Today’s Dietitian
Vol. 18 No. 2 P. 24
Research shows that consuming plenty of plant-based foods containing highly absorbable calcium and vitamin D is the key to optimal bone health.
Research indicates that well-planned vegan diets, which are devoid of any animal products, including meat, fish, poultry, dairy, and eggs, may be linked with health benefits, including a lower risk of heart disease, type 2 diabetes, obesity, and certain types of cancer. However, a shadow has been cast over one potential concern: bone health. Some studies suggest that vegans may be at higher risk of bone fracture, but the evidence isn’t so clear cut. Factor in that confusion abounds over bone nutrition in the vegan community, which may lead to poorly planned diets. In the end, it may be the type of diet a vegan follows that matters more than being vegan itself.
Raising Bone Health Concerns
Osteoporosis is a serious health concern. This common chronic condition, marked by progressive loss of bone mineral density (BMD) and compromised bone strength, is associated with increasing risk of fracture over time. More than 200 million people worldwide suffer from this disease,1 and 30% of all postmenopausal women in the United States and Europe have osteoporosis.2
The process of bone mineralization (the laying down of minerals on the bone matrix) and resorption (when osteoclasts break down bone and release calcium into the blood) is complex and is affected by many factors, including nutrients, such as calcium, vitamins D and B12, zinc, protein, and omega-3 fatty acids, according to Katherine L. Tucker, PhD, a professor of nutritional epidemiology at the University of Massachusetts Lowell. Tucker, a leading researcher on bone nutrition, says that unless one is very careful to ensure that all needed nutrients are obtained, it’s easy for vegans to become deficient in these important nutrients.
“An animal-free diet can be so healthful and offer incredible benefits, but it’s hard to deny that certain vitamins and minerals may need to be supplemented in the majority of vegans,” says Ginger Hultin, MS, RDN, CSO, LDN, plant-based nutrition expert and owner of Champagne Nutrition in Seattle. “Any type of diet needs to be planned to avoid deficiencies in vitamins or minerals. Huge studies and meta-analyses have shown that vegans may be at a slightly higher risk for reduced bone density.”
In a 2009 meta-analysis of studies looking at the effects of vegetarian diets on BMD, vegans had lower lumbar spine BMD compared with omnivores.3 And in the EPIC-Oxford study, fracture rates in the United Kingdom (UK) were compared among the following four diet groups: meat eaters, fish eaters, vegetarians, and vegans. While the fish eaters and vegetarians had rates of fractures similar to those of the meat eaters, the vegans had a higher incidence rate ratio of 1.15.4
However, one intriguing study compared 105 Buddhist nuns, who were lifelong vegans due to religious rule, with 105 omnivorous women from monasteries in Ho Chi Minh City, Vietnam. Researchers found that the median intake of calcium among vegans was lower, yet it wasn’t correlated with lower BMD.5
Another concern is the impact of veganism on bone health among children and adolescents. “These are formative years for bone development, and a poorly designed vegan diet during that time may be a risk factor for bone health, among many, many other risk factors,” Hultin says.
“Up to 90% of peak bone mass is acquired by age 18 in girls. Women who have a higher bone mass are at lower risk of osteoporosis later in life,” says Reed Mangels, PhD, RD, LDN, nutrition adviser for The Vegetarian Resource Group.
In a study of one vegan family, scientists found that low dietary intake of calcium and vitamin D was linked to lower BMD, which was even more pronounced in the children, though it’s important to note the small size of this study.6 In a study of 50 vegetarian and 50 omnivorous children, markers of bone turnover were lower in vegetarian children compared with omnivorous children. In addition, calcium and vitamin D intake was two times lower in the vegetarian children.7
Linked to Intake, Not Veganism
When taking a closer look at the research, lower BMD may be related to poor nutrient intake within a vegan diet. The EPIC-Oxford study found that among subjects consuming at least 525 mg/day of calcium, the incidence rate ratios of fractures were 1.05 for fish eaters, 1.02 for vegetarians, and 1.00 for vegans.4 Mangels explains, “This study found that vegans had a higher risk of fractures than did other vegetarians or nonvegetarians. When only vegans with calcium intakes above the UK Estimated Average Requirement for calcium were included in the analysis, there was no difference between any of the groups in terms of fracture incidence.”
