Today’s Dietitian
Vol. 18 No. 1 P. 36
Here’s an overview of the conflicting research regarding the effectiveness and safety of current calcium intake recommendations and tips for advising clients.
While advocacy and health-policy making organizations cite evidence that calcium is necessary to build and maintain strong bones, a body of research continues to grow indicating this nutrient is ineffective when it comes to preventing fractures in older adults, and may, in fact, be dangerous at recommended levels. What accounts for such dramatically different conclusions? And what advice should nutrition professionals give their clients and patients going forward? Today’s Dietitian reviews the conflicting research and offers strategies to counsel clients and patients more effectively.
Critical Calcium
“Calcium is the most abundant and dominant mineral in the body,” says Andrea J. Singer, MD, FACP, CCD, director of women’s primary care and bone densitometry for the department of obstetrics and gynecology at MedStar Georgetown University Hospital and clinical director of the National Osteoporosis Foundation. “It’s important for skeletal health, as well as a whole host of other essential functions.” Without calcium there would be no nerve transmission, muscle contraction, cell signaling, blood clotting, constriction and relaxation of blood vessels, or secretion of hormones like insulin.1-3 “If there isn’t enough calcium coming in from the diet,” Singer says, “the body will pull calcium from the bones for all of these things that need to be done.”
The 2011 Dietary Reference Intakes for Calcium and Vitamin D from the Institute of Medicine (IOM) concluded that calcium plays a key cause-and-effect role in maintaining a healthy skeleton, and issued Recommended Dietary Allowances (RDAs) for all life stages over 1 year of age.4 The report recommends that most adults aged 19 to 70 get a total of 1,000 mg of calcium daily, and women older than 50 and men older than 70 aim for 1,200 mg of calcium per day.4 The 2015 Dietary Guidelines Advisory Committee (DGAC) concluded that many Americans don’t meet these recommendations, and declared calcium “a nutrient of public health concern for underconsumption.”3
While the IOM intends for RDAs to be met by eating a variety of foods as part of a regular diet, supplements often are seen as a way to ensure adequate calcium intake.5 “Many guidelines advise older people to get at least 1,000 to 1,200 mg per day of calcium to improve bone density and prevent fractures,” says Mark J. Bolland, PhD, an associate professor of medicine at the University of Auckland in New Zealand. “The average calcium intake in most countries is a lot less than these recommendations, and so many people take calcium supplements to increase their calcium intake. For example, in recent studies, more than 50% of older women in the USA took calcium supplements.”
Conflicting Conclusions
In September 2015, BMJ published a study by Bolland and colleagues questioning the effectiveness of America’s current calcium recommendations for protecting bone health. This meta-analysis of randomized controlled trials concluded there’s “weak and inconsistent” evidence that calcium supplements prevent fractures.6 According to Bolland, the lead study author, “In 26 clinical trials, calcium supplements have only small, inconsistent benefits in preventing fractures, with no effect on fractures seen in the highest-quality trials. In addition, in 59 randomized, controlled trials, we found that increasing calcium intake either from the diet or by taking calcium supplements led to similar, small, one-off increases in bone density of 1% to 2%. These increases do not build up over time and are too small to produce significant reductions in the chance of having a fracture.” Bolland recommends against increasing calcium intake to prevent fractures except in frail, institutionalized, elderly women with low dietary calcium intake and serum vitamin D levels.6 While this study is compelling, an October 2015 meta-analysis from the National Osteoporosis Foundation reached the opposite conclusion. This analysis by Weaver and colleagues concluded there’s a significant reduction in total fractures with calcium plus vitamin D supplementation, and that the use of calcium plus vitamin D supplements to reduce fracture risk is supported in both community-dwelling and institutionalized older adults.7
This inconsistency of data on the impact of supplemental calcium also is seen in studies on dietary calcium. While the IOM based its recommendations on a body of data supporting calcium’s role in bone health, Bolland asserts there’s “no clinical trial evidence that increasing calcium intake from dietary sources prevents fractures. Furthermore, in our meta-analysis the level of dietary calcium intake was not associated with the risk of having a fracture in 44 cohort studies.”
