Today’s Dietitian
Vol. 18, No. 10, P. 48
Research shows a diet rich in anti-inflammatory compounds can prevent and even slow disease progression.
According to the Centers for Disease Control and Prevention (CDC), osteoarthritis (OA), also known as degenerative joint disease, affects one-third of adults aged 65 and older, making it the most common form of arthritis. It’s also one of the leading causes of disability. It’s projected that OA will affect more than 67 million Americans by the year 2030.1 OA can affect any joint, but it occurs most often in the knees, hips, lower back, neck, the small joints of the fingers, and at the base of the thumb and big toe. Not only does OA cause pain and disability, but the CDC also found death rates among adults with OA to be 1.6 times greater compared with the general population.
The pathogenesis of osteoarthritis isn’t completely understood, but according to the Arthritis Foundation, once degeneration of cartilage occurs in the joints, bone can break down, triggering an inflammatory response that causes further damage. While inflammation most often is associated with rheumatoid arthritis (RA), recent research indicates that systemic inflammation may not only worsen existing OA; it may also contribute to its development.
Inflammation has long been identified as the result of injury or illness. Acute inflammation is easy to recognize, as it manifests as redness, swelling, and fever, all easy-to-spot signs of a healthy immune response triggered by a well-regulated release of immune cells and chemicals designed to heal wounds and fight bacterial and viral infections. Chronic inflammation, however, can last for years, and it often goes undetected as it spreads throughout the body with no outward signs, damaging organs and causing disease. Like acute inflammation, chronic inflammation is the result of an immune response. When exposure to any immune system trigger is constant, it works overtime and the components of inflammation designed to destroy microbes can end up injuring normal tissue, including joints. This constant exposure, such as a proinflammatory diet, and the body’s destructive reactions, can result in or aggravate disease—in this case, OA.
Obesity often is cited as a risk factor for OA, especially on load-bearing joints, such as the knee. However, researchers are beginning to understand that it may not be just obesity itself, but systemic factors that often go along with obesity as well, such as chronic systemic inflammation or insulin resistance that can contribute to the initiation and progression of joint deterioration that leads to and aggravates OA.2 The inflammatory process is known to be associated with excessive fat tissue and poses a potential risk of chronic disease.3 In obesity, fat cells churn out inflammatory proteins called cytokines. The end result, regardless of the trigger, is a constant trickle of immune cells that interferes with the body’s healthy tissues, causing chronic pain. Proinflammatory cytokines include interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor alpha (TNF-alpha). Elevated levels of any of these proinflammatory cytokines in the blood are an indication of inflammation and/or disease. Transforming growth factor beta and IL-10 oppose the action of the proinflammatory cytokines and promote healing.
Data from the Third National Health and Nutrition Examination Survey demonstrated that all of the factors associated with metabolic syndrome—abdominal obesity, hyperglycemia, hypertension, and low levels of HDL cholesterol—were more common among people with OA.4 Full metabolic syndrome was more common among subjects with OA, regardless of sex or race.
“Obesity is the main factor that seems to provoke inflammation,” says Britt Burton-Freeman, PhD, an associate professor of food science and nutrition at the Illinois Institute of Technology. “We see that diets, or even single meals, high in calories, fat, and readily available carbohydrates induce an acute inflammatory response.” Obesity-induced chronic inflammation is a key component in the development of insulin resistance.5 A recent laboratory study using synovial tissue (the soft connective tissue that constitutes the membranes surrounding joints) from mice and individuals with type 2 diabetes suggested that the insulin resistance of type 2 diabetes may promote OA.2
Dietary Associations
Research also has shown that diet plays a key role in the regulation of inflammation.6 Diet can affect levels of C-reactive protein (CRP) in the blood, a compound often used as a marker for inflammation. Because there appears to be a relationship between inflammation and the development and progression not only of RA, but now OA, consuming diets shown to have anti-inflammatory effects may be an important step in preventing and halting the progression of the disease.