Virginia Messina, MPH, RD, coauthor of Never Too Late to Go Vegan: The Over-50 Guide to Adopting and Thriving on a Plant-Based Diet, says, “Bone health is a concern for vegans who have low intakes of calcium, protein, and vitamin D. As long as vegans are eating a healthful diet, however, there is no evidence that they are at greater risk for bone disease.”
Tucker agrees, but adds, “The reality is that many vegans do not have adequate intakes of these nutrients.”
Lessons From Around the World
Some experts point out that vegans’ bone risk may be related to avoiding dairy products, often associated with bone health. But incidence of hip fracture—the most serious consequence of osteoporosis—is highest in Sweden and North America worldwide, where dairy intake is prominent. Hip fracture rates are lower in Asia, where dairy intake is much lower.8 According to a scientific review, calcium intake is much lower in Asia and Africa, due to the very low intake of dairy products, yet the prevalence of osteoporosis is much lower in these countries than in the United States and Europe.9 About 75% of the world’s population loses their lactose enzymes after weaning, raising the question about whether dairy products are essential to bone health.
However, the bone discussion is much more complicated than dairy. Tucker explains that diets from regions, such as Asia, that don’t typically contain calcium from dairy often include small fish with bones and calcium-set tofu. “One may be able to get along with somewhat less calcium than recommended if other bone-building nutrients are adequate and in balance and in the environment of consistent weight-bearing exercise,” Tucker says.
Messina says, “Since these are ecological comparisons and often use hip fracture rates, which are affected by many factors, for comparison, I don’t think they tell us too much about diet and bone health. But it’s also clear that these populations have identified other good ways to meet calcium needs. Asian populations, for example, can get lots of calcium from soyfoods and the cruciferous greens that are common parts of their diets.”
Bone Myths Among Vegans
Compounding the risk is a steady source of myths among the vegan community. “Many vegans think that their lower protein intake protects bone health because older thinking was that protein caused calcium to be leached from bones,” Messina says. “We know now that protein is important for strong bones and that vegans aren’t protected by the more alkaline nature of their diets. Because of this misinformation, many vegans believe that calcium isn’t important and they may not strive to include adequate amounts in their diet. Some vegans also may believe that they’re getting enough vitamin D from sunlight, but it can be very difficult to get enough in certain climates.”
Matt Ruscigno, MPH, RD, a speaker and author with a private practice in Los Angeles specializing in plant-based nutrition, says, “There are strong feelings in the vegan community, with reason, about how the dairy industry may influence calcium recommendations. Often, vegans think they don’t need to meet calcium requirements because they’re avoiding animal protein, once thought to leach calcium from bones, but the research shows they still do.”
Other concerns involve a homespun trend that finds vegans making their own (unfortified) plant milks and avoiding fortified foods or supplements with the feeling that “they can get everything they need from their diet,” which Mangels finds concerning. Homemade and newly popular brands of plant milks may be very low in protein, calcium, and vitamin D, compared with fortified soymilks, which typically have protein, calcium, and vitamin D levels very similar to dairy milk.
Calcium
Considering the lack of dairy products in their diets, a big issue among vegans is calcium intake. The body carefully regulates calcium levels; if the concentration in the blood, muscles, or intercellular fluids is too low, the body takes calcium from the bones through resorption.
Recent research has created confusion over just how much calcium is needed, as well as the impact of supplementation. (Read “The Calcium Debate” in the January 2016 issue of Today’s Dietitian.) The 2011 Dietary Reference Intakes recommend a Recommended Dietary Allowance (RDA) of 1,000 mg for most adults aged 19 to 70, and 1,200 mg for women older than 50 and men older than 70.10 However, this recommendation isn’t embraced around the world. The UK Estimated Average Requirement suggests adults get 700 mg per day,11 and the World Health Organization recommends 400 to 500 mg of calcium to prevent osteoporosis in countries with a high fracture incidence.12 Throw into the mix that some studies have linked calcium supplements with an increased risk of cardiovascular disease in elderly adults. Some health organizations are critical of the current calcium RDA, as well as the number of dairy products the USDA suggests. For example, the Harvard’s Healthy Eating Plate doesn’t include dairy products as an essential component of a healthful diet.
So where does that leave dietitians when it comes to making calcium recommendations for vegans? Experts agree that for now it’s best to be cautious and stick with the current RDA, and keep in mind that many vegans aren’t meeting their calcium needs.
