 September 2017 Issue
September 2017 Issue
CPE Monthly: Assessing and Monitoring Body Composition — Learn About Different Methods of Monitoring Body Composition for Weight Management Throughout the Life Cycle and How to Apply Them to a Variety of Patient Care Settings
By Cassie Vanderwall, MS, RD, CD, CDE, CPT
Today's Dietitian
Vol. 19, No. 9, P. 50
Suggested CDR Learning Codes: 3080, 3090, 4060, 5370
Suggested CDR Performance Indicators: 8.3.6, 10.1.1, 10.2.1, 10.2.2
CPE Level 2
Take this course and earn 2 CEUs on our Continuing Education Learning Library
When it comes to overall health, a person's weight isn't nearly as important as the composition of the weight.
Body composition evaluation should involve use of the most appropriate, accurate, and accessible strategy available to clinicians to estimate an individual's adiposity, musculature, and body habitus. The composition of an individual's weight is important on two fronts. The consequences of overnutrition/obesity, including hypertension, insulin resistance leading to type 2 diabetes mellitus, cardiovascular disease, cerebrovascular disease, and other weight-related comorbidities are well known. There are also, of course, consequences to undernutrition/inadequate body fat, including malnutrition and disruption of the endocrine system, such as that seen in the female athlete triad.1-9
Accurate estimation of lean body mass and fat mass are critical components of the nutrition assessment and key determinants of a client's overall health and well-being. The RD's evidence-based practice requires knowledge and skills for determining the most appropriate strategies for nutrition assessment, including estimation of body composition. The body composition variables—lean body mass, bone mass, fat mass, and body fat percentage—will influence energy estimation and the RD's individualized intervention and, thus, affect the client's nutrition-related health outcomes.
This continuing education course compares and contrasts BMI with a variety of strategies for measuring body composition as it relates to weight management throughout the life cycle and provides recommendations and strategies for RDs to apply this information to a variety of patient care settings.
Body Composition Basics
The most prevalent body composition estimation strategy is known as the two-compartment model, which views the body as having two parts: fat and fat-free compartments.10,11 The fat compartment is composed of fat mass, whereas the fat-free compartment consists of not only lean body mass but also 2% to 8% lipid, based on gender.12 Body fat percentage can be calculated by dividing fat mass by total body weight.
Excessive body fat, or obesity, is characterized by greater than 25% body fat in males and 32% in females.13 Obesity is associated with a host of short- and long-term morbidities including cardiovascular and cerebrovascular diseases, hypertension, insulin resistance and type 2 diabetes, asthma, obstructive sleep apnea, psychosocial problems, decreased quality of life, and, in children and adolescents, an increased likelihood of becoming obese adults.1-7 Likewise, having inadequate body fat and scant lean body mass also is associated with acute and chronic disease. Essential body fat is present in bone marrow, major organ systems, and cellular membranes; the loss of this fat will result in compromised physiological function of the cardiovascular, endocrine, reproductive, skeletal, gastrointestinal, renal, and nervous systems.8,9
Essential body fat is estimated to be about 2% to 5% for males and 10% to 13% for females, as indicated in Table 1 on page 51.
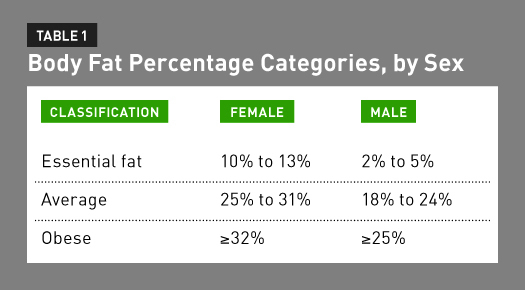
Stored fat, which is different from essential body fat, accumulates due to excess energy. Both types of body fat are vital to good health; healthful ranges of body fat are 12% to 24% for males and 25% to 31% for females. Women require higher levels of both types of fat to maintain reproductive function.8 When total body fat falls below the minimum recommended levels of essential body fat, the body can't effectively deliver key macro- and micronutrients to organs, resulting in deficiencies and electrolyte imbalances. This increases the risk of fracture, sarcopenia, damage to the heart muscle, poor growth, and even death.8,9
Accurate body composition assessment is critical considering the impact of having too little or too much body fat. Directly assessing the composition of an individual's body weight, or his or her body fat, is a key strategy for preventive and therapeutic intervention for the aforementioned disease states.14
BMI
BMI, formally known as the Quetelet Index, was first described in 1832 by Adolphe Quetelet, a Belgian statistician who applied mathematical science to his studies related to human physicality. His cross-sectional studies of human growth led him to conclude that weight increases as the square of the height.15 Quetelet's observation resulted in the commonly known BMI equation: dividing individuals' weight (in kilograms) by their height (in meters) squared. BMI is highly correlated with adult weight, independent of height.16

Obesity also is described using BMI ranges.17 For children and adolescents aged 2 to 19, BMI is plotted on the gender-specific Centers for Disease Control and Prevention growth chart to identify the BMI-for-age percentile. Normal weight for a child and adolescent is a BMI-for-age range between the 5th and the 85th percentiles, as indicated in Table 2 on page 52.
