Today’s Dietitian
Vol. 19, No. 6, P. 42
Learn About the SCD to Support Clients With IBD and How It Compares With Other Evidence-Based Nutritional Therapies
Suggested CDR Learning Codes: 5000, 5220, 5420
Suggested CDR Performance Indicators: 8.1.5, 8.3.1, 8.3.6
CPE Level 2
Take this course and earn 2 CEUs on our Continuing Education Learning Library
Inflammatory bowel disease (IBD) is an often-debilitating inflammatory condition of the gastrointestinal (GI) tract that’s becoming more common both in the United States and abroad. While medications are available, they’re expensive, may cause significant side effects, and often are ineffective at controlling the disease process. Consequently, there’s a push from both a health and economic standpoint for nonpharmacologic treatments. The Specific Carbohydrate Diet (SCD) has been touted for decades as a means of establishing or maintaining remission, and, after nearly a century, research is finally available to assess the potential utility of this strategy.
This continuing education course examines the evidence that the SCD may be used to support clients with IBD and explores how the SCD compares with other evidence-based nutritional therapies for IBD.
The two primary types of IBD are Crohn’s disease (CD) and ulcerative colitis (UC).
IBD most commonly occurs in developed countries and urban areas.1 There are many theories about the etiology of IBD, and current research suggests that genetics, environmental factors, hygiene, the microbiome, and lifestyle factors—including smoking, diet, stress, and even medications—may play a role.1,2 Studies indicate that IBD is becoming more common both in the United States and worldwide and that it affects people at a younger age.1 This is concerning, since an earlier age at diagnosis has been associated with increased risk of colorectal cancers and a worse prognosis.3
While UC and CD often present with similar and often overlapping symptoms such as abdominal pain and diarrhea, the pathophysiology often is distinct. UC typically affects the rectum and all or parts of the colon.2 It usually involves only the mucosal and/or the submucosal layers of tissue, and the damage seen in UC usually is continuous.
CD often affects the ileum, or the terminal section of the small intestine, and the colon, and it may affect any part of the GI tract from the mouth to the anus and any or all layers of the mucosa.2,3 The presentation of CD may be patchy, with both areas of affected and unaffected tissue.2
Collectively, IBD affects approximately 1.4 million Americans.2 It’s a costly condition. The Centers for Disease Control and Prevention estimates that as of 2008 direct treatment costs are $6.3 billion yearly, with an additional $5.5 billion annually in indirect costs due to lost productivity,4 and the cost likely has increased since then. Approximately 1.3 million physician visits per year and 92,000 hospitalizations are due to IBD.4
People with IBD often also incur significant indirect costs, including decreased quality of life, lower productivity at work, and decreased leisure time.5 In addition, IBD has a profound effect on nutritional status and often is associated with malnutrition.
Nutrient Deficiencies
Severe and active disease often is associated with protein and energy malnutrition; however, micronutrient deficiencies are common across a range of patients with IBD.6 Nutritional deficiencies may be due to decreased food intake, increased nutrient losses and malabsorption, increased nutrient needs due to the disease state, nutrient depletions due to medications, decreased absorptive capacity following a surgical resection, and even dietary restrictions intended to control symptoms.6 Typically, micronutrient deficiencies are more common in people with CD, since it may affect a larger proportion of the GI tract, including the small intestine, where the majority of nutrient absorption and assimilation occurs.6
The most frequent nutritional deficiencies in patients with IBD include folate, vitamin A, vitamin D, calcium, and iron. Magnesium and zinc deficiencies also are believed to be common, and lower levels of B1, B12, vitamin E, vitamin K, and selenium also are documented.6 Appropriate testing and supplementation as needed will support the nutritional care of patients with IBD.
Treatment Options
One of the mainstays of treatment for IBD is pharmacotherapy aimed at inducing and maintaining remission. In adults, this typically involves the long-term use of various medications, from the milder aminosalicylates to corticosteroids, thiopurines, immunomodulatory medications, and biologics.7 These medications can have significant consequences for weight, blood sugar, and bone health in adults, and may have a profoundly negative impact on the growth potential of children with IBD.