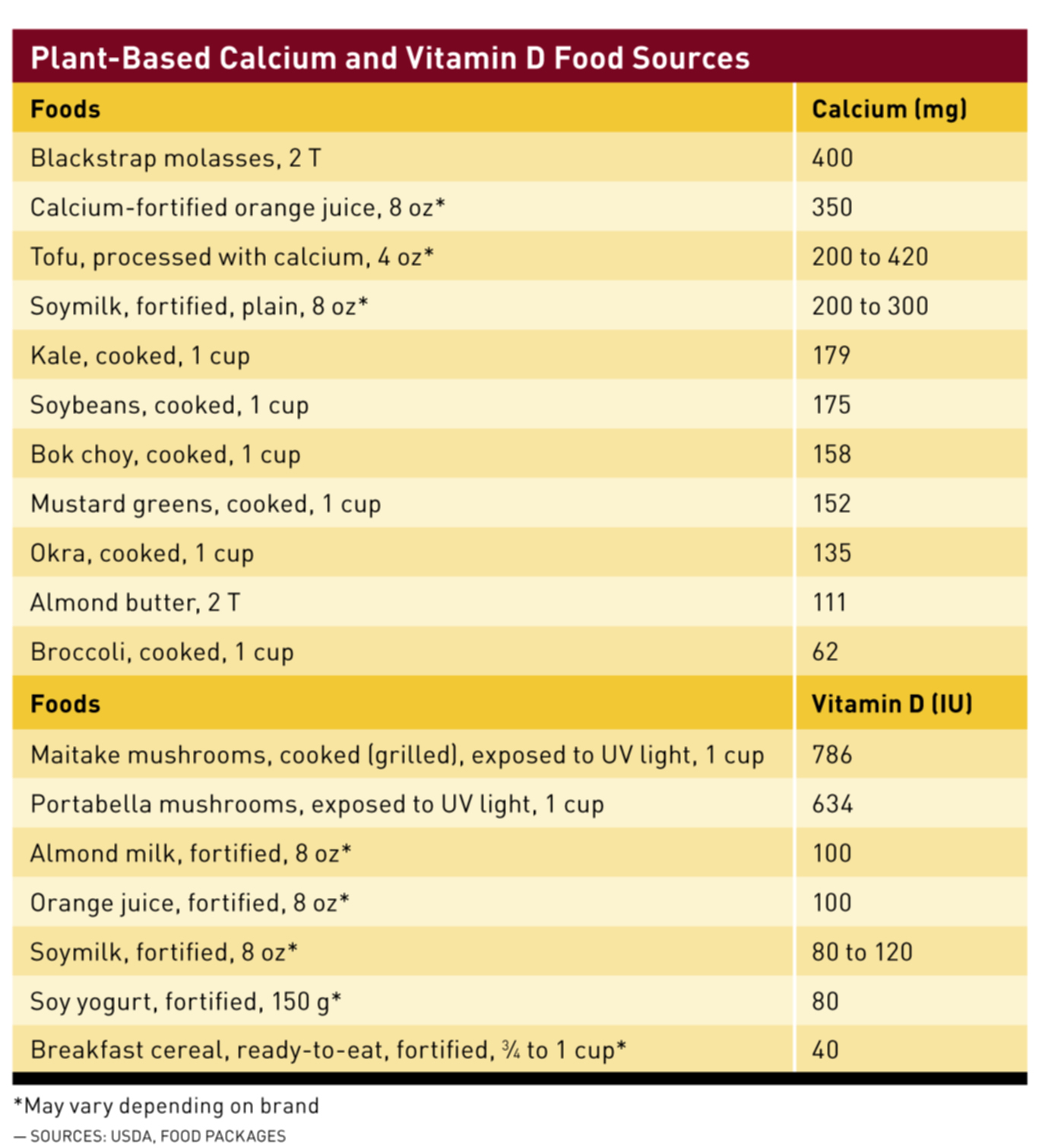
Where should calcium come from? This is another misunderstood area, according to Messina, who says, “Vegans should concentrate on foods with high absorption as their main sources of calcium. Bioavailability is excellent from cruciferous vegetables like turnip greens, collards, mustard greens, and kale. But it’s very poor from certain other greens, such as spinach, Swiss chard, and beet greens. It’s also good from soyfoods and fortified plant milks, but calcium is absorbed at much lower rates from other legumes, nuts, and seeds. If vegans are consuming large amounts of calcium-rich cruciferous vegetables they can probably get away with a little bit lower calcium intake since bioavailability from these vegetables is so high.”