Childhood obesity is defined as a BMI at or above the 95th percentile on the BMI-for-age growth chart. This definition of obesity is calculated based on a reference population and, therefore, BMI doesn't directly measure adiposity.18 In adults, BMI is calculated using the aforementioned equation. A normal BMI is 18.5 to 24.9, and obesity is classified by a BMI greater than 30, as seen in Table 2.
There's evidence that BMI calculations correlate with direct measures of body fat mass, including skinfold thickness, bioelectrical impedance analysis (BIA), densitometry, dual-energy X-ray absorptiometry (DXA), air displacement plethysmography (ADP), and hydrodensitometry (underwater weighing).19-21 The indirect relationship between BMI and adiposity has been established but varies according to gender, age, and race/ethnicity.22,23 These variations are due to differences in hormones between the sexes (estrogen vs testosterone), resulting in greater degrees of fat mass in women vs men, metabolism throughout the life cycle (decrease in the metabolic rate with age), and genetics. Furthermore, BMI levels correlate with risk of weight-related morbidities and mortality.24,25 The vast adoption and use of BMI over several decades are a strength of this simple surrogate measure of body fat and are responsible for the increase in research literature and public health data related to obesity and chronic disease.18
BMI may be a suitable screening tool and may be ideal for many clinical situations due to its ease of use; however, it may be an inappropriate diagnostic tool as well as a poor strategy for measuring and monitoring changes in body composition over time.26,27 Therefore, understanding the limitations of BMI and the advantages of using other body composition strategies to measure changes in body fat and lean mass over time extends the RD's toolkit.
Limitations of BMI
The limitations of BMI can be summarized by its lack of sensitivity and specificity. The accuracy of BMI is questionable when comparing weight classifications in a racially diverse population. There's increasing evidence that BMI classifications are outdated because they don't account for the variety of patient populations that differ according to gender, age, and race/ethnicity.28 It's also necessary to exercise caution when comparing BMI across race-ethnicity groups due to variations in body composition and location of adiposity.29 BMI also maintains a weak relationship with percent body fat and doesn't distinguish the components of total weight. Direct measurements of total percent body fat provide a better tool for classifying overweight and obesity.29 In fact, BMI is positively associated with body fat mass, but the correlation between BMI and percent body fat is tenuous.30,31 Therefore, BMI is more closely linked with the weight of adiposity vs the percentage. However, total body fat mass isn't indicative of relative fat or obesity.
Consider an athlete vs a sedentary adult. Both individuals may be the same age and sex and both also may have the same fat mass, but it's likely that the athlete has greater muscle mass and thus a smaller percentage of body fat. Therefore, BMI may classify people as obese or nonobese incorrectly; this is especially true of men who generally maintain more muscle mass than women.32
These limitations can be summarized by BMI's inability to distinguish between fat and fat-free mass in both pediatric and adult populations.32,33 Total fat mass doesn't identify an individual's relative fat, or the amount of fat in relation to their bone, muscle, and total body mass.
