the patients with type 2 diabetes in the study were African American (43%), followed by white (26%), Latino (21%), Native American (7%), or other (3%), and most were obese (72%) or overweight (18%). Most (41%) came from families in the lowest annual household income category (<$25,000 per year).11
Management
Generally, the treatment goals for youth with type 2 diabetes are the same as those for youth with type 1 diabetes, including blood glucose control and management of obesity, dyslipidemia, hypertension, and microvascular complications.9 The American Academy of Pediatrics Clinical Practice Guidelines for children with type 2 diabetes suggest that clinicians incorporate the Academy of Nutrition and Dietetics’ Pediatric Weight Management Evidence-Based Nutrition Practice Guidelines at the time of diagnosis and as part of ongoing management.12 (See andeal.org/topic.cfm?menu=5296&cat=5632 for the full practice guidelines.)
Pharmacotherapy for youth with type 2 diabetes is limited. “Unfortunately, there are limited therapeutic treatments for children with type 2 diabetes due to the lack of available clinical data in this population. Typically, insulin and metformin are the two medications used in children with diabetes,” Chaparro says.
However, new drugs such as dipeptidyl peptidase inhibitors or glucagonlike peptide-1 mimetics are in development for treatment of youth with type 2 diabetes.8
Type 2 diabetes has a disproportionate impact on youth of ethnic/racial minorities and from disadvantaged backgrounds; it also often occurs in complex psychosocial and cultural environments that make lasting lifestyle change difficult to achieve and adherence to medical recommendations a struggle.1 The following strategies can help improve outcomes in dietitians’ pediatric patients with type 2 diabetes:
• Dispel myths. Behavior change recommendations must take into account families’ health beliefs and behaviors. Often, parents of children diagnosed with type 2 diabetes have preconceived notions about diabetes—typically based on myths. Marla C. Solomon, RD, LDN, CDE, a dietitian and diabetes educator in pediatric endocrinology at the University of Illinois Hospital & Health Sciences System in Chicago, says, “A family’s understanding of the disease may impact a child with type 2 diabetes. Many people will say, ‘You have sugar,’ when referring to diabetes. They believe all you need to do is avoid sugar and diabetes will go away.”
• Treat the parent first. Chaparro suggests you shift the focus away from the child and onto the parent. “You treat the parent first, and then you treat the child. Parental obesity is a big predictor of kids being overweight, so it’s crucial to assess parent’s attitudes and perceptions of diabetes, obesity, and eating habits. Based on what we know, lifestyle modifications that only encompass diet and exercise have a very low success rate. It’s only until medications are introduced that some parents begin to think of diabetes as something serious. That being said, key aspects of the nutrition counseling involve individualization and constant follow-up,” Chaparro says.
• Make culturally appropriate recommendations. Solomon says, “As registered dietitians, we need to demonstrate how all cultural and heritage foods can fit into [the child’s] life with diabetes. Focus on the portion sizes, not elimination.” Solomon prefers to avoid the complexity of carbohydrate counting and uses MyPlate to focus on portion control.
• Involve the entire family. A family-centered approach to nutrition and lifestyle modification is essential for children with type 2 diabetes. Philbin says, “When dealing with children, the whole family must be involved and willing to make behavior changes; otherwise, the goals you set with them will not be effective. The parents and older siblings, if any, must act as healthy role models for the child.”
• Avoid labeling food. “As some people use the word ‘bad’ when describing a child’s actions, they also will use the word ‘bad’ when talking about food. We want food and nutrition to be positively presented so that no other family member will blame the child with diabetes for taking away their favorite items. This prevents the child with diabetes from feeling different. In this world, we want all children to be included vs excluded, even with diabetes,” Solomon says. There are no foods that are off limits. Parents should be taught to monitor how different foods affect their child’s blood glucose. They may need to decrease portions or redistribute carbohydrate foods to keep blood glucose in the child’s target range.
• Be sensitive to family resources. Most children with type 2 diabetes are from ethnic minority groups and families in the lowest annual household income category.11 “There are many psychosocial challenges in children with type 2 diabetes, including home environment, single parenting, juggling work and home life, limited safe areas for exercise, and food deserts. Also, many African American women, and even men, will accept a larger body image even though it’s a risk factor for diabetes, as they say, ‘It runs in the family,'” Solomon says. Lifestyle intervention strategies must take into account the family psychosocial challenges.
Future Directions
The face of type 2 diabetes will continue to change. As mentioned, it’s projected that by 2050 the prevalence of type 2 diabetes in youth will increase four-fold. The increasing number of children with type 2 diabetes will present unique challenges for health care providers who care for them. A disproportionate number of children diagnosed with type 2 diabetes are of ethnic/racial minorities and from disadvantaged backgrounds, making sustained lifestyle change and medical adherence extremely difficult. Nutrition professionals who desire to work with this population must be skilled in behavior modification techniques for adults and children, culturally competent, and knowledgeable about food insecurity.
— Constance Brown-Riggs, MSEd, RD, CDE, CDN, is a member of the board of directors for the American Association of Diabetes Educators; a past national spokesperson for the Academy of Nutrition and Dietetics, specializing in African American nutrition; and author of The African American Guide to Living Well With Diabetes and Eating Soulfully and Healthfully With Diabetes. Her latest book, Diabetes Guide to Enjoying Foods of the World, was published in September 2017 by the Academy of Nutrition and Dietetics.
References
1. Nadeau KJ, Anderson BJ, Berg EG, et al. Youth-onset type 2 diabetes consensus report: current status, challenges, and priorities. Diabetes Care. 2016;39(9):1635-1642.
2. Phillips D. Black children more likely to die from diabetes. Medscape website. http://www.medscape.com/viewarticle/880377. Published May 22, 2017. Accessed May 30, 2017.
3. Mayer-Davis EJ, Lawrence JM, Dabelea D, et al. Incidence trends of type 1 and type 2 diabetes among youths, 2002-2012. N Engl J Med. 2017;376(15):1419-1429.
4. Imperatore G, Boyle JP, Thompson TJ, et al. Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care. 2012;35(12):2515-2520.
5. Farag YM, Gaballa MR. Diabesity: an overview of a rising epidemic. Nephrol Dial Transplant. 2011;26(1):28-35.
6. Obesity in children quadruples their risk of type 2 diabetes. Medscape website. http://www.medscape.com/viewarticle/879125. Published April 26, 2017. Accessed May 30, 2017.
7. Childhood obesity facts. Centers for Disease Control and Prevention website. https://www.cdc.gov/obesity/data/childhood.html. Updated April 10, 2017. Accessed May 30, 2017.
8. Reinehr T. Type 2 diabetes mellitus in children and adolescents. World J Diabetes. 2013;4(6):270-281.
9. American Diabetes Association. American Diabetes Association Standards of Medical Care in Diabetes — 2017. Diabetes Care. 2017;40(Suppl 1):S1-S135.
10. Youth with type 2 diabetes develop complications more often than type 1 peers. US Department of Health & Human Services, National Institutes of Health website. https://www.nih.gov/news-events/news-releases/youth-type-2-diabetes-develop-complications-more-often-type-1-peers. Published February 28, 2017. Accessed June 1, 2017.
11. Busko M. 72% of youth with type 2 diabetes have complications. Medscape website. http://www.medscape.com/viewarticle/876399. Published February 28, 2017. Accessed June 1, 2017.
12. Copeland KC, Silverstein J, Moore KR, et al. Management of newly diagnosed type 2 diabetes mellitus (T2DM) in children and adolescents. Pediatrics. 2013;131(2):364-382.