In addition to these concerns about the effectiveness of calcium on fracture risk, studies also have raised questions about the safety of the IOM recommendations. Bolland and others have reported that calcium supplements can cause kidney stones, hypercalcemia, acute gastrointestinal symptoms leading to hospitalization, and increased cardiovascular disease (CVD) risk.8 According to the American Society for Bone and Mineral Research, one randomized controlled trial, one prospective cohort study, and two meta-analyses suggest an increased risk of CVD in elderly adults taking calcium supplements; however, one particular high-quality meta-analysis, one randomized controlled trial, and several cohort studies found no evidence of such an association.9
“Many studies have looked carefully at the issue of calcium increasing CVD risk and are just not seeing a link,” says Bess Dawson-Hughes, MD, director of the Bone Metabolism Laboratory at the Jean Mayer USDA Human Nutrition Research Center on Aging at Tufts University.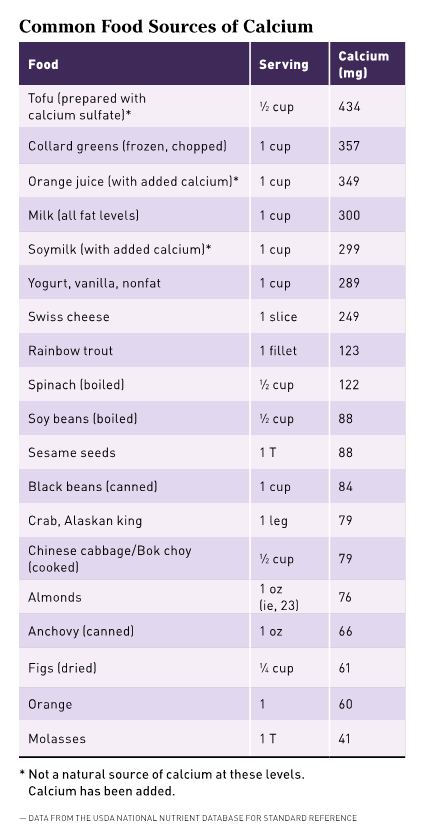
Causes of the Confusion
“There’s a huge body of literature about the benefits and risks of calcium, much of which is inconsistent,” Singer says. “This has led to a lot of confusion and controversy.”
Dawson-Hughes cautions against using the inconsistency of the data to infer that calcium has little effect on bone density or fracture risk. Instead of relying on consistency as an indicator of effectiveness, Dawson-Hughes says, “We need to look at the sources of inconsistency and see what we can learn from them.”
Singer says, “It’s important to look at the literature out there carefully and evaluate it.”
First, determining the type of study that was conducted is important. “Epidemiologic studies do not show cause and effect; they only find correlations that could be areas for future study,” says Isabel Maples, MEd, RDN, a spokesperson for the Academy of Nutrition and Dietetics and a former National Dairy Council spokesperson. “Even meta-analyses can potentially be misleading, especially if they don’t utilize all available studies. Sometimes inconsistent or inaccurate results can come from not having enough studies to draw from, or from trying to compare studies that may have looked at an issue in different ways.” In a September 2015 BMJ editorial, Karl Michaëlsson stated that meta-analyses on dietary calcium often use evidence from studies that aren’t similar enough to be pooled together. Studies used in current meta-analyses differ in sample size, the quality of the dietary assessments used, how adjustments were made for energy intake, how fractures were reported (self-report vs identification from records), and selection of variables examined, Michaëlsson wrote.10
In calcium studies, the amount of calcium in a participant’s prestudy diet is one factor that can complicate results. “Individuals vary in baseline calcium intake levels, and those levels are often not accurately assessed or not assessed at all,” Singer says. “That fact alone can make a big difference in the response to calcium supplements or dietary calcium given, and therefore a big difference in study outcomes.” Mixing data from different populations also can affect outcomes. “Meta-analyses might compare studies done in healthy populations, at-risk populations, and those who have osteoporosis or fractures already,” Singer says. “These are very different populations likely to have different calcium needs and/or different responses to increased calcium intake.” She recommends looking at studies individually to see exactly who and what was studied. “Look at the data being analyzed and consider: Is this the population we are interested in?” Singer says. “People with osteoporosis or who already had fractures are a very different population than healthy individuals over 50. The risk-benefit analysis ratios are different.”