More important, patients have a variable response to the medications and often a diminished response over time. While every person has a different response, the reality is that most of the commonly used medications, including oral 5-aminosalicylates (5-ASA) treatments, steroids, thiopurines, and antitumor necrosis factor medications, are effective at inducing or maintaining remission in fewer than one-half of patients with IBD.7 Although many new medications and treatments are underway, a large percentage of people with IBD experience inadequate relief from medications.
If patients don’t remain in remission and the disease process continues, surgical removal of diseased areas of the GI tract often are necessary, with significant physiologic consequences. Because of the difficulty in establishing and maintaining remission and the physical damage due to IBD, there’s been great interest in finding alternative approaches both for inducing and maintaining remission.
The Specific Carbohydrate Diet
There’s an increasing body of evidence that the SCD is a viable option for both improving symptom management and inducing or maintaining remission among people with IBD. The SCD was first proposed by Sidney V. Haas, MD, in the 1920s as a way to manage celiac disease, and it was described in a textbook by Haas and his son, which was published in 1951.8 The diet was popularized by Elaine Gottschall, BA, MSc, based on her experiences with her daughter’s healing from UC under Haas’ care and subsequent decades of advocacy with patients. She published the definitive SCD guide, Breaking the Vicious Cycle: Intestinal Health Through Diet in 1994.8 For many decades, clients have experimented with the SCD to reduce or resolve IBD symptoms, largely relying on anecdotal reports.
The premise of the SCD as described by Gottschall is that humans evolved to digest simple, single molecules of carbohydrates, or monosaccharides, efficiently, because they’re easily absorbed and assimilated by the body. Fruits, many vegetables, and honey are comprised of carbohydrates with simple sugars. According to this theory, complex carbohydrates, such as disaccharides or polysaccharides, aren’t immediately absorbed; this can lead to an overgrowth of bacterial flora and inappropriate bacterial fermentation. Acidic and inflammatory byproducts of this process can cause damage to the intestines and interrupt normal enzyme function, a situation that can lead to malnutrition and diarrhea.8 To date, the hypothesis concerning the underlying physiological mechanism hasn’t been adequately elucidated.
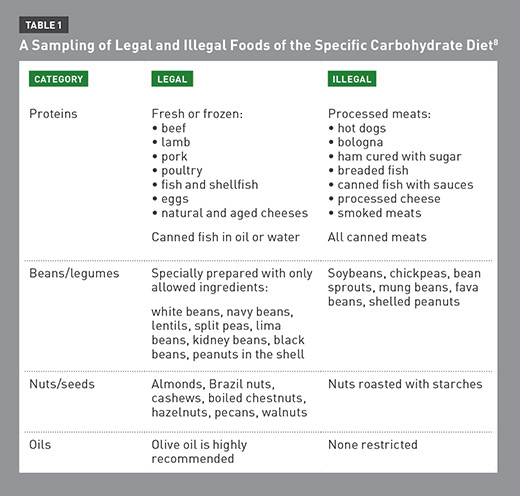
The SCD permits the consumption of almost all fruits, most vegetables, nuts, eggs, fish, poultry, meat, fats, specially fermented yogurt, and dry curd cottage cheese. Added sugar is limited to honey. On the SCD, clients must strictly avoid complex carbohydrates, including grains such as corn, pseudograins, potatoes, most dairy products aside from specially prepared yogurt, soy, canned beans, seaweeds and derivatives, most sweets including chocolate, many preservatives and additives, and processed foods.8 The SCD isn’t necessarily a low-carbohydrate diet, but it’s extremely specific about the types of carbohydrates that are permitted.
Detailed lists of the foods permitted, known as “legal,” and the foods that must be avoided, known as “illegal,” are summarized in Table 1 on page 45.8
According to Gottschall, the SCD is extremely strict, and the author’s recommendation is to follow the diet with “fanatical adherence.”8 Per Gottschall, patients often experience improvements by one month on the diet, although the author specifically recommends that people with IBD remain on a strict SCD diet for a minimum of two years.8 Although Breaking the Vicious Cycle is very clear on the strictness and length of time necessary for remission, the ideal length of time for the diet and degree of adherence are topics of considerable debate and active research.
