Today’s Dietitian
Vol. 19, No. 10, P. 36
Emerging research shows that nutraceuticals plus diet and lifestyle changes may treat common mental illnesses.
The prevention and treatment of mental health conditions is a critical issue in health care today. Depression- and anxiety-related disorders are among the most common mental health illnesses in the United States and around the globe, with increasing rates of disability due to these conditions.1 The World Health Organization estimates that by 2020, depression will rank second among the top 10 burdens of disease worldwide.2 Identification of safe and effective treatments is warranted, and a growing body of research provides evidence that food and nutrition therapies are some of the most promising interventions for this modern-day pandemic.
Integrative and Functional Nutrition Therapy
The concept of chemical imbalances and the role of neurotransmitters, such as serotonin, underlying the etiology of mood disorders has expanded recently with newer technologies contributing to a better understanding of brain metabolism. This emerging integrative and functional nutrition model of psychiatric medicine is rooted in systems biology that seeks to unravel the genetic, epigenetic, and metabolic mechanisms related to inflammation, the microbiota-gut-brain axis, oxidative stress/mitochondrial dysfunction, and nutrient deficits.3
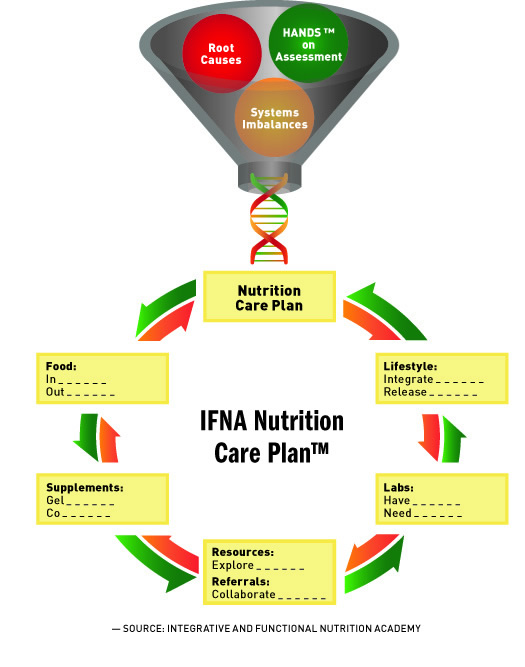
The biological basis of mental illness lends itself to nutrition and lifestyle measures that enhance neuroplasticity and brain resiliency.4 RDs can assess these physiological areas to identify imbalances that can be modified through diet and supplements tailored to the individual and design a personalized intervention and treatment plan. Core elements of an integrative and functional nutrition care plan include recommendations in five key areas: food, supplements, lifestyle, labs, and resources/referrals.5 (See figure, Integrative and Functional Nutrition Academy Care Plan.)
Nutrition Assessment of Physiological Inflammation
Inflammation is an essential physiological process that supports healing in the event of an injury, infection, toxin, or other trauma. Normally, it’s a short-lived, regenerative process. However, if it’s sustained beyond what’s needed for the temporary repair of bodily tissues and shifts to a chronic state, the brain and nervous system can be negatively impacted and mood disorders can result. A bidirectional relationship ensues, with inflammation fueling the flames of depression and depression priming inflammatory cytokine responses to stressors and pathogens.6
Diet is one of the major epigenetic influences on inflammation. Several dietary components that can fuel or cool inflammatory processes have been recognized.7 Analysis of a client’s food records to identify proinflammatory foods and dietary patterns that include excess calories, refined sugars, and low omega-3 fatty acid intake is central to nutrition assessment for mood disorders. Dietitians also should consider the possibility that intolerance to ingredients such as gluten, casein, or other food chemicals are contributing to the inflammatory burden.
Serum biomarkers to evaluate for inflammation include C-reactive protein, homocysteine, tumor necrosis factor alpha, and interleukin-6.8,9 Uncovering the cause of the inflammation is important so dietitians can tailor appropriate treatment. A place to begin investigating is the patient’s gastrointestinal tract because disruptions in the digestive system and microbiome can contribute to neuroinflammation.