As stated earlier, BMI is the product of individuals' weight in kilograms divided by the square of their height in meters. Therefore, total fat would be expected to highly correlate with BMI because weight is the numerator in the BMI formula. Mathematically, a heavier individual will have a higher fat mass than a lighter individual with the same percent body fat. Specifically, the utility of BMI is limited in older adults, men, highly trained athletes, overweight children (BMI-for-age percentile between the 86th and 95th), and underweight children.18
A client's percent body fat is an indicator of overall health. As noted previously, individuals with body fat percentages below those that are essential for health can experience morbidities and mortality comparable to those experienced by individuals with high body fat percentages. Despite these limitations, health care professionals continue to use BMI as a screening tool for overweight and obesity based on the assumption that a high BMI equals excessive adiposity. However, the literature doesn't support the use of BMI as a diagnostic tool for body fatness in the general population.28,29
Therefore, BMI should serve as an initial screening tool for weight and weight-related disease but should be integrated with other components of a thorough health assessment, including a client's medical, family, biochemical, dietary, and exercise histories, as well as the composition of their weight. Accurate measurement of body composition can be a valuable tool for preventing, managing, and treating both acute and chronic disease states in pediatric and adult populations. Therefore, it's essential for RDs to know which assessment strategies best fit their practices, and all health care practitioners can benefit from a more valid tool than BMI to screen for excess fat mass relative to total body weight.
Assessment Strategies
Following are the most common clinical assessment strategies for directly evaluating body composition with the greatest evidence to validate their use in both pediatric and adult populations. These include the skinfold method, BIA, hydrodensitometry, ADP, and DXA. The methods are compared below and on the following pages based on their utility in accurately measuring body composition as well as their feasibility in terms of clinician use and cost.
Skinfold Method
The skinfold method is quick, inexpensive, and easily performed. It estimates body composition based on skinfold thickness via equations validated by Jackson and Pollock in 1985, as listed below. These skinfold estimation equations are preferred and highly used in the industry.34 The four-site skinfold equations are unique for males and females but use the same variables: sum of the four skinfolds in millimeters and age in years.
Calipers are used to measure skinfold thickness at three to seven sites on the bodies of males and females to calculate body density or percent body fat. Ideally, skinfolds are measured on the abdomen, triceps, thigh, and suprailiac in millimeters in both males and females. The percentage of total body fat also can be derived from the body's density.
Hydrodensitometry and ADP, which will be discussed later, both use body density equations to estimate body fat percentages. The gold standard equations—the Jackson and Pollock equations—use a client's age, gender, race/ethnicity, and physical activity to calculate the most precise value.34 The following predictive equations have been validated in athlete and nonathlete populations to promote precision:
4-Site Skinfold Equation for Males:
Body fat (%) = (0.29288 X sum of skinfolds, mm) – (0.0005 X sum of skinfolds, mm squared) + (0.15845 X age, years) – 5.76377
4-Site Skinfold Equation for Females:
Body fat (%) = (0.29669 X sum of skinfolds, mm) – (0.00043 X sum of skinfolds, mm squared) + (0.02963 X age, years) + 1.4072
The accuracy of the skinfold method also depends on the technician's skill, standardized procedures, the type of calipers used, and the clients' hydration status.35 The quality of calipers varies; plastic calipers have less pressure, varied pressure throughout the range of measurement, and a smaller measurement scale than do higher quality calipers.3 In addition, hydration affects the compression of the adipose tissue, so it's important to keep hydration status stable from measurement to measurement. Exercise also influences hydration and can increase accumulation of water in adipose tissue. Therefore, skinfolds shouldn't be measured immediately following exercise. The skinfold method may not be satisfactory for measuring body composition in the morbidly obese or very muscular clientele. It's vital, however, that skinfold technicians practice with precision in mind and adhere to standardized measurement procedures. If this isn't possible, an alternative strategy for assessing body composition is indicated.
BIA
BIA is widely used and allows for determination of fat-free mass and total body water. BIA estimates body composition based on the principle that an electrical current travels more quickly through hydrated fat-free body mass and fluids than it does through fat and bone due to the higher concentration of electrolytes in fat-free tissues. BIA predicts body density by measuring the rate of a small electrical current passing between two electrodes. Impedance—resistance to the electrical current or speed of the current—is relative to the amount of water and predicts the fat and fat-free mass.36 A variety of BIA methods differ depending on the frequencies used. The most popular is the single-frequency technique, which transmits a current between two surface electrodes placed on either the hand or foot, allowing current measurement from hand-to-hand or foot-to-foot. Newer BIA tools, scales, and estimation equations consider the clients' age, gender, race/ethnicity, and circumference (girth) measurements.