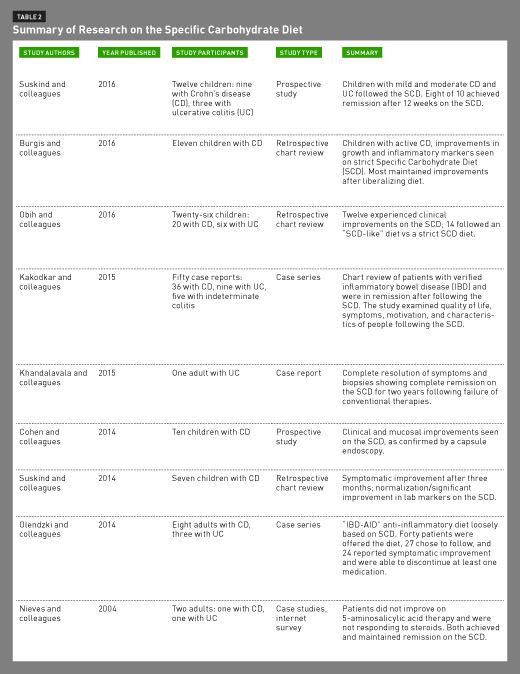
A range of studies on the SCD are now available, from case studies and reports to prospective studies, many of which are summarized in Table 2. The primary goal of the research is to determine whether the SCD is a safe and effective option for establishing and maintaining remission of IBD in children and adults.
Research on the SCD
Suskind and colleagues at Seattle Children’s Hospital did a 12-week prospective study on the effectiveness of the SCD with 12 children who had UC or CD and were experiencing mild to moderate disease activity. According to the results, published online in December 2016 in the Journal of Clinical Gastroenterology, RDs provided individual counseling and support throughout the study. The diet was ineffective for two children, and two children were unable to maintain the diet. The remaining eight children experienced disease remission within the 12 weeks, with statistically and therapeutically significant decreases in disease activity scores and inflammatory markers. Moreover, researchers performed fecal studies before and after the dietary change showing significant changes in microbial composition, and further study is needed to understand potential relevance of microbial changes.
A 2016 retrospective chart review by Burgis and colleagues examined 11 pediatric patients with CD following the SCD. The patients either had experienced a flare or were newly diagnosed at the time of SCD introduction. Some were only following the SCD, while others also were taking antibiotics or other medications. After participants began a strict SCD, hematocrit and albumin values significantly improved, sedimentation rate improved for all patients, and 90% of children gained weight. Most children also grew taller. The second phase of the study involved mild liberalization of the SCD after approximately 7.5 months on the diet. The degree of liberalization was individualized, ranging from an illegal ingredient or meal daily to an illegal meal every two weeks. Most improvements seen with the strict SCD were maintained on the liberalized diet, however, researchers observed a small decrease in weight percentile. The authors conclude, “A strict SCD was effective to improve laboratory values and maintain growth parameters in pediatric patients with CD.”9
A 2016 retrospective study at Seattle Children’s Hospital involved 26 patients with UC with active IBD who adhered to the SCD. The primary reason the majority of participants followed the SCD was to avoid medication (17 of 26 patients, or 65%); nine of the 26 (34%) patients followed the diet due to inadequate improvement or side effects of the medications. Some used the SCD as the primary treatment modality, while others used medications concurrently. Of the 26 who followed the SCD, 12 experienced improvements in clinical and inflammatory markers. Of the 15 who were on medication, two were able to discontinue medications and maintain remission solely on the SCD. In this study, the children took part in the decision process regarding their diets; about one-half opted to follow an “SCD-like” diet with liberalization. The authors also note that many had difficulty with compliance because of the strict nature of the diet, and there were some concerns with weight loss for nine patients, even though a nutritionist on staff provided support.10
The Journal of the Academy of Nutrition and Dietetics published a 2015 case series review on adult patients with IBD who reported achieving and maintaining remission on the SCD. Both the diagnosis of IBD and remission were independently corroborated with medical records. Twenty-two of the 50 were off all medications, and 16 discontinued their medications while on the SCD and maintained remission. The self-report of dietary compliance ranged from 71% to 100%, with an average of 95% compliance. The main motivators for following the SCD were fear of long-term consequences of medication (82%), medications weren’t effective (64%), belief that the SCD is more effective than medications (64%), and adverse reactions to medications (56%). Overall, the group was highly educated and most had college or graduate degrees. Subjects estimated that food preparation time was 10.8 hours weekly and most noticed symptomatic improvement approximately one month after starting the SCD.11
A case report by Khandalavala and Nirmalraj describes a 73-year-old Asian physician with UC who didn’t respond to conventional pharmacologic therapies. She noticed symptomatic improvements after three months on the SCD, and a colonoscopy at two years indicated a complete remission of her UC. Accidental consumption of foods that were disallowed on the SCD caused acute flares in symptoms.12
Cohen and colleagues performed a prospective study using the SCD with children with active CD, and nine of the 10 children completed the study. Researchers saw clinical improvement in disease status of 80%, and 60% achieved remission by 12 weeks. Six of the seven patients who remained on the diet for a full year achieved clinical remission. Data weren’t collected on “cheating” on the diet and whether it might have affected clinical response to the SCD.13