And what about calcium supplements? “Ideally, we should get our calcium from foods. But for those who find it difficult to meet needs it’s okay to make up the difference with a low-dose supplement—about 300 mg per day,” Messina says.
Vitamin D
Vitamin D is required for calcium absorption, and the Dietary Reference Intakes recommends 600 IU of vitamin D daily for adults aged 19 to 70.10 While vitamin D is a shortfall nutrient for all Americans, it’s even more of a concern for vegans. The EPIC-Oxford study found that vegans had the lowest intake of vitamin D, compared with other diet patterns.13 Since the major dietary sources of vitamin D are fortified dairy products, fish, and egg yolks, it makes sense that vegans’ intake may be low. Vegan sources include fortified foods, such as plant milks, orange juice, and cereals; mushrooms exposed to light; sunlight exposure; and supplements.
Many experts recommend that vegans supplement the diet with vitamin D. “Vitamin D is critical. There are few food sources, and without fish or milk, it’s very low in a vegan diet. While 10 minutes a day with exposed skin in good sunlight is fine in the summer, during winter months supplements may be needed to obtain sufficient vitamin D,” Tucker says.
Protein
Protein also is key in bone health, despite an older theory that lower protein intake protected calcium in bones. In the Framingham Osteoporosis Study, elderly men and women with lower protein intake had increased bone loss, and higher intake of animal protein didn’t affect the skeleton adversely.14 According to Tucker, who was a researcher in this study, “The highest protein intakes were protective. Over the long term, there appears to be increased calcium absorption and increased bone building with higher protein.”
Does the type of protein vegans consume make a difference? Perhaps not, according to a 25-year study of wrist fracture risk among women, which compared meat and plant protein consumption. In this study of nearly 2,000 peri- and postmenopausal women, vegetarians who consumed the least vegetable protein were at the greatest risk of wrist fracture, but increasing levels of plant proteins decreased wrist fracture risk, with a 68% reduction in risk in the highest intake group. Among those with the lowest vegetable protein consumption, increasing meat intake decreased the risk of wrist fracture, with the highest consumption decreasing risk by 80%. The scientists concluded that higher consumption of protein-rich foods was associated with reduced wrist fracture, and the similarity in risk reduction with consumption of vegetable protein compared with animal protein suggests that adequate protein intake is attainable in a vegetarian diet.15
Many vegans rely on fortified soymilk to replace milk, thus providing rich sources of protein, calcium, and vitamin D. In a 2014 article on bone nutrients for vegan diets in The American Journal of Clinical Nutrition, Mangels reported that bone health often is associated with consumption of dairy products to provide bone health nutrients, yet plant-based sources also offer these nutrients.16 In the Adventist Health Study 2, scientists compared the bone effects of soymilk and dairy consumption among 337 postmenopausal women. At least one serving of soymilk per day was associated with improved bone health to a similar degree as dairy in vegetarian diets, leading the researchers to conclude it may be a useful replacement, possibly related to its protein and calcium content. The protein content of unfortified soymilk is 3.27 g/100 g compared with 3.15 g/100 g for whole milk; the calcium contents of unfortified and fortified soymilks are 25 mg/100 g and 123 mg/100 g, respectively, compared with a calcium content of 113 mg/100 g for whole milk.17
Alkaline vs Acid Diets
The potential bone impact of alkaline vs acid diets has merited a great deal of attention. The theory is that foods like meats, dairy, eggs, grains, and processed foods produce more acid, while foods like fruits, vegetables, and legumes produce more alkaline.
Some research has suggested that high acid diets cause calcium to be released from the bones. However, one recent study found that high acid diets with adequate calcium intake didn’t impact BMD.18 Another study of German vegans found that diet didn’t affect acid-base homeostasis (the body’s natural balance between acidity and alkalinity).19 A cross-sectional study of young adult vegetarians, vegans, and omnivores found that urinary pH was more alkaline among vegetarians and vegans, yet it was associated with BMD in omnivores only, and protein intake was associated with BMD only among vegan diets. The scientists concluded that plant-based diets aren’t detrimental to bone in young adults, and that diet prescriptions for bone health may vary among diet groups, including recommendations for increased fruit and vegetable intake for those with high meat intakes and increased plant protein intake for vegetarians.20
“While some research finds that a more acid diet could lead to increased osteoclatic activity and increased bone resorption, more recent research suggests that the serum pH change that occurs in response to an acid-generating diet is not large enough to lead to increased bone resorption,” Mangels says. “A vegan diet does contain foods that generate acid, such as soy products, corn, wheat, and rice. The potential acid-producing effect of these foods may be offset by a high fruit and vegetable intake, since they have an alkalizing effect.”