Microbiota-Brain-Gut Axis
Groundbreaking medical theories and practices in the 19th and early 20th centuries linked microbes to mood disorders.10 In the 1825 classic The Physiology of Taste, Jean-Anthelme Brillat-Savarin wrote: “Digestion, of all the bodily functions, is the one which exercises the greatest influence on the mental state of the individual.”11 Modifying diet, administering beneficial microbes such as Lactobacillus acidophilus in milk products, correcting dysbiosis, and ridding the body of “intestinal toxemia” were common medical interventions for individuals suffering from “melancholia” and “the neuroses.”12
Despite their promise and potential for healing illnesses of the nervous system, with the dawn of the antibiotic era, microbial-centric therapies were discarded as medical mythology. Pathogen eradication with antibiotics became the norm and dominated 20th-century medicine along with a focus on psychopharmacology as chemical imbalance-based theories of depression gained ground in the 1950s and 1960s.12 During this time, René Dubos, PhD, and other highly respected microbiologists again proposed that the noxious components produced by intestinal flora impacted one’s physical and mental well-being. However, theories connecting intestinal barrier integrity and microbial toxins with mental health status weren’t in accordance with the prevailing scientific logic of the time. Consequently, drug treatments remained the mainstay of psychiatry.
Nonetheless, research on the microbiome has exploded in recent years due to sophisticated technologies that are unraveling the gut-brain-microbial relationship. This has fueled a renaissance of interest in some of the early microbe-based theories on the role of dysbiosis, increased intestinal permeability (ie, leaky gut), and endotoxemia in mental health disorders.12
Science is revealing that our microbes multitask, performing vital functions that ultimately contribute to the state of our mind, moods, and more. The microbiota-brain-gut-axis is an integral part of the digestive tract’s communication system; imbalances in gut bacteria change neurotransmitter function and alter immune response, resulting in associated inflammatory activation.13 In susceptible individuals, it’s possible that a leaky gut may set the stage for a leaky blood-brain barrier with mind-altering consequences.14 In addition, a poorly nourished microbiome due to a highly processed, low-fiber diet can result in decreased production of short-chain fatty acids such as butyrate, which has been shown to be neuroprotective.15
What this means for the RD is that assessing a patient’s gut health is critical to evaluating their mental health. In working with clients with mood disorders, nutrition assessments should include key questions that reflect digestion, absorption, and elimination functions. It’s important to inquire about underlying causes of gut dysfunction such as poor diet, medication use (eg, antibiotics, nonsteroidal anti-inflammatory medications, proton pump inhibitors, antacids, etc), an excessively clean and hygienic environment, psychological stress, and environmental toxins. Early life events such as C-section birth, formula feeding, childhood adversity, and food allergies also are potential causative factors.13
Understanding how to interpret both conventional and functional laboratory testing that provides clues regarding the need for nutrition therapy to restore the microbiota-gut-brain axis is essential for RDs in practice. These tests may include a stool analysis, breath test, nutrigenetic data (eg, celiac disease markers), and urine organic acids, all of which, in the author’s experience in 20-plus years of practice, can provide information on gut metabolites that impact neurotransmission and immune activation.13
Oxidative Stress
Moreover, an association between mental disorders and markers of oxidative stress has been reported in the literature. Oxidative stress, like inflammation, is unavoidable, as both are physiological processes of normal metabolism and, when functioning in balance, help maintain health. A disturbance in the balance of free radicals and reactive oxygen and nitrogen species can lead to cellular and organ damage from oxidative destruction of lipids, proteins, DNA, and RNA. Free radical production fuels the flame of inflammatory processes and assaults mitochondria, the cellular structures responsible for generating the majority of energy utilized by the brain to carry out essential functions. When mitochondria are injured by oxidative stress because the body’s antioxidant defense mechanisms are overwhelmed, the brain and nervous system are negatively impacted. This surplus of free radicals on board can manifest in somatic complaints such as fatigue, neuropsychiatric symptoms, and mood disorders.3