Suskind and colleagues at Seattle Children’s Hospital examined charts of seven children with mild, moderate, or severe CD who followed the SCD. All experienced a resolution of symptoms after three months on the diet and increased their height and weight while following the SCD. Researchers observed normalization in hematocrit, sedimentation rate, and stool calprotectin values.14
In 2014, Olendzki and colleagues at the University of Massachusetts studied the IBD anti-inflammatory diet (IBD-AID), a modified version of the SCD. IBD-AID incorporates many principles of the SCD, including consumption of lean proteins, fruits, vegetables, and legumes, but it also encouraged the inclusion of products not allowed on the SCD, such as prebiotic fibers, chia and flax seeds, kefir, yogurt, and other probiotic foods. The researchers offered the diet to patients who were refractory to pharmaceutical therapies or hadn’t experienced the degree of symptomatic improvement desired. Of the 40 people offered the diet, 13 declined, 24 had a positive response, and three had a mixed response. Complete data were available only for 11 clients following the diet, and 100% experienced symptomatic improvements and were able to decrease the amount of medication used.15
A 2004 study examined two case studies. One patient with UC experienced flares despite 5-ASA therapy and flared while tapering off steroids. She reported symptomatic improvement within two weeks on the SCD, and a follow-up colonoscopy at one year indicated disease remission. The second was a 24-year-old with CD who didn’t respond to 5-ASA therapy and experienced a flare on prednisone. She experienced symptomatic improvement within one week on the SCD, tapered off steroids after one month on the diet, and remained in remission without medications for the next three years. This paper also included a survey of patients using the SCD. Eighty-four percent of patients reported they were in remission following the SCD; however, patient reports weren’t confirmed through medical record review, so this can’t be corroborated.16
One area of great interest is why the SCD works. While there likely are many factors, one answer is that the diet modifies the microbiome. A small pilot study examined stool samples of patients with CD and healthy controls, comparing microbial changes on the SCD with those in individuals following a low-residue diet. The patients with IBD had lower microbial diversity and different bacteria than did healthy controls before the dietary modifications.2,17 While following the SCD, patients had a significantly wider range of microbial diversity, which generally is associated with better health. Conversely, researchers saw a decrease in microbial expression on a low-residue diet.17 Forthcoming research from Seattle Children’s Hospital will examine similar themes of microbiome changes on the SCD.
Other Nutritional Strategies
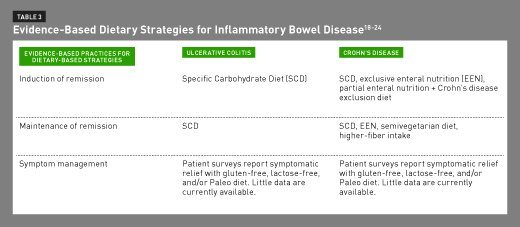
For adults in the United States, medications usually are the first line of therapy for IBD. However, in children with CD, the primary nutritional strategy to induce remission is exclusive enteral nutrition (EEN), or sole consumption of a nutritionally complete formula for six to eight weeks with no additional food and only water. EEN is primarily used for children, and studies show that EEN can bring more than 80% of children with CD into remission. Beyond simple taste fatigue, EEN can be socially, emotionally, and logistically challenging.18 EEN also may be effective in adults with CD, but it’s rarely routinely used outside of Japan.19 Moreover, current guidelines recommend EEN only for CD because EEN doesn’t induce remission in UC.20
Unfortunately, to date, no direct studies are published that directly compare the effectiveness of EEN with the SCD, and only one 2017 case study examines both strategies. A 15-year-old with CD who had persistently elevated inflammatory markers was given EEN for eight weeks, which decreased his inflammatory markers, such as fecal calprotectin and sedimentation rate. However, the levels were still elevated. He then began the SCD, and his levels of inflammation decreased. After two months on the SCD he was able to stop his medication; after six months on the SCD he was able to liberalize his diet while inflammatory markers remained stable.21
While partial enteral nutrition (PEN) hasn’t been effective, a combination of PEN and a restricted diet known as the Crohn’s disease exclusion diet may be effective. A 2014 pilot study examined the use of a partial enteral diet with 47 children and adults with mild to moderate CD. In addition to enteral feeds, the patients followed a strict gluten-free, dairy-free diet without animal fat. The diet also removed all processed and canned goods and called for avoidance of all thickeners and emulsifiers. Seventy percent of children and 69% of adults went into remission while following the diet.22 A larger trial is underway.