BIA requires standardized measurement conditions to safeguard precision and accuracy. Clients must maintain consistent hydration status, skin temperature, and length of time since exercise. As with the skinfold method, hydration affects the accuracy of the BIA. Impedance is lower in dehydration and higher in the overhydrated. Therefore, dehydrated individuals display a body fat percentage deceivingly higher than the actual percentage. In addition, skin temperature can alter impedance; a warmer skin temperature decreases impedance and results in a lower predicted body fat percentage. Practitioners can promote ambient measurement conditions by maintaining the same room temperature for all measurements. Time since exercise also is an important variable that's best kept consistent. Even moderate exercise before BIA measurements can lead to overestimation of lean body mass and thus underestimation of total body fat percentage.
Even under optimal and standardized conditions, BIA measurements aren't as accurate as other body composition estimation techniques. Conventional BIA is unsuited for predicting body fat because it measures only properties of fat-free mass. The single-frequency BIA is very precise, but only if electrode placement is consistent across measurements.37 BIA tends to overestimate body fatness in lean and athletic clientele and underestimate body fat in obese clients, often negating its utility. If conditions are standardized, it can be a tool better suited for monitoring change over time than for accuracy.
Hydrodensitometry
Densitometry is based on the fact there are specific densities for fat mass and fat-free mass and thus requires measurement of total body density to calculate individual masses. Recall that density is mass divided by volume. The density of fat mass is fairly constant, but the density of fat-free mass depends on its composition (bone vs tissue). Fat-free materials are denser than water, and fat is known to be less dense than water. Therefore, a person with greater fat-free mass likely will have a greater density. The volume of individuals' bodies is calculated based on their density using generalized equations. The body fat percentage then is calculated from the density using either the Brozek or Siri estimation equations,10,37 listed below; population-specific equations have yet to be validated. The Brozek and Siri equations are comparable and differ only by the values into which density is divided and values that are subtracted from the result, illustrated as follows:
• Brozek formula: Body fat (%) = (4.57 / density − 4.142) X 100
• Siri formula: Body fat (%) = (4.95 / density − 4.5) X 100
Body volume originally was measured by hydrodensitometry. This technique is considered a criterion method, or a method providing a standard with which other procedures are compared.38 Underwater weighing requires weighing individuals on dry land, and then immersing them completely in water and weighing them again underwater. The individuals must be weighed underwater three to five times to calculate a reliable average.
Certain factors can affect hydrodensitometry's accuracy. The equipment used varies in sophistication from a stainless steel tub to a cot mounted to an underwater scale. In addition, air remaining in a person's lungs isn't completely expelled; this residual air must be estimated or the resulting densities will be inaccurate. Accuracy also depends on the stillness of the water; there can be no movement. Standardization of the testing environment is critical.
Hydrodensitometry was considered the gold standard for measuring volume for many years and remains a viable method for measuring change over time. Recently, however, it has been viewed as a cumbersome strategy compared with other available methods and as too uncomfortable for most clients. The technique may be inappropriate or uncomfortable for specific patient populations, including children and individuals with anxiety, panic, or posttraumatic stress disorders due to the nature of the measurement method. Moreover, hydrodensitometry may be inappropriate for patients with chronic disease states that result in fluid retention; these effects will modify the composition of lean mass.38
ADP
A newer technique that embraces the principles of densitometry and can be appropriate for a variety of patient populations (eg, children, obese persons, older adults, and disabled persons) is ADP. A more comfortable, noninvasive, and automated process for measuring body composition, ADP is more precise than hydrodensitometry. It measures the volume of air clients displace when placed in an enclosed chamber, often referred to as a "bod pod." The body volume is calculated indirectly by identifying the difference in the volume of air in the chamber when the clients are in the chamber vs when they are not. The calculation also accounts for normal breathing movement with its application of Boyle's law, a governing physical gas principle that states that at a constant temperature, volume and pressure are inversely related. Therefore, standardized temperatures are critical for accurate measurements with ADP. The same limitations described for underwater weighing also apply to ADP, and thus this technique may be inappropriate for children and individuals with pulmonary disease.