Inflammatory Diets
Dietary patterns high in refined starches, sugar, and saturated and trans fats are likely to trigger the release of proinflammatory cytokines and reduce production of anti-inflammatory cytokines. “The ‘standard American diet’ is definitely an example of a proinflammatory diet,” says Michelle Babb, MS, RD, a Seattle-based nutrition and lifestyle educator and author of Anti-Inflammatory Eating Made Easy. “A number of my patients have been able to discontinue use of nonsteroidal anti-inflammatory drugs by making dietary changes and sometimes supplementing with fish oil.” The fatty acid, arachidonic acid, is a precursor to proinflammatory prostaglandins and leukotrienes. Western diets, characterized by a high intake of red meat, refined sugars, saturated fat, and little fiber, are high in arachidonic acid mainly from animal products such as red meat, hard cheeses, and eggs.7
Studies have found an association between the intake of sugar sweetened beverages, but not diet soft drinks, and RA.8-10 While no one has looked at a possible association between sugar-sweetened beverages and OA, if consumption contributes to inflammation, as suggested, it likely would impact the risk and severity of OA as well.
Consumption of trans fats, which are found in many processed foods, including cakes, cookies, pie crusts, biscuits, stick margarine, and commercially fried foods, also have been found to increase biomarkers of inflammation, including CRP and IL-6, especially in people who are overweight.11,12
Anti-Inflammatory Diets
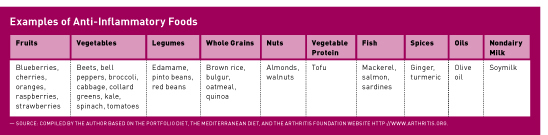
Dietary patterns rich in natural antioxidants and fiber from fruits, vegetables, and whole grains are likely to reduce inflammation.6 Whole food, plant-based diets are low in inflammation-inducing arachidonic acid and therefore are less likely to induce inflammation.7,13 One study, using an inflammatory food index, found that an anti-inflammatory diet consisting of foods rich in fish, fruits and vegetables, and olive oil was associated with lower levels of CRP.14 The omega-3 fatty acids found mainly in foods such as walnuts, sardines, salmon, and ground flaxseeds have long been recognized for their anti-inflammatory power.15-18
The Portfolio Diet
The Portfolio diet, a dietary pattern developed by David Jenkins, MD, PhD, DSc, at the University of Toronto, which focuses on nuts, viscous fiber, soy protein, and plant sterols, has been found to reduce markers of inflammation in the blood. In addition, each key component of the diet has been found individually to have a beneficial effect on inflammation via genistein in soy, sterols in wheat germ, and ellagic acid in walnuts, among others.
Nuts contain several components such as fiber, magnesium, L-arginine, antioxidants, and alpha-linolenic acid (ALA), which the body converts to omega-3s (walnuts are richest in ALA) that help reduce inflammation.19 Soluble fiber, like that in oatmeal, barley, psyllium, or okra, has been shown to reduce CRP.20
Moreover, several studies have found that high total fiber intakes result in lower levels of several markers of inflammation.21-24 The isoflavones found in soy have been shown to significantly reduce CRP in postmenopausal women, especially among those whose levels were elevated.25,26 According to the Arthritis Foundation, omega-3s are converted in the body into powerful anti-inflammatory compounds, called resolvins and protectins, and inhibit the synthesis of proinflammatory cells, such as TNF-alpha, IL-1, and IL-2.6
By putting all of these foods and compounds together, the Portfolio diet plan has been found to be as effective as statin drugs (usually prescribed to lower cholesterol) for reducing CRP levels in the blood.27 One study also showed that eating according to the Portfolio plan and substituting monounsaturated fats, in the form of sunflower oil and avocados, for saturated and trans fats over four weeks, reduced CRP levels an impressive 76% compared with people eating the conventional Portfolio plan.28 Olive oil is rich in oleocanthal, which has been shown to have anti-inflammatory effects.29
The Mediterranean Diet
The Mediterranean diet, which is characterized by a large amount of fruits and vegetables, whole grains, legumes, and olive oil, and includes fish and poultry over red meat, as well as red wine in moderation, also has been found to have an anti-inflammatory effect and it has been suggested that it could play a role in the prevention of OA, especially during early stages of the disease.30
The DASH Diet
The DASH (Dietary Approaches to Stop Hypertension) diet was designed to lower blood pressure, but research has found that following the diet can decrease markers of inflammation.31-33 The diet is rich in fruits, vegetables, whole grains, fat-free or low-fat dairy products, fish, poultry, beans, nuts, and vegetable oils and limits sugar-sweetened beverages, sweets, and foods high in saturated fats. The Arthritis Foundation includes the DASH diet in its list of recommended diets for arthritis.