A 2010 prospective study in Japan examined the use of a semivegetarian diet to support remission among adults with CD. The semivegetarian diet involves a lacto-ovo vegetarian diet with fish once per week and a small portion of meat every two weeks. Researchers encouraged intake of vegetables, fruits, legumes, rice, and an abundance of fermented foods, and they provided menu plans and nutritional support. Twenty-two people in remission with CD were instructed about the diet, and 16 followed it for two years. Ninety-four percent of those adhering to the diet maintained remission.23 It’s uncertain which components of the diet were most supportive of maintaining remission. This study is encouraging and hopefully larger investigations will follow; however, it was aimed at maintaining remission, not inducing remission. It also wasn’t investigated in patients with UC.
Other dietary strategies proposed for managing symptoms of IBD include low-FODMAP (fermentable oligo-, di-, and monosaccharides and polyols), gluten-free, lactose-free, or Paleo diets.20 A small body of research supports a low-FODMAP diet for symptomatic relief.24 In addition, IBD patient surveys report a reduction in symptoms on a gluten-free, lactose-free, and/or Paleo diet. However, there’s no evidence to suggest that these diets have the potential to induce or maintain remission.20 The primary role of these diets is likely symptom management.20
A low-fat, low-fiber diet for IBD has long been standard nutritional practice, especially right after a disease flare. The theory was that there might be scarring or stricturing in CD, and fiber could potentially worsen symptoms or cause a blockage. However, newer research challenges this idea. A meta-analysis on IBD and fiber indicates that fiber may have a slightly beneficial impact on UC, and that there’s no evidence that fiber should be limited, except in cases of a bowel obstruction.25 In addition, a 2016 study of patients in remission with CD showed that the people with the highest quartile of fiber had a 40% lower risk of a CD flare compared with the people in the lowest quartile of fiber intake.26
There’s a growing body of research investigating the use of probiotic supplements for IBD. According to the 2015 Consensus Opinion from the Yale/Harvard Triennial Workshop on Probiotic Recommendations, there’s significant evidence of benefit from a multistrain probiotic brand such as VSL#3 and E coli Nissle 1917 for UC. Evidence is weaker for the use of probiotics in CD, and some studies support the use of E coli Nissle 1917, Saccharomyces boulardii, and Lactobacillus rhamnosus GG.27 For more detail, see “Probiotics & IBD” in the April 2013 edition of Today’s Dietitian.
Practical Applications
Both CD and UC can be challenging conditions associated with physical and emotional costs. As IBD becomes more common globally, the economic burden of disease symptoms, surgeries, and medications will only grow, and this makes dietary strategies even more valuable. For a segment of people with IBD who don’t see adequate improvement on the medications, experience intolerable side effects, can’t afford the medications, or simply want an alternative option with a lower side effect profile, the SCD may be an effective therapeutic option. However, as mentioned throughout this course, implementation of the diet requires significant time and commitment.
While some patients were successful using only the SCD, in many cases, the SCD was used in conjunction with medications and other treatments. All patients will have different nutritional, social, cultural, and logistical needs and preferences, and dietary changes should be tailored to the individual with active collaboration between the RD and the rest of the patient’s health care team. While patients may be eager to stop treatments when they notice symptomatic improvements, they should be actively discouraged from changing or discontinuing medications without oversight and the consent of the team.