Root causes of oxidative stress, including a nutrient-poor diet, chronic stress, heavy metal burden, smoking, excess alcohol intake, and other lifestyle factors, should be explored. RDs also should assess their clients’ diets for food sources of nutrient antioxidants such as vitamin C, vitamin E, carotenoids, trace minerals (eg, zinc, manganese, selenium), and flavonoids. In addition, detoxification genetic polymorphisms (eg, CYP1A1, GSTM1, NQ01) and biomarker evaluation of oxidative stress may be considered, which include blood or urine indices such as lipid peroxides, superoxide dismutase, F2 isoprostanes, and 8-OH deoxyguanosine.16
Dietary Patterns and Nutrient Deficits
In addition to exploring markers of oxidative stress, RDs also should evaluate clients’ dietary patterns and possible nutrient deficiencies, as the brain is an organ dependent on a constant supply of nutrients. There’s clear evidence that dietary patterns and specific nutrients are vital to the mitigation of inflammation, oxidative stress/mitochondrial dysfunction, and gut dysbiosis.3 Nutrients also are necessary to support methylation, neurobiological networks, and hormone signaling pathways that modulate mood, appetite, sleep, neurogenesis, and cognitive function.16 Several metabolic actors including insulin, GABA (gamma-Aminobutyric acid), brain-derived neurotrophic factor (BDNF), and other gut hormones play roles in stress-related and affective disorders.17
Metabolic syndrome, characterized by higher levels of glucose, total and LDL cholesterol, BMI, abdominal obesity, and low HDL cholesterol, has been associated with a higher prevalence of depression compared with those without the condition. A bidirectional relationship of metabolic syndrome and depression exists, and there has been discussion of classifying depression as “metabolic syndrome type II.”18 Hyperglycemia contributes to elevation of advanced glycation end products, pro-oxidant, cytotoxic substances that induce inflammation.19
Thyroid pathologies such as hypothyroidism, “thyro-stress,” and Hashimoto’s thyroiditis also have been linked to an increased predisposition toward anxiety and depression and shouldn’t be overlooked.20 A complete thyroid profile is recommended to determine whether an imbalance exists, and, if so, corrective measures should be taken.
Several studies support the relationship between a Western-style dietary pattern and increased prevalence of depression. A “failure in the food system” post-WWII with dependence on intensified agricultural methods and other environmentally destructive practices has been proposed to be at the root of the rise in mood disorders, with the surge in mental illness metaphorically described as a “hidden hunger.”21 Nutritional insults that deprive the brain of the nourishment it needs include an energy-dense, highly processed food diet, high glycemic load, and proinflammatory fats (eg, high ratio omega-6s:omega-3s). A noteworthy lack of dietary fiber is another serious Westernized dietary shortcoming. Fiber is the quintessential substance needed to nourish the gut microbiota, resulting in subsequent production of short-chain fatty acids such as butyrate, which benefits the brain.15 In addition, there’s a possibility that food components such as gluten, casein, or food chemicals to which a client might be intolerant are driving inflammation, disrupting intestinal barrier function, and igniting immune activation. In cases of food sensitivities, it may be that what’s eliminated from the diet is as essential in improving psychological health as what’s included.
A growing evidence base confirms that diet quality is at the core of psychological and emotional well-being. Systematic reviews and meta-analyses across genders, age groups, cultures, and countries endorse the adage that food is medicine for mind and mood. A variety of healthy plant-based diets from around the globe in the Mediterranean region, Norway, Japan, Australia, China, and the United Kingdom share common characteristics that support mental health and have been inversely associated with depression.22 Compatible elements of these diets include an abundance of vegetables, along with fish, legumes, fruits, nuts, and whole grains. Extra virgin olive oil, rich in phenolic compounds, is a mainstay ingredient in the Mediterranean dietary pattern, while soybeans and green tea are predominant elements in the Asian dietary guidelines. Complex phytochemicals from deeply colored vegetables, fruits, herbs, spices, cocoa, and seaweeds play critical roles as anti-inflammatory dietary agents, antioxidant cellular bodyguards, and BDNF manufacturers.