A Plant-Based Diet
While several studies have examined the effects of vegetarian diets on the symptoms of RA and found them in general to be beneficial for pain and stiffness,34-36 only one study was found that examined the effects of a plant-based diet on OA in a six-week randomized trial.7 The group consuming the vegetarian diet reported significant improvement in energy level, pain, and physical functioning compared with the control group.
Practice Recommendations
So what should dietitians recommend to clients and patients to help them reduce inflammation and the disease risk that goes along with it? “We have no reason at this point to believe we have different anti-inflammatory diets. If you eat for your heart, you’re eating for your brain, your eyes, and your lungs. And we can add joints in this lineup as well,” Burton-Freeman says. It’s the same dietary recommendations dietitians would give to reduce the risk of cardiovascular disease, cancer, high blood pressure, or overweight: Eat a diet rich in fruits, vegetables, whole grains, beans, legumes, nuts, soy, and olive oil, and avoid foods high in saturated and trans fats.
— Densie Webb, PhD, RD, is a freelance writer, editor, and industry consultant based in Austin, Texas.
References
1. Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2006;54(1):226-229.
2. Hamada D, Maynard R, Schott E, et al. Suppressive effects of insulin on tumor necrosis factor-dependent early osteoarthritic changes associated with obesity and type 2 diabetes mellitus. Arthritis Rheumatol. 2016;68(6):1392-1402.
3. Lottenberg AM, Fan PL, Buonacorso V. Effects of dietary fiber intake on inflammation in chronic diseases. Einstein (Sao Paulo). 2010;8(2):254-258.
4. Peunpatom RA, Victor TW. Increased prevalence of metabolic syndrome in individuals with osteoarthritis: an analysis of NHANES III data. Postgrad Med. 2009;121(6):9-20.
5. de Luca C, Olefsky JM. Inflammation and insulin resistance. FEBS Lett. 2008;582(1):97-105.
6. Giugliano D, Ceriello A, Esposito K. The effects of diet on inflammation: emphasis on the metabolic syndrome. J Am Coll Cardiol. 2006;48(4):677-685.
7. Clinton CM, O’Brien S, Law J, Renier CM, Wendt MR. Whole-foods, plant-based diet alleviates the symptoms of osteoarthritis. Arthritis. 2015;2015:708152.
8. Hu Y, Costenbader KH, Gao X, et al. Sugar-sweetened soda consumption and risk of developing rheumatoid arthritis in women. Am J Clin Nutr. 2014;100(3):959-967.
9. Lu B, Ahmad O, Zhang FF, et al. Soft drink intake and progression of radiographic knee osteoarthritis: data from the osteoarthritis initiative. BMJ Open. 2013;3(7):e002993.
10. DeChristopher LR, Uribarri J, Tucker KL. Intake of high-fructose corn syrup sweetened soft drinks, fruit drinks and apple juice is associated with prevalent arthritis in US adults, aged 20-30 years. Nutr Diabetes. 2016;6:e199.
11. Mozaffarian D, Pischon T, Hankinson SE, et al. Dietary intake of trans fatty acids and systemic inflammation in women. Am J Clin Nutr. 2004;79(4):606-612.
12. Lopez-Garcia E, Schulze MB, Meigs JB, et al. Consumption of trans fatty acids is related to plasma biomarkers of inflammation and endothelial dysfunction. J Nutr. 2005;135(3):562-566.
13. Adam O, Beringer C, Kless T, et al. Anti-inflammatory effects of a low arachidonic acid diet and fish oil in patients with rheumatoid arthritis. Rheumatol Int. 2003;23(1):27-36.
14. Cavicchia PP, Steck SE, Hurley TG, et al. A new dietary inflammatory index predicts interval changes in serum high-sensitivity C-reactive protein. J Nutr. 2009;139(12):2365-2372.
15. Lopez-Garcia E, Schulze MB, Manson JE, et al. Consumption of (n-3) fatty acids is related to plasma biomarkers of inflammation and endothelial activation in women. J Nutr. 2004;134(7):1806-1811.
16. Lorente-Cebrián S, Costa AG, Navas-Carretero S, et al. An update on the role of omega-3 fatty acids on inflammatory and degenerative diseases. J Physiol Biochem. 2015;71(2):341-349.