As seen in Table 3, there are several nutritional options for patients with CD, including the SCD, EEN, and PEN in conjunction with the Crohn’s disease exclusion diet. Research isn’t yet available to directly compare the efficacy of each treatment; it’s unknown whether there are specific patient characteristics (eg, type of IBD, location of damage, and degree of damage) that affect the relative efficacy of each diet. Additional research will begin to fill in these gaps so health care professionals can guide patients toward the most efficacious dietary strategies. The semivegetarian diet also may be an option for maintaining (not inducing) remission among people with CD. Thus far, none of the alternative dietary options besides the SCD have been researched for patients with UC.
The current research suggests the SCD belongs on the table as a viable option for inducing or maintaining remission and health care professionals can present it as an evidence-based option. According to David Suskind, MD, of Seattle Children’s Hospital, “Eating healthful foods and removing processed foods reduces disease activity for IBD. But if you’re using nutrition and diet as a therapy and want to limit intestinal inflammation, we lean towards the SCD. A low-FODMAP diet works well to decrease symptoms, but not necessarily the inflammation.”
While there’s evidence that the SCD is helpful, it requires commitment. It’s important that nutrition professionals develop more comprehensive strategies to aid in the implementation of the SCD. In most studies, some participants declined to undertake the diet or dropped out due to the intensity of requirements. There’s ample indication that degree of compliance also may affect physiologic improvement. It’s necessary that dietitians assess what supports are needed to raise the likelihood of success on the diet and develop appropriate strategies to fill in those needs. This may include SCD recipe books and websites, personal chefs that can make SCD-compliant meals, stores that carry SCD-legal products, cooking classes, and support groups, especially for children.
Given the high rate of nutritional deficiencies in people with IBD and at least some indications for particular concerns with weight loss in children on the SCD, particular attention should be paid to nutritionally balanced, accessible meals and appropriate supplementation to complement the diet.
Conclusion
Based on studies done thus far, the SCD appears to be an effective way to both establish and maintain remission for people with UC or CD. Both prospective and retrospective studies at different institutions with slightly different protocols have demonstrated benefits, and improvements have been observed in people of different ages and genders and with different locations and disease severity. Variants on the SCD, such as IBD-AID or “SCD-like” diets also may prove to be viable strategies—in fact, Seattle Children’s Hospital is investigating the effectiveness of the SCD compared with a modified SCD with added foods, such as rice and oats, vs a more whole-foods based diet to see which strategy yields the best clinical results. Several additional clinical trials are underway or in review for publication, with research projects underway at Stanford and University of Massachusetts. Forthcoming research is aimed at determining the degree of adherence necessary to achieve clinical remission and a better understanding of the physiological underpinnings of the diet that lead to positive results, especially as it relates to the gut microbiome.
In addition, larger and more robust prospective studies will give a better idea of the percentage of people with IBD who will benefit from the SCD, and the physical characteristics and lifestyle factors that help contribute to the patient’s success on the SCD.
— Cheryl Harris, MPH, RD, specializes in gastrointestinal disorders and autoimmune disease in private practice in Northern Virginia.
Learning Objectives
After completing this continuing education course, nutrition professionals should be better able to:
1. Describe the challenges people with inflammatory bowel disease (IBD) face and the necessity for improved treatment options, including dietary strategies.
2. Interpret the fundamentals of the Specific Carbohydrate Diet (SCD), from the origins to the implementation of the diet.
3. Assess the strengths and weaknesses of current research on the SCD.
4. Contrast the potential utility and research on the SCD with other diets used for IBD.
[Sidebar]
RESOURCES FOR FURTHER STUDY
• Official website on implementing the Specific Carbohydrate Diet: www.breakingtheviciouscycle.info
• Original guidebook on the Specific Carbohydrate Diet: Breaking the Vicious Cycle: Intestinal Health Through Diet by Elaine Gottschall, BA, MSc
• Guide for Specific Carbohydrate Diet implementation for children with inflammatory bowel disease: NIMBAL Therapy by David L. Suskind, MD, available at www.nimbal.org.