The SMILES trial (Supporting the Modification of Lifestyle In Lowered Emotional States) was the first randomized controlled trial to investigate the efficacy of a 12-week dietary intervention in the treatment of major depressive disorder.23 Researchers designed a modified Mediterranean diet based on the Australian Dietary Guidelines and the Dietary Guidelines for Adults in Greece. However, in contrast with a traditional Mediterranean diet, it included moderate consumption of red meat and dairy. Participants in the intervention group received seven dietary coaching sessions from a dietitian, while the control group received social “befriending” support. Results were significant and demonstrated that dietary improvement is a viable treatment strategy for treating major depression despite the physical and socioeconomic challenges patients with mental illness often encounter.24
Evidence from these studies is intriguing and sets the stage for larger clinical trials necessary to elucidate the mechanisms linking meals to mood. Many questions remain, including the impact of vegetarian and vegan diets, as some preliminary studies report better mood in vegetarians than in omnivores.17 This may be due to the reduction in trimethylamine oxide, a compound in the urine linked to cardiovascular disease, although this remains to be further investigated in omnivores consuming a healthful diet based on whole foods.13
Specific nutrients act as spark plugs in neurobiological pathways, performing vital functions for the brain and other organ systems. Deficiencies in vitamins, minerals, amino acids, and omega-3 fatty acids are associated with a higher prevalence of mood disorders.17,21 For example, zinc and magnesium are involved in NMDA (N-methyl-D-aspartate) receptor signaling, while folate, vitamin B12, vitamin B6, and riboflavin are essential cofactors for the synthesis of neurotransmitters.13,17 Accumulating evidence highlights the importance of vitamin D in mental health, with the suggestion that it may act to reduce increased neuronal levels of Ca2+ driving the depression.25
In addition to dietary intake, the intestinal microbiota produce and facilitate the supply of a variety of vitamins including biotin; vitamins B12, B6, B3, and B5; folate; vitamin D; and vitamin K.13 Thus, gut microbiota also influence nutrient availability and neuronal integrity. The RD must evaluate possible drug-induced nutrient deficiencies resulting from psychopharmacologic agents (eg, calcium intake due to selective serotonin reuptake inhibitors).26 Both conventional and functional laboratory tests can identify nutrient shortfalls and may include methylation genetic polymorphisms (eg, MTHFR, CBS, COMT), complete blood count, iron profile, and red blood cell vitamin, mineral, and fatty acid levels.
Dietary Supplements
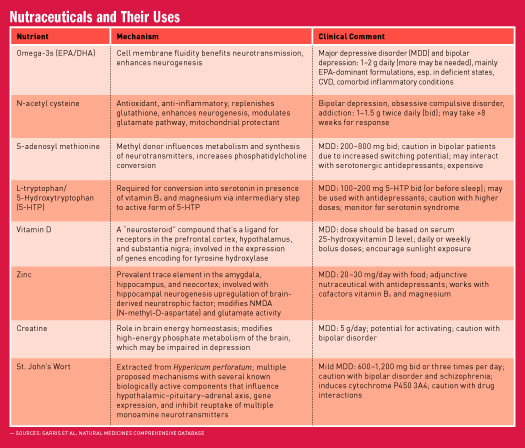
There’s a growing appreciation that in addition to dietary modification, nutraceutical supplementation has great potential in the treatment and management of mental health disorders.27 The International Society for Nutritional Psychiatry Research recommends that nutrition and nutraceuticals should be considered mainstream elements of psychiatric practice.28 Both single-nutrient and multinutrient formulas and probiotics have been studied. Kaplan and colleagues say that “a few hundred dollars of minerals and vitamins may be a significant savings relative to the costs of psychiatric treatment and the social costs of family distress … and treating with a combination of probiotics (either through dietary means, such as yogurts or fermented foods, or with formulated probiotic supplements alongside micronutrients may have an advantage of ensuring that nutrient absorption is maximized.”3 The integrative and functional RD can bring the needed expertise in evidence-based dietary supplementation to the nutritional psychiatry team. (See table on page 39 for a synopsis of some supplements for clinical consideration as adjuncts to dietary enhancement.)29