DXA
Absorptiometry is the measurement of the amount of radiation absorbed by living tissue to determine the density of the tissue. DXA, previously known as DEXA, calculates mass from the differential absorption of X-rays of two different energies. The strategy uses ionizing radiation, but the effective dose equivalents are below background levels, or those levels that are naturally occurring in the environment.37 The measurements are collected while the clients are in a supine position on the instrument's platform and the arm of the instrument passes over them. The body fat percentage estimation equation—often the Brozek equation—for DXA requires measurement of fat and fat-free masses that are acquired from whole body scans. This method also relies on algorithms that are specific to individual instruments or machines.
DXA is validated for use in children as young as age 4 but also can be used with small infants. It has become the gold standard for measuring not only bone mineral density but also body composition due to its ease, accuracy, and precision. As with other methods, the results are affected by age, race/ethnicity, body figure, and adiposity. Moreover, accuracy varies depending on the region of the body scanned. For example, body fat estimation of the trunk region requires substantial prediction as compared with that of the limbs due to the amount of soft tissue present. Overall, DXA provides the most accurate measures for body composition, with accuracy decreasing with the complexity of the region—from limb (least complex) to trunk (most complex).37
The Nutrition Care Process
It's the role of RDs to understand and use appropriate body composition assessment strategies as part of the nutrition care process (NCP). This standardized, four-step NCP guides RDs' assessment, diagnosis, intervention, and monitoring/evaluation of patients and clientele in a variety of domains. The estimation of an individual's body composition is part of the nutrition assessment, and the results will direct the remainder of the NCP.
Accurate estimates of an individual's body composition provide insight into their overall health, disease risk, and consequences of disease. This insight will help to determine the dietitian's intervention. For example, when dietitians identify that female athletes are maintaining body fat percentages lower than the recommended range, they can provide evidence for the likely health consequences (eg, fracture, amenorrhea, and poor performance) as well as estimate their energy needs for appropriate weight restoration, enhanced athletic ability, and overall health.
Acknowledging the strengths and limitations of the BMI classifications as well as body composition strategies can equip RDs to select the most appropriate strategy. A summary, "Comparison of Common Body Composition Techniques," available at humankinetics.com, presents all of the aforementioned strategies for assessing body composition and compares them by cost of the instrument, time required to appropriately employ the method, the expertise required for a standard and accurate measure, sensitivity of the instrument or precision, and accuracy.38
It's evident that BMI and BIA are quick, inexpensive, and require less expertise. Of the two, BMI is less precise and less accurate at measuring body composition compared with BIA.38 The skinfold method also is fairly quick and inexpensive, but requires greater training and experience to produce an accurate measurement and estimate. When a trained practitioner completes the skinfold assessment, accuracy is comparable to that achieved though BIA. Hydrodensitometry was the gold standard, but is now rarely used due to advances in technology and the cost, time, and expertise required. Today, despite its cost, DXA is the gold standard because it provides accurate estimates that vary little from day-to-day and is capable of monitoring changes in body composition over time.
Knowledge is Impactful
RDs' knowledge of BMI and its indications for use and the variety of strategies for accurately measuring body composition will greatly influence their practices and care for a variety of patient and client populations. Overall, it's vital for dietitians to base their practice on sound evidence and appropriate tools for nutrition assessment and diagnosis because these steps in the NCP will guide their intervention and plan and ultimately dictate the nutrition-related health outcomes for patients and clients.
— Cassie Vanderwall, MS, RD, CD, CDE, CPT, is a Madison, Wisconsin-based freelance food and nutrition writer, manager for the University of Wisconsin (UW) health dietetic internship program, and a clinical nutritionist at UW Health's Pediatric Fitness Clinic.
Learning Objectives
After completing this continuing education course, nutrition professionals should be better able to:
1. Distinguish key methods and strategies used to measure body composition.
2. Assess limitations of key methods and strategies used to measure changes in body composition over time.
3. Compare and contrast the use of BMI with other body composition assessment strategies used in weight management.
4. Demonstrate the role of RDs in using appropriate body composition assessment strategies as part of the nutrition care process.