“The greater use of vegetables in a healthy vegan diet will usually help the acid/base balance, as opposed to a typical Western diet, and this does offer some advantage. We have found that fruit and vegetable intake is protective of bone mineral density,” Tucker says.
Hultin’s viewpoint is that the acid/alkaline theory discounts other important factors, including adequacy and absorption of vitamins and minerals. She says, “The acid or alkaline nature of a diet is not enough to ensure bones will build and maintain adequate strength over time without taking in adequate bone building minerals.”
Other Bone Nutrients
Research is shining the light on other bone-protective nutrients, including phosphorus, magnesium, zinc, copper, manganese, vitamin C, vitamin B12, vitamin K, and potassium, Mangels says.
Of particular interest is the impact of vitamin B12. Tucker explains that vitamin B12 is critical for DNA methylation and rebuilding of bone, and inadequacy has been related to fracture risk. “Vitamin B12 is only found to any extent in animal foods. This nutrient is very important for vegans and should be supplemented,” Tucker adds. In a study of German vegetarians, vegans, and omnivores, researchers found that low vitamin B12 status was related to increased bone turnover in vegetarian diet patterns, independent from vitamin D status.21
Growing research shows that omega-3 fatty acids have a role in bone metabolism, such as in calcium balance and osteoblast activity.22 Intake of omega-3 fatty acids can be a problem for vegans, according to Tucker, since intake comes mainly from fish. “Plant sources are limited, and include walnuts and flaxseeds, but the alpha-linolenic acid from these sources isn’t as efficient as the DHA/EPA from fish, so it’s difficult to get enough. There are new vegan supplements of DHA available from algae, but few studies have evaluated them,” Tucker says.
On the bright side, vegan diets are very high in whole grains, nuts, seeds, fruits, vegetables, and legumes, thus they’re rich in an array of bone-protective nutrients. “We have seen protective effects of vitamin C and beta-carotene from fruits and vegetables,” Tucker says. “The magnesium and potassium from these, as well as whole grains and nuts, are also protective. In addition to vitamins and minerals, a plant-based diet provides phytonutrients which are anti-inflammatory, and this is also beneficial to bones.”
And, it’s important to consider lifestyle factors that can impact bone health. “Vegans should pay close attention to other protective lifestyle factors, such as weight-bearing physical activity and maintaining an appropriate body weight,” Hultin says. “Studies have shown that vegans often maintain a lower body weight. Body stature and frame size can affect bone health in slighter folks, especially those who are underweight.”
Strategies for RDs
RDs have the perfect opportunity to provide vegans with the best advice on maintaining healthy bones, especially given the confusing information that’s so pervasive. Hultin says, “I think it is best for vegans to meet with a dietitian to ensure they are taking in adequate vitamins and minerals, assess risk factors on a personal basis, and discuss the appropriateness of supplementing. A dietitian can recommend labs or tests that need to be done, such as vitamin D blood labs or bone density scans, and discuss other risk factors such as ethnicity, family history, body weight, use of bone depleting medications, or history of smoking or eating disorders. A dietitian can suggest diet and lifestyle factors to support bone health in vegans.”
Messina says, “RDs need to be knowledgeable about vegan sources of well-absorbed calcium and vitamin D. Most supplements are not vegan, so it’s important to identify ones that are either vitamin D2 or the harder to find vegan D3. RDs should give vegans specific guidance on eating diets rich in legumes, calcium-rich foods, and a daily source of vitamin D.”
“Weight-bearing exercise is a very crucial part of bone health,” Ruscigno says, “and I recommend all of my clients make working out a part of their health plan.”
It’s important to recognize that the current body of research suggests that a vegan diet—as long as it is adequate—may not necessarily put clients at risk of osteoporosis. And that’s where dietitians come in: help your clients and patients make the most of their chosen eating pattern in order to maintain strong, healthy bones for years to come.
— Sharon Palmer, RDN, is the nutrition editor for Today’s Dietitian and author of Plant-Powered for Life and The Plant-Powered Diet. She blogs regularly at www.sharonpalmer.com.