CPE Monthly Examination
1. Which of the following correctly describes Crohn’s disease (CD) and ulcerative colitis (UC)?
a. They are two forms of irritable bowel syndrome.
b. UC affects the small intestine; CD affects the large intestine.
c. CD can affect anywhere in the gastrointestinal tract, from mouth to anus.
d. UC affects all layers of tissue in the intestine.
2. What are factors that promote the development of inflammatory bowel disease (IBD)?
a. Genes, hygiene, infections, medications, and smoking.
b. Eating more fruits and vegetables.
c. Not getting enough sleep.
d. An excess of supplemental beta-carotene.
3. The premise of the Specific Carbohydrate Diet states which of the following?
a. Complex carbohydrates have a lower glycemic load and are therefore beneficial and supportive.
b. Animal protein raises cholesterol and causes intestinal harm.
c. Humans are not designed to digest complex carbohydrates, and they cause intestinal damage.
d. An excess of fats and oils leads to intestinal inflammation.
4. Foods permitted on the Specific Carbohydrate Diet include which of the following?
a. All fruits, vegetables, beans, nuts, and seeds
b. Any kind of dairy
c. Gluten-free whole grains in moderation
d. Any kind of plain beef, poultry, fish, and eggs
5. Studies show that the Specific Carbohydrate Diet may best benefit which of the following?
a. Only children
b. Only people with CD
c. Only people with mild disease
d. People with any form of IBD at a range of ages
6. Which of the following has evidence-based research to demonstrate that it may help people with CD induce remission?
a. Paleo diet
b. Low-FODMAP diet
c. Food allergy or food intolerance testing
d. Enteral feedings
7. Which of the following has evidence-based research to demonstrate that it may help people with UC induce remission?
a. Semivegetarian diet
b. Specific Carbohydrate Diet
c. Grain-free or Paleo diet
d. Gluten-free diet
8. For people with CD, which of the following dietary strategies is supported by research to maintain remission?
a. A low-fat, low-fiber diet to manage strictures
b. High omega-3 foods daily
c. A higher-fiber diet, as tolerated
d. A sugar-free diet
9. The current recommendations on probiotics for IBD include which of the following?
a. Strict avoidance of all probiotic supplements and probiotic foods
b. Twice daily consumption of unsweetened yogurt
c. Use of VSL#3 or E coli Nissle 1917 for UC
d. Consumption of Lactobacillus acidophilus and L reuteri for CD
10. Which of the following is among the main challenges in implementing the Specific Carbohydrate Diet?
a. Because it’s so new, there isn’t yet consensus on what foods are permitted.
b. Significant time requirements for food preparation are involved.
c. It hasn’t yet been utilized in hospitals or medical settings.
d. It tends to cause significant and inappropriate weight gain.
References
1. Ye Y, Pang Z, Chen W, Ju S, Zhou C. The epidemiology and risk factors of inflammatory bowel disease. Int J Clin Exp Med. 2015;8(12):22529-22542.
2. Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361(21):2066-2078.
3. M’Koma AE. Inflammatory bowel disease: an expanding global health problem. Clin Med Insights Gastroenterol. 2013;6:33-47.
4. An expensive disease without a cure. Centers for Disease Control and Prevention website. http://www.cdc.gov/ibd/pdf/inflammatory-bowel-disease-an-expensive-disease.pdf. Accessed August 1, 2016.
5. Kawalec P. Indirect costs of inflammatory bowel diseases: Crohn’s disease and ulcerative colitis. A systematic review. Arch Med Sci. 2016;12(2):295-302.
6. Hwang C, Ross V, Mahadevan U. Micronutrient deficiencies in inflammatory bowel disease: from A to zinc. Inflamm Bowel Dis. 2012;18(10):1961-1981.
7. Peyrin-Biroulet L, Lémann M. Review article: remission rates achievable by current therapies for inflammatory bowel disease. Aliment Pharmacol Ther. 2011;33(8):870-879.
8. Gottschall E. Breaking the Vicious Cycle: Intestinal Health Through Diet. 12th printing. Baltimore, Ontario, Canada: Kirkton Press Ltd; 2007.
9. Burgis JC, Nguyen K, Park KT, Cox K. Response to strict and liberalized specific carbohydrate diet in pediatric Crohn’s disease. World J Gastroenterol. 2016;22(6):2111-2117.