CPE Monthly Examination
1. Which of the following is an accurate equation for calculating BMI in an adult?
a. BMI = height (m) / weight (kg)2
b. BMI = height (cm) / weight (lbs)2
c. BMI = weight (kg) / height (m)2
d. BMI = weight (lbs) / height (cm)2
2. What is the primary benefit of using BMI as a screening tool?
a. Its ability to determine abdominal adiposity
b. Its simplicity and widespread use
c. Its ability to determine total lean body mass
d. Its direct association with percent body fat
3. Practitioners can be fairly confident when using BMI in athletes, pregnant women, and older adults.
a. True
b. False
4. Which of the following statements accurately describes best the procedures for estimating body composition using the skinfold method?
a. Calipers are used to measure skinfold thickness at four sites on the body to calculate body density.
b. Plastic calipers are used to measure skinfold thickness at two sites on the body to calculate body density.
c. Calipers are used to measure skinfold thickness at three sites on the body to calculate body fatness.
d. Plastic calipers are used to measure skinfold thinness at three sites on the body to calculate body density.
5. Bioelectrical impedance analysis (BIA) estimates body composition based on the principle that an electrical current travels more quickly through hydrated fat-free body mass and fluids than fat and bone mass due to which of the following?
a. The higher concentration of calcium in bone mass
b. The higher concentration of electrolytes in fat mass
c. The higher concentration of electrolytes in lean mass
d. The lower concentration of electrolytes in lean mass
6. Which of the following explains why it's inappropriate to use densitometry in individuals with chronic disease?
a. It may result in overestimation of body fatness due to fluid retention.
b. It may result in overestimation of lean body mass due to fluid retention.
c. It may result in underestimation of body fatness due to increased density of lean mass.
d. It may result in underestimation of lean mass due to excess mineralization.
7. Which of the following strategies more effectively assesses trends over time vs accurate cross-sectional estimates?
a. Skinfold method
b. BIA
c. Hydrodensitometry
d. Dual-energy X-ray absorptiometry (DXA)
8. What is the gold standard method for estimating body composition?
a. Skinfold method
b. BIA
c. Hydrodensitometry
d. DXA
9. Which of the body composition estimation strategies may be most appropriate for RDs in private practice?
a. Skinfold method
b. BIA
c. Hydrodensitometry
d. DXA
10. The estimation of an individual's body composition can be incorporated into all steps of the nutrition care process.
a. True
b. False
References
1. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. J Am Med Assoc. 2014;311(8):806-814.
2. Solving the problem of childhood obesity within a generation. Let's Move website. https://letsmove.obamawhitehouse.archives.gov/sites/letsmove.gov/files/
TaskForce_on_Childhood_Obesity_May2010_FullReport.pdf. Published May 2010. Accessed September 4, 2013.
3. Barlow SE. Expert Committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164-S192.
4. Kuczmarski RJ, Flegal KM. Criteria for definition of overweight in transition: background and recommendations for the United States. Am J Clin Nutr. 2000;72(5):1074-1081.
5. Ogden CL, Li Y, Freedman DS, Borrud LG, Flegal KM. Smoothed percentage body fat percentiles for U.S. children and adolescents, 1999-2004. Natl Health Stat Report. 2011;(43):1-7.
6. Styne DM, Arslanian SA, Connor EL, et al. Pediatric obesity — assessment, treatment, and prevention: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2017;102(3):709-757.
7. Kelly AS, Barlow SE, Rao G, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128(15):1689-1712.
8. Going SB, Lohman TG, Cussler EC, Williams DP, Morrison JA, Horn PS. Percent body fat and chronic disease risk factors in U.S. children and youth. Am J Prev Med. 2011;41(4 Suppl 2):S77-S86.
9. Get the facts on eating disorders. National Eating Disorders Association website. http://www.nationaleatingdisorders.org/get-facts-eating-disorders
10. Brozek J, Grande F, Anderson JT, Keys A. Densitometric analysis of body composition: revision of some quantitative assumptions. Ann N Y Acad Sci. 1963;110:113-140.
11. Siri WE. Body composition from fluid space and density. In: Brozek J, Hanschel A, eds. Techniques for Measuring Body Composition. Washington, DC: National Academy of Sciences; 1961:223-244.
12. Heyward VH, Stolarczyk LM. Applied Body Composition Assessment. Champaign, IL: Human Kinetics; 1996.
13. Muth ND. What are the guidelines for percentage of body fat loss? American Council on Exercise website. https://www.acefitness.org/acefit/healthy-living-article/60/112/what-are-the-guidelines-for-percentage-of-body-fat. Published December 2, 2009.
14. Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101(3 Pt 2):518-525.
15. Eknoyan G. Adolphe Quetelet (1796-1874) — the average man and indices of obesity. Nephrol Dial Transplant. 2008;23(1):47-51.
16. Heymsfield SB, Gallagher D, Mayer L, Beetsch J, Pietrobelli A. Scaling of human body composition to stature: new insights into body mass index. Am J Clin Nutr. 2007;86(1):82-91.
17. Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120(Suppl 4):S193-S228.
18. US Department of Health and Human Services, Centers for Disease Control and Prevention. Body mass index: considerations for practitioners. https://www.cdc.gov/obesity/downloads/BMIforPactitioners.pdf
19. Garrow JS, Webster J. Quetelet's index (W/H2) as a measure of fatness. Int J Obes. 1985;9(2):147-153.
20. Freedman DS, Horlick M, Berenson GS. A comparison of the Slaughter skinfold-thickness equations and BMI in predicting body fatness and cardiovascular disease risk factor levels in children. Am J Clin Nutr. 2013;98(6):1417-1424.
21. Wohlfahrt-Veje C, Tinggaard J, Winther K, et al. Body fat throughout childhood in 2647 healthy Danish children: agreement of BMI, waist circumference, skinfolds with dual X-ray absorptiometry. Eur J Clin Nutr. 2014;68(6):664-670.
22. Flegal KM, Ogden CL, Yanovski JA, et al. High adiposity and high body mass index-for-age in US children and adolescents overall and by race-ethnic group. Am J Clin Nutr. 2010;91(4):1020-1026.
23. Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002;3(3):141-146.
24. Adult obesity facts. Centers for Disease Control and Prevention website. http://www.cdc.gov/obesity/data/adult.html. Updated September 1, 2016.
25. Kitahara CM, Flint AJ, Berrington de Gonzalez A, et al. Association between class III obesity (BMI of 40-59 kg/m2) and mortality: a pooled analysis of 20 prospective studies. PLoS Med. 2014;11(7):e1001673.
26. Himes JH. Anthropometric Assessment of Nutritional Status. New York, NY: Wiley-Liss, Inc; 1991.
27. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1-452.
28. De Lorenzo A, Bianchi A, Maroni P, et al. Adiposity rather than BMI determines metabolic risk. Int J Cardiol. 2013;166(1):111-117.
29. Katzmarzyk PT, Barreira TV, Broyles ST, et al. Association between body mass index and body fat in 9-11-year-old children from countries spanning a range of human development. Int J Obes Suppl. 2015;5(Suppl 2):S43-S46.
30. Pietrobelli A, Faith MS, Allison DB, Gallagher D, Chiumello G, Heymsfield SB. Body mass index as a measure of adiposity among children and adolescents: a validation study. J Pediatr. 1998;132(2):204-210.
31. Chin J, Wang H, Jia-Shuai M. The association between body mass index, waist circumference with body fat percent, and abdominal fat rate in overweight and obese pupils. Prev Med. 2013;47(7):603-607.
32. Burkhauser RV, Cawley J. Beyond BMI: the value of more accurate measures of fatness and obesity in social science research. J Health Econ. 2008;27(2):519-529.
33. Widhalm K, Schönegger K. BMI: Does it really reflect body fat mass? J Pediatr. 1999;134(4):522-523.
34. Jackson AS, Pollock ML. Practical assessment of body composition. Phys Sportsmed. 1985;13(5):76-90.
35. Lohman TG, Pollock ML, Slaughter MH, Brandon LJ, Boileau RA. Methodological factors and the prediction of body fat in female athletes. Med Sci Sports Exerc. 1984;16(1):92-96.
36. Kyle UG, Bosaeus I, De Lorenzo AD, et al. Bioelectrical impedance analysis — part I: review of principles and methods. Clin Nutr. 2004;23(5):1226-1243.
37. Wells JC, Fewtrell MS. Measuring body composition. Arch Dis Child. 2006;91(7):612-617.
38. Howley E, Thompson D. Choose the correct method for body composition assessment. Human Kinetics website. http://www.humankinetics.com/excerpts/excerpts/choose-the-correct-method-for-body-composition-assessment