References
1. Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2(6):285-289.
2. Melton LJ 3rd, Chrischilles EA, Cooper C, Lane AW, Riggs BL. Perspective: How many women have osteoporosis? J Bone Miner Res. 1992;7(9):1005-1010.
3. Ho-Pham LT, Nguyen ND, Nguyen TV. Effect of vegetarian diets on bone mineral density: a Bayesian meta-analysis. Am J Clin Nutr. 2009;90(4):943-950.
4. Appleby P, Roddam A, Allen N, Key T. Comparative fracture risk in vegetarians and nonvegetarians in EPIC-Oxford. Eur J Clin Nutr. 2007;61(12):1400-1406.
5. Ho-Pham LT, Nguyen PL, Le TT, et al. Veganism, bone mineral density, and body composition: a study in Buddhist nuns. Osteoporos Int. 2009;20(12):2087-2093.
6. Ambroszkiewicz J, Klemarczyk W, Gajewska J, Chełchowska M, Franek E, Laskowska-Klita T. The influence of vegan diet on bone mineral density and biochemical bone turnover markers. Pediatr Endocrinol Diabetes Metab. 2010;16(3):201-204.
7. Ambroszkiewicz J, Klemarczyk W, Gajewska J, Chełchowska M, Laskowska-Klita T. Serum concentration of biochemical bone turnover markers in vegetarian children. Adv Med Sci. 2007;52:279-282.
8. Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of hip fracture: worldwide geographic variation. Indian J Orthop. 2011;45(1):15-22.
9. Tsukahara N, Ezawa I. Calcium intake and osteoporosis in many countries. Clin Calcium. 2001;11(2):173-177.
10. Institute of Medicine Food and Nutrition Board. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press; 2011.
11. Michaëlsson K. Calcium supplements do not prevent fractures. BMJ. 2015;351:h4825.
12. World Health Organization. Diet, nutrition and the prevention of chronic diseases: recommendations for preventing osteoporosis. http://www.who.int/dietphysicalactivity/publications/trs916/en/gsfao_osteo.pdf?ua=1. Published 2003.
13. Crowe FL, Steur M, Allen NE, Appleby PN, Travis RC, Key TJ. Plasma concentrations of 25-hydroxyvitamin D in meat eaters, fish eaters, vegetarians and vegans: results from the EPIC-Oxford study. Public Health Nutr. 2011;14(2):340-346.
14. Hannan MT, Tucker KL, Dawson-Hughes B, Cupples LA, Felson DT, Kiel DP. Effect of dietary protein on bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res. 2000;15(12):2504-2512.
15. Thorpe DL, Knutsen SF, Beeson WL, Rajaram S, Fraser GE. Effects of meat consumption and vegetarian diet on risk of wrist fracture over 25 years in a cohort of peri- and postmenopausal women. Public Health Nutr. 2008;11(6):564-572.
16. Mangels AR. Bone nutrients for vegetarians. Am J Clin Nutr. 2014;100(Suppl 1):469S-475S.
17. Orlich MJ, Fraser GE. Vegetarian diets in the Adventist Health Study 2: a review of initial published findings. Am J Clin Nutr. 2014;100(1):353S-358S.
18. Mangano KM, Walsh SJ, Kenny AM, Insogna KL, Kerstetter JE. Dietary acid load is associated with lower bone mineral density in men with low intake of dietary calcium. J Bone Miner Res. 2014;29(2):500-506.
19. Ströhle A, Waldmann A, Koschizke J, Leitzmann C, Hahn A. Diet-dependent net endogenous acid load of vegan diets in relation to food groups and bone health-related nutrients: results from the German Vegan Study. Ann Nutr Metab. 2011;59(2-4):117-126.
20. Knurick JR, Johnston CS, Wherry SJ, Aguayo I. Comparison of correlates of bone mineral density in individuals adhering to lacto-ovo, vegan, or omnivore diets: a cross-sectional investigation. Nutrients. 2015;7(5):3416-3426.
21. Herrmann W, Obeid R, Schorr H, et al. Enhanced bone metabolism in vegetarians — the role of vitamin B12 deficiency. Clin Chem Lab Med. 2009;47(11):1381-1387.
22. Maggio M, Artoni A, Lauretani F, et al. The impact of omega-3 fatty acids on osteoporosis. Curr Pharm Des. 2009;15(36):4157-4164.