Lifestyle
Mind-body modalities when used with nutrition and conventional treatments for mood disorders have had promising results. These interventions may include yoga, tai chi, qigong, meditation, mindfulness, breath regulation techniques, and the relaxation response.30,31 One hypothesis is that mind-body interventions reverse expression of genes involved in inflammatory processes activated by stress.32
Physical activity has been shown to exert multiple physiological benefits in major depressive disorder, including increasing BDNF.33 Whether it’s walking, swimming, bicycling, dancing, or some other enjoyable activity, an exercise prescription is a vital component of a mood-boosting care plan. Robust evidence exists for the positive effects of nature and gardening on health with reductions in anxiety and depression, gains in quality of life, and renewed sense of community.34 Circadian rhythm alignment with high-quality sleep is another lifestyle factor that’s gaining ground in physical and mental health.35
RDs bring unique knowledge and skills to the nutritional psychiatry team. It’s an exciting time ripe with promise and possibilities that by applying an integrative and functional lens in clinical practice, those suffering from anxiety, depression, and other mental health problems can discover hope and healing through nutritional therapies.
— Kathie Madonna Swift, MS, RDN, LDN, FAND, is the cofounder of the Integrative and Functional Nutrition Academy, an online functional nutrition training program, and author of the books The Swift Diet and The Inside Tract. Connect with her at kathieswift.com or IFNAcademy.com.
References
1. Mental health by the numbers. National Alliance on Mental Health website. http://www.nami.org/Learn-More/Mental-Health-By-the-Numbers. Accessed August 1, 2017.
2. World Health Organization. Mental health: a call for action by world health ministers. http://www.who.int/mental_health/advocacy/en/Call_for_Action_MoH_Intro.pdf. Published 2001. Accessed August 1, 2017.
3. Kaplan BJ, Rucklidge JJ, Romijn A, McLeod K. The emerging field of nutritional mental health: inflammation the microbiome, oxidative stress, and mitochondrial function. Clin Psychol Sci. 2015;3(6):1-17.
4. Phillips C. Lifestyle modulators of neuroplasticity: how physical activity, mental engagement and diet promote cognitive health during aging. Neural Plast. 2017;2017:3589271.
5. Integrative and functional nutrition care plan. Integrative and Functional Nutrition Academy website. https://www.ifnacademy.com/topic/my-clinical-toolkit/. Accessed August 1, 2017.
6. Kiecolt-Glaser JK, Derry HM, Fagundes CP. Inflammation: depression fans the flames and feasts on the heat. Am J Psychiatry. 2015;172(11):1075-1091.
7. Giugliano D, Ceriello A, Esposito K. The effects of diet on inflammation: emphasis on the metabolic syndrome. J Am Coll Cardiol. 2006;48(4);677-685.
8. Tabung FK, Smith-Warner SA, Chavarro JE, et al. Development and validation of an empirical dietary inflammatory index. J Nutr. 2016;146(8):1560-1570.
9. Tabung FK, Smith-Warner SA, Chavarro JE, et al. An empirical dietary inflammatory pattern score enhances prediction of circulating inflammatory biomarkers in adults. J Nutr. 2017;147(8):1567-1577.
10. Logan AC, Jacka FN, Craig JM, Prescott SL. The microbiome and mental health: looking back, moving forward with lessons from allergic disease. Clin Psychopharmacol Neurosci. 2016;14(2):131-147.
11. Brillat-Savarin JA. The Physiology of Taste. New York, NY: Penguin Books; 2011.
12. Bested AC, Logan AC, Selhub EM. Intestinal microbiota, probiotics and mental health: from Metchnikoff to modern advances: part 1 — autointoxication revisited. Gut Pathog. 2013;5(1):5.