In addition to the type of study and the differences in populations, the quality of the study also is important. According to one analysis, flaws in study design or execution, such as the inclusion of people who already get enough calcium, high dropout rates, and poor compliance, may make it impossible to determine not only if calcium supplements reduce fracture risk, but also if calcium deficiency increases fracture rates.11
Data analysis is another point that must be considered. “Some of the studies being used to claim calcium supplements increase heart attack risk weren’t designed to measure that outcome, and there was no verification,” Dawson-Hughes says.
Another possible factor confounding the data on the effectiveness and safety of dietary and supplemental calcium is the fact that calcium doesn’t act alone on the skeleton. The interplay between vitamin D and calcium often is discussed, but many other nutrients are involved in calcium balance. According to the World Health Organization, a case can be made based on biochemical and metabolic evidence that zinc, copper, manganese, boron, vitamin A, vitamin C, vitamin K, the B vitamins, potassium, and sodium all may be involved in long-term bone heath and the prevention of osteoporosis.12 This means that the overall diet and nutrition status (and even genetic tendencies) of the study participants could be influencing the impact of calcium intake. Moreover, since physical activity improves bone health, the varying activity levels of study participants also could affect outcomes.13 For all of these reasons, it’s difficult to perform a true placebo-controlled, randomized trial of a single nutrient.14
Being aware of potential flaws and confounding factors in individual studies will help to explain inconsistencies, but seeing the big picture is valuable as well. “It’s important for clinicians to look at the whole body of research before drawing conclusions, because sometimes it’s hard to tease out the different factors involved in one or two studies,” Maples says.
Clinical Implications
While the data are clearly inconsistent, there are certain points on which almost everyone agrees: Calcium is important for skeletal health; and calcium and vitamin D supplementation reduce fracture risk in frail, elderly women living in institutions.8
“The National Osteoporosis Foundation, the Institute of Medicine, and the Food and Drug Administration have all come out with guidelines and recommendations saying that calcium and vitamin D are clearly important for skeletal and other health,” Singer says. But how these recommendations are being implemented is shifting, with less emphasis being placed on calcium supplements and more on food sources. “The bottom line is that food trumps supplements,” Singer says. “In other words, dietary sources are preferred in terms of calcium intake. When someone is unable to get enough through diet, then supplements should be used to make up the shortfall.”
Bolland doesn’t think this shift is the answer. “Recent concerns about the safety of calcium supplements have led experts to recommend increasing calcium intake through food rather than by taking supplements,” he says, “even though the effect of increasing dietary calcium intake on bone health has not been clearly established.”
Even if Bolland is correct, getting calcium from food can improve health in other ways. “Nearly three-quarters (72%) of calcium in the American diet comes from dairy foods,” Maples says. “Dairy is also the No. 1 source of potassium in the American diet.” (Potassium is another nutrient identified by the 2015 DGAC as an underconsumed nutrient of concern.)3 Shifting the focus to food first has other benefits as well. Since bone health is impacted by more than just calcium, a well-balanced, healthful diet ensures intake of all the nutrients necessary for a strong skeleton. Calcium is less bioavailable in plant sources than animal sources, but including plant-based sources of calcium such as dark leafy greens, broccoli, beans, tofu, and almonds increases calcium intake while adding to the healthfulness of the overall diet.3 “With calcium and vitamin D supplements, you’re getting just those nutrients,” Maples says. “From foods you get nutrients like potassium, magnesium, fiber, and phytochemicals that also play an important role in health.”