10. Obih C, Wahbeh G, Lee D, et al. Specific carbohydrate diet for pediatric inflammatory bowel disease in clinical practice within an academic IBD center. Nutrition. 2016;32(4):418-425.
11. Kakodkar S, Farooqui AJ, Mikolaitis SL, Mutlu EA. The Specific Carbohydrate Diet for inflammatory bowel disease: a case series. J Acad Nutr Diet. 2015;115(8)1226-1232.
12. Khandalavala BN, Nirmalraj MC. Resolution of severe ulcerative colitis with the Specific Carbohydrate Diet. Case Rep Gastroenterol. 2015;9(2):291-295.
13. Cohen SA, Gold BD, Oliva S, et al. Clinical and mucosal improvement with specific carbohydrate diet in pediatric Crohn disease. J Pediatr Gastroenterol Nutr. 2014;59(4):516-521.
14. Suskind DL, Wahbeh G, Gregory N, Vendettuoli H, Christie D. Nutritional therapy in pediatric Crohn disease: the specific carbohydrate diet. J Pediatr Gastroenterol Nutr. 2014;58(1):87-91.
15. Olendzki BC, Silverstein TD, Persuitte GM, Ma Y, Baldwin KR, Cave D. An anti-inflammatory diet as treatment for inflammatory bowel disease: a case series report. Nutr J. 2014;13:5.
16. Nieves R, Jackson RT. Specific carbohydrate diet in treatment of inflammatory bowel disease. Tenn Med. 2004;97(9):407.
17. Walters SS, Quiros A, Rolston M, et al. Analysis of gut microbiome and diet modification in patients with Crohn’s disease. SOJ Microbiol Infect Dis. 2014;2(3):1-13.
18. Ruemmele FM, Veres G, Kolho KL, et al. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J Crohns Colitis. 2014;8(10):1179-1207.
19. Wall CL, Day AS, Gearry RB. Use of exclusive enteral nutrition in adults with Crohn’s disease: a review. World J Gastroenterol. 2013;19(43):7652-7660.
20. Shah ND, Parian AM, Mullin GE, Limketkai BN. Oral diets and nutrition support for inflammatory bowel disease: what is the evidence? Nutr Clin Pract. 2015;30(4):462-473.
21. Nakayuenyongsuk W, Christofferson M, Nguyen K, Burgis J, Park KT. Diet to the rescue: cessation of pharmacotherapy after initiation of exclusive enteral nutrition (EEN) followed by strict and liberalized specific carbohydrate diet (SCD) in Crohn’s disease [published online January 13, 2017]. Dig Dis Sci. doi: 10.1007/s10620-016-4446-1.
22. Sigall-Boneh R, Pfeffer-Gik T, Segal I, Zangen T, Boaz M, Levine A. Partial enteral nutrition with a Crohn’s disease exclusion diet is effective for induction of remission in children and young adults with Crohn’s disease. Inflamm Bowel Dis. 2014;20(8):1353-1360.
23. Chiba M, Abe T, Tsuda H, et al. Lifestyle-related disease in Crohn’s disease: relapse prevention by a semi-vegetarian diet. World J Gastroenterol. 2010;16(20):2484-2495.
24. Gearry RB, Irving PM, Barrett JS, Nathan DM, Shepherd SJ, Gibson PR. Reduction of dietary poorly absorbed short-chain carbohydrates (FODMAPs) improves abdominal symptoms in patients with inflammatory bowel disease — a pilot study. J Crohns Colitis. 2009;3(1):8-14.
25. Wedlake L, Slack N, Andreyev HJ, Whelan K. Fiber in the treatment and maintenance of inflammatory bowel disease: a systematic review of randomized controlled trials. Inflamm Bowel Dis. 2014;20(3):576-586.
26. Brotherton CS, Martin CA, Long MD, Kappelman MD, Sandler RS. Avoidance of fiber is associated with greater risk of Crohn’s disease flare in a 6-month period. Clin Gastroenterol Hepatol. 2016;14(8):1130-1136.
27. Floch MH, Walker WA, Sanders ME, et al. Recommendations for probiotic use — 2015 update: proceedings and consensus opinion. J Clin Gastroenterol. 2015;49(Suppl 1):S69-S73.