17. Moro K, Nagahashi M, Ramanathan R, Takabe K, Wakai T. Resolvins and omega three polyunsaturated fatty acids: clinical implications in inflammatory diseases and cancer. World J Clin Cases. 2016;4(7):155-164.
18. Souza PR, Norling LV. Implications for eicosapentaenoic acid- and docosahexaenoic acid-derived resolvins as therapeutics for arthritis. Eur J Pharmacol. 2016;785:165-173.
19. Salas-Salvadó J, Casas-Agustench P, Murphy MM, López-Uriarte P, Bulló M. The effect of nuts on inflammation. Asia Pac J Clin Nutr. 2008;17(Suppl 1):333-336.
20. Ma Y, Griffith JA, Chasan-Taber L, et al. Association between dietary fiber and serum C-reactive protein. Am J Clin Nutr. 2006;83(4):760-766.
21. Ajani UA, Ford ES, Mokdad AH. Dietary fiber and C-reactive protein: findings from national health and nutrition examination survey data. J Nutr. 2004;134(5):1181-1185.
22. Delzenne NM, Cani PD. A place for dietary fibre in the management of the metabolic syndrome. Curr Opin Clin Nutr Metab Care. 2005;8(6):636-640.
23. Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J Am Coll Surg. 2008;207(6):928-934.
24. King DE, Egan BM, Woolson RF, Mainous AG 3rd, Al-Solaiman Y, Jesri A. Effect of a high-fiber diet vs a fiber-supplemented diet on C-reactive protein level. Arch Intern Med. 2007;167(5):502-506.
25. Hall WL, Vafeiadou K, Hallund J, et al. Soy-isoflavone-enriched foods and inflammatory biomarkers of cardiovascular disease risk in postmenopausal women: interactions with genotype and equol production. Am J Clin Nutr. 2005;82(6):1365-1366.
26. Dong JY, Wang P, He K, Qin LQ. Effect of soy soflavones on circulating C-reactive protein in postmenopausal women: meta-analysis of randomized controlled trials. Menopause. 2011;18(11):1256-1262.
27. Jenkins DJ, Kendall CW, Marchie A, et al. Direct comparison of dietary portfolio vs statin on C-reactive protein. Eur J Clin Nutr. 2005;59(7):851-860.
28. Jenkins DJA, Chiavaroli L, Wong JM, et al. Adding monounsaturated fatty acids to a dietary portfolio of cholesterol-lowering foods in hypercholesterolemia. CMAJ. 2010;182(18):1961-1967.
29. Parkinson L, Keast R. Oleocanthal, a phenolic derived from virgin olive oil: a review of the beneficial effects on inflammatory disease. Int J Mol Sci. 2014;15(7):12323-12334.
30. Oliviero F, Spinella P, Fiocco U, Ramonda R, Sfriso P, Punzi L. How the Mediterranean diet and some of its components modulate inflammatory pathways in arthritis. Swiss Med Wkly. 2015;145:w14190.
31. Saneei P, Hashemipour M, Kelishadi R, Esmaillzadeh A. The Dietary Approaches to Stop Hypertension (DASH) diet affects inflammation in childhood metabolic syndrome: a randomized cross-over clinical trial. Ann Nutr Metab. 2014;64(1):20-27.
32. Azadbakht L, Surkan PJ, Esmaillzadeh A, Willett WC. The Dietary Approaches to Stop Hypertension eating plan affects C-reactive protein, coagulation abnormalities, and hepatic function tests among type 2 diabetic patients. J Nutr. 2011;141(6):1083-1088.
33. Asemi Z, Esmaillzadeh A. DASH diet, insulin resistance, and serum hs-CRP in polycystic ovary syndrome: a randomized controlled clinical trial. Horm Metab Res. 2015;47(3):232-238.
34. Hafström I, Ringertz B, Spångberg A, et al. A vegan diet free of gluten improves the signs and symptoms of rheumatoid arthritis: the effects on arthritis correlate with a reduction in antibodies to food antigens. Rheumatology (Oxford). 2001;40(10):1175-1179.
35. McDougall J, Bruce B, Spiller G, Westerdahl J, McDougall M. Effects of a very low-fat, vegan diet in subjects with rheumatoid arthritis. J Altern Complement Med. 2002;8(1):71-75.36. Kjeldsen-Kragh J. Rheumatoid arthritis treated with vegetarian diets. Am J Clin Nutr. 1999;70(3 Suppl):594S-600S.