While others believe, as Bolland says, “There’s actually no evidence of an important relationship between calcium intake and bone health in older people, and these dietary recommendations should be revised,” most advocacy organizations and health policymakers are standing by the IOM recommendations, for now.
“The studies are numerous, and at this time it still remains inconclusive and inconsistent, so we don’t have data to change the recommendations,” Singer says.
“People should strive to meet the calcium levels recommended by the IOM, using food sources to the greatest extent possible,” Dawson-Hughes says. “Those who cannot meet requirements using food can take supplements to get there. Getting more than the recommended levels is not a good idea, though,” since there’s the possibility of increased risk of kidney stones and other potential adverse effects.
The mixed messages on calcium recommendations are confusing to clients and clinicians alike. “It’s very frustrating for clinicians to have to go through this with every osteoporosis patient they see,” Dawson-Hughes says. Nutrition professionals should keep a close analytical eye on emerging research and continue to encourage clients to be physically active and include dairy, dairy substitutes, dark leafy greens, and other calcium sources like almonds and beans as part of a healthful, well-balanced diet.
— Judith C. Thalheimer, RD, LDN, is a freelance nutrition writer, a community educator, and the principal of JTRD Nutrition Education Services.
References
1. Linus Pauling Institiute. Calcium dietary supplement fact sheet. National Institutes of Health Office of Dietary Supplements website. https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/. Updated November 21, 2013.
2. Micronutrient Information Center. Oregon State University website. http://lpi.oregonstate.edu/mic
3. US Department of Agriculture, US Department of Health and Human Services. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. http://www.health.gov/dietaryguidelines/2015-scientific-report/PDFs/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf. Published February 2015.
4. Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press; 2011.
5. National Research Council (US) Subcommittee on the Tenth Edition of the Recommended Dietary Allowances. Recommended Dietary Allowances: 10th Edition. Washington, DC: National Academies Press (US); 1989.
6. Bolland MJ, Leung W, Tai V, et al. Calcium intake and risk of fracture: systematic review. BMJ. 2015;351:h4580.
7. Weaver CM, Alexander DD, Boushey CJ, et al. Calcium plus vitamin D supplementation and risk of fractures: an updated meta-analysis from the National Osteoporosis Foundation [published online October 28, 2015]. Osteoporos Int. doi: 10.1007/s00198-015-3386-5.
8. Bolland MJ, Grey A, Reid IR. Should we prescribe calcium or vitamin D supplements to treat or prevent osteoporosis? Climacteric. 2015;18(Suppl 2):22-31.
9. Latest research on osteoporosis, bone fractures in men, calcium and vitamin D supplements and new treatments for bone disease released at ASBMR 2013 Annual Meeting. American Society for Bone and Mineral Research website. http://www.asbmr.org/About/PressReleases/Detail.aspx?cid=285ee54c-d6c1-4940-930a-4f9e87176a7c. Updated October 14, 2013.
10. Michaëlsson K. Calcium supplements do not prevent fractures. BMJ. 2015;351:h4825.
11. Seeman E. Evidence that calcium supplements reduce fracture risk is lacking. Clin J Am Soc Nephrol. 2010;5(Suppl 1):S3-S11.
12. World Health Organization. Joint WHO/FAO expert consultation on diet, nutrition and the prevention of chronic diseases: recommendations for preventing osteoporosis. WHO Technical Report Series, No. 916 (TRS 916).
http://www.who.int/dietphysicalactivity/publications/trs916/en/gsfao_osteo.pdf. Published April 23, 2003.
13. Exercise for strong bones. National Osteoporosis Foundation website. http://nof.org/exercise
14. Khan B, Nowson CA, Daly RM, et al. Higher dietary calcium intakes are associated with reduced risks of fractures, cardiovascular events, and mortality: a prospective cohort study of older men and women. J Bone Miner Res. 2015;30(10):1758-1766.