13. Sandhu KV, Sheervin E, Schellekens H, Stanton C, Dinan TG, Cryan JF. Feeding the microbiota-gut-brain-axis: diet, microbiome, and neuropsychiatry. Transl Res. 2017;179:223-244.
14. Shalev H, Serlin Y Friedman A. Breaching the blood-brain barrier as a gate to psychiatric disorder. Cardiovasc Psychiatry Neurol. 2009;2009:278531.
15. Bourassa MW, Alim I, Bultman SJ, Ratan RR. Butyrate, neuroepigenetics and the gut microbiome: can a high fiber diet improve brain health? Neurosci Lett. 2016;625:56-63.
16. Hodges RE, Minich DM. Modulation of metabolic detoxification pathways using foods and food-derived components: a scientific review with clinical application. J Nutr Metab. 2015;2015:760689.
17. Lang UE, Beglinger C, Schweinfurth N, Walter M, Borgwardt S. Nutritional aspects of depression. Cell Physiol Biochem. 2015;37(3):1029-1043.
18. McIntyre RS, SOczynska JK, Konarski JZ, et al. Should depressive syndromes be reclassified as ‘metabolic syndrome type II’? Ann Clin Psychiatry. 2007;19(4):257-264.
19. Vlassara H, Uribarri J. Advanced glycation end products (AGE) and diabetes: cause, effect, or both? Curr Diab Rep. 2014;14(1):453.
20. Kalra S, Verma K, Balhara YPS. Thyro-stress. Indian J Endocinol Metab. 2017;21(4):632-663.
21. Crawford MA. Non-communicable diseases, mental ill-health: is it a failure of the food system? Nutr Health. 2013;22(3-4):171-179.
22. Jacka FN. Nutritional psychiatry: where to next? EBioMedicine. 2017;17:24-29.
23. O’Neil A, Berk M, Itsiopoulos C, et al. A randomised, controlled trial of a dietary intervention for adults with major depression (the ‘SMILES’ trial): study protocol. BMC Psychiatry. 2013;13:114.
24. Jacka F, O’Neill A, Opie R, et al. A randomized controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Medicine. 2017;15:23.
25. Berridge MJ. Vitamin D and depression: cellular and regulatory mechanisms. Pharmacol Rev. 2017;69(2):80-92.
26. Rao TS, Asha MR, Ramesh BN, Rao KS. Understanding nutrition, depression and mental illness. Indian J Psychiatry. 2008;50(2):77-82.
27. Lakhan SE, Vieira KF. Nutritional therapies for mental disorders. Nutr J. 2008;7:2.
28. Sarris J, Logan AC, Akbaraly TN, et al. International Society for Nutritional Psychiatry Research consensus position statement: nutritional medicine in modern psychiatry. World Psychiatry. 2015;14(3):370-371.
29. Sarris J. Clinical use of nutraceuticals in the adjunctive treatment of depression in mood disorders. Australas Psychiatry. 2017;25(4):369-372.
30. Payne P, Crane-Godreau MA. Meditative movement for depression and anxiety. Front Psychiatry. 2013;4:71.
31. Chang C, Tsai G, Hsieh CJ. Psychological, immunological and physiological effects of a Laughing Qigong Program (LQP) on adolescents. Complement Ther Med. 2013;21(6):660-668.
32. Buric I, Farias M, Jong J, Mee C, Brazil IA. What is the molecular signature of mind-body interventions? A systematic review of gene expression changes induced by meditation and related practices. Front Immunol. 2017;8:670.
33. Kerling A, Kück M, Tegtbur U, et al. Exercise increases serum brain-derived neurotrophic factor in patients with major depressive disorder. J Affect Disord. 2017;215:152-155.
34. Soga M, Gaston KJ, Yamaura Y. Gardening is beneficial for health: a meta-analysis. Prev Med Rep. 2017;5:92-99.
35. Abbott SM, Videnovic A. Chronic sleep disturbance and neural injury: links to neurodegenerative disease. Nat Sci Sleep. 2016;8:55-61.